What Are These Umbilicated, Pruritic Papules on the Lower Extremities?
Case Report

A 66-year-old man with no past medical history presented with a pruritic eruption on the lower extremities of approximately 3 weeks’ duration. The patient endorsed possible chigger bites while working on his farm prior to the appearance of the rash. The lesions started as papules that subsequently became umbilicated. On physical exam, there were numerous umbilicated, crusted papules and plaques with erythematous borders involving the bilateral anterior lower extremities up to the distal thigh (Figure 1).
Scroll below to find out the answer!
Answer
 Acquired Reactive Perforating Collagenosis
Acquired Reactive Perforating Collagenosis
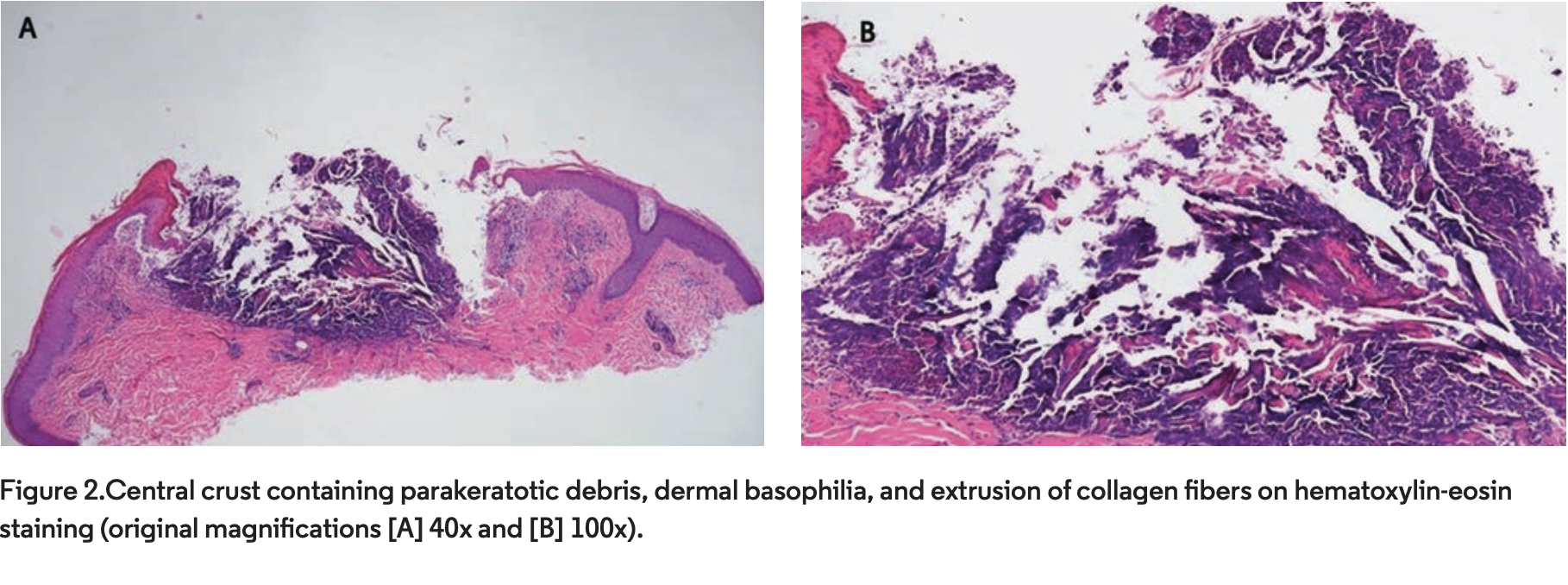
Reactive perforating collagenosis (RPC) was first described in 1967 as an unusual reaction to superficial trauma.1 Because the original description was of a child, it represented the now known familial variant. Mehregan et al1 described the life of the lesions in both clinical and histopathologic detail. The eruption initially presented as pruritic, skin-colored papules that became umbilicated with a central keratinaceous plug, which then enlarged to 4 mm to 6 mm over 3 to 5 weeks with the keratinaceous plug acquiring a brown, leathery, and deeply adherent quality (Figure 1). The lesions then finally entered a phase of regression and completely resolved within 6 to 8 weeks. Histopathologically, a fully developed, umbilicated lesion showed extrusion of vertically oriented collagen fibers amid a basophilic papillary dermis and parakeratotic debris.1 The extruded material can be confirmed to be collagen by Masson’s trichome stain.2
Subsequently, identical lesions were described in older adults usually in association with diabetes and renal disease.3-6 Rarely, cases of acquired RPC appear without systemic disease such as the case presented herein.7 In contrast to the familial variant, the clinical course is often protracted.7,8
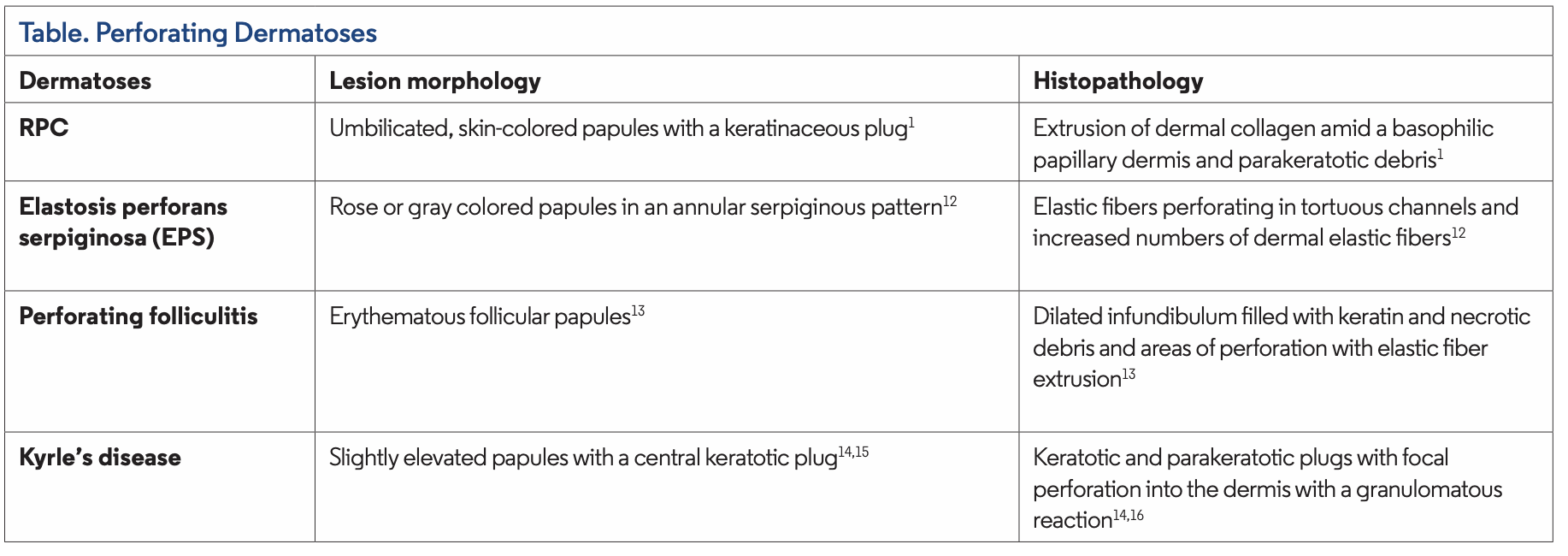
Although Mehregan et al1 noted an absence of elastic fibers within the devitalized plug in the original description, some studies demonstrated extrusion of elastin fibers as well.9-11 As a result, some authors advocate the term acquired perforating dermatosis, because there seems to be considerable overlap and disagreement on the classification and features of the classically described perforating disorders (Table1, 12-16).10
Although the etiopathogenesis of RPC is poorly understood, it is accepted that trauma induced by scratching seems to be an important triggering factor. This observation explains the frequent koebnerization of lesions and the numerous cases linked to scabies infestation or more rarely to exacerbations of atopic dermatitis.11, 17-20 Some authors proposed that vasculopathy, subsequent hypoxia, and dermal necrosis in response to trauma are the key factors in this disease.6 Other theories include deposition of byproducts of chronic kidney disease within the dermis while others highlight the potential role of polymorphonuclear cells with the release of lysosomal enzymes in its pathogenesis.5, 21, 22 Ultrastructurally, the eliminated collagen is not degenerated and showed normal periodicity.23,24 The role of glycated collagen I and III in the mechanism of transepithelial elimination was explored in cell cultures, where it was shown that exposing keratinocytes to these advanced glycation end products induced terminal differentiation of keratinocytes through the AGE-receptor CD36 with concomitant and upward movement of keratinocytes and collagen.25 Finally, overexpression of TGFB-3 (an important peptide in tissue repair) by immunohistochemistry has been documented.26,27
Differential Diagnosis
The differential diagnosis of RPC includes prurigo nodularis and the other traditionally recognized perforating disorders of EPS, perforating folliculitis, and Kyrle’s disease. EPS is characterized by its classical serpiginous or annular distribution of keratotic papules with preferential involvement of the back or sides of neck and frequent association to genetic disorders such as Down syndrome, Marfan syndrome, EhlerDanlos, osteogenesis imperfecta, pseudoexanthoma elasticum, and long-term use of penicillamine.12 By histology, there is elimination of elastic fibers through perforating epithelial channels along with an increase in elastic fibers in the dermis.12 Perforating folliculitis consists of an asymptomatic to pruriginous, discrete follicular papules with a central keratinous plug.13 Although it can be seen in association with chronic kidney disease, it is often seen in the absence of systemic disease and more recently also associated with the use of kinase inhibitors such as sorafenib.28-30 On histopathology, there is a dilated hair follicle plugged with keratinous material and necrotic crust. Serial sectioning reveals the areas of perforation located at the level of the follicular infundibulum where elastic fibers, necrotic connective tissue, and degenerated inflammatory cells access the follicular cavity. In the near vicinity of this area, a curled hair shaft may be seen.31 Kyrle’s disease is considered a controversial entity by several authors; many cases described in the literature as such were reclassified to represent RPC or the end-stage of other disorders including perforating folliculitis.10,31 Strict criteria to diagnose this disorder as described by Kyrle14 and reviewed by Carter and Constantine15,16 include a chronic popular eruption with a cone shaped hyperkeratotic plug that may or may not involve the hair follicles. Histopathology shows a keratotic plug with basophilic debris and parakeratosis which may also involve the basal layer where epidermal disruption occurs. In this focus, a dermal granulomatous reaction is usually seen. Importantly, there is no extrusion of elastic fibers. This entity can also be associated with renal failure and diabetes mellitus.32,33
Prurigo nodularis is a chronic dermatosis characterized by dome-shaped papulonodules distributed symmetrically in areas accessible to scratching such as the extensor surfaces of extremities and trunk. The lesions may have a central scale, crust, or ulcerations. The diagnosis is usually clinical. Of note, some authors describe the umbilicated variant of prurigo nodularis and propose that acquired reactive perforating dermatosis is a variant of it.34 This view, however, is not universally accepted and the cases described were in the setting of diabetes mellitus and chronic kidney disease. Additionally, when evaluated by histopathology, some showed extrusion of collagen fibers within the plug.13
Management
Treatment of acquired RPC is challenging, with no clinical trials available to recommend a standard treatment. Evaluation of treatment efficacies is also confounded by the fact that some lesions may spontaneously self-involute. Efforts should focus on controlling the pruritus and managing comorbid diseases. Case series and case reports showed efficacy of narrowband (NB) UV-B, allopurinol, topical doxycycline and systemic retinoids, topical and intralesional steroids, usually in combination with antihistamines, and topical combination of benzoyl peroxide and steroids among others.18,32, 35-41
Our Patient
A complete blood count, comprehensive metabolic panel, antinuclear antibodies, and protein electrophoresis were within normal limits. A punch biopsy revealed a central crater containing parakeratotic debris, basophilic debris, extrusion of collagen fibers, and a mixed inflammatory infiltrate (Figure 2). The clinical and histopathologic findings were that of RPC. The patient underwent three sessions of NB-UVB with improvement and was lost to follow-up.
Conclusion
This case highlights the clinical presentation of acquired RPC likely triggered by chigger bites in a patient without systemic disease. As others have hypothesized, it is a further piece of evidence that the trauma induced by scratching may play an important role in the formation of lesions.
References
1. Mehregan AH, Schwartz OD, Livingood CS. Reactive perforating collagenosis. Arch Dermatol. 1967;96(3):277-282.
2. Karpouzis A, Giatromanolaki A, Sivridis E, Kouskoukis C. Acquired reactive perforating collagenosis: current status. J Dermatol. 2010;37(7):585-592. doi:10.1111/j.1346-8138.2010.00918.x
3. Poliak SC, Lebwohl MG, Parris A, Prioleau PG. Reactive perforating collagenosis associated with diabetes mellitus. N Engl J Med. 1982;306(2):81-84. doi:10.1056/NEJM198201143060206
4. Cochran RJ, Tucker SB, Wilkin JK. Reactive perforating collagenosis of diabetes mellitus and renal failure. Cutis. 1983;31(1):55-58.
5. Morton CA, Henderson IS, Jones MC, Lowe JG. Acquired perforating dermatosis in a British dialysis population. Br J Dermatol. 1996;135(5):671-677.
6. Kawakami T, Saito R. Acquired reactive perforating collagenosis associated with diabetes mellitus: eight cases that meet Faver’s criteria. Br J Dermatol. 1999;140(3):521-524. doi:10.1046/j.1365-2133.1999.02722.x
7. Kim SW, Kim MS, Lee JH, et al. A clinicopathologic study of thirty cases of acquired perforating dermatosis in Korea. Ann Dermatol. 2014;26(2):162-171. doi:10.5021/ad.2014.26.2.162
8. García-Malinis AJ, Del Valle Sánchez E, Sánchez-Salas MP, Del Prado E, Coscojuela C, Gilaberte Y. Acquired perforating dermatosis: clinicopathological study of 31 cases, emphasizing pathogenesis and treatment. J Eur Acad Dermatol Venereol. 2017;31(10):1757-1763. doi:10.1111/jdv.14220
9. Millard PR, Young E, Harrison DE, Wojnarowska F. Reactive perforating collagenosis: light, ultrastructural and immunohistological studies. Histopathology. 1986;10(10):1047-1056. doi:10.1111/j.1365-2559.1986.tb02541.x
10. Rapini RP, Herbert AA, Drucker CR. Acquired perforating dermatosis. Evidence for combined transepidermal elimination of both collagen and elastic fibers. Arch Dermatol. 1989;125(8):1074-1078. doi:10.1001/archderm.125.8.1074
11. Thiele-Ochel S, Schneider LA, Reinhold K, Hunzelmann N, Krieg T, Scharffetter-Kochanek K. Acquired perforating collagenosis: is it due to damage by scratching? Br J Dermatol. 2001;145(1):173-174. doi:10.1046/j.1365-2133.2001.04309.x
12. Mehregan AH. Elastosis perforans serpiginosa: a review of the literature and report of 11 cases. Arch Dermatol. 1968;97(4):381-393. doi:10.1001/archderm.97.4.381
13. Mehregan AH, Coskey RJ. Perforating folliculitis. Arch Dermatol. 1968;97(4):394-399. doi:10.1001/archderm.1968.01610100034004
14. Kyrle J. Hyperkeratosis Follicularis et parafollicularis in cutem penetrans. Arch Derm Syph. 1916;123:466-493.
15. Carter VH, Constantine VS. Kyrle’s disease. I. Clinical findings in five cases and review of literature. Arch Dermatol. 1968;97(6):624-632. doi:10.1001/archderm.97.6.624
16. Constantine VS, Carter VH. Kyrle’s disease. II. Histopathologic findings in five cases and review of the literature. Arch Dermatol. 1968;97(6):633-639. doi:10.1001/archderm.97.6.633
17. Kurschat P, Kröger A, Scharffetter-Kochanek K, Hunzelmann N. Acquired reactive perforating collagenosis triggered by scabies infection. Acta Derm Venereol. 2000;80(5):384-385.
18. Brinkmeier T, Herbst RA, Frosch PJ. Reactive perforating collagenosis associated with scabies in a diabetic. J Eur Acad Dermatol Venereol. 2004;18(5):588-590. doi:10.1111/j.1468-3083.2004.00978.x
19. Hinrichs W, Breuckmann F, Altmeyer P, Kreuter A. Acquired perforating dermatosis: a report on 4 cases associated with scabies infection. J Am Acad Dermatol. 2004;51(4):665-667. doi:10.1016/j.jaad.2004.02.025
20. Ikezaki E, Sugita K, Kabashima K, Tokura Y. Scabies-induced acquired reactive perforating collagenosis. J Eur Acad Dermatol Venereol. 2008;22(1):120-121. doi:10.1111/j.1468-3083.2007.02285.x.
21. Zelger B, Hintner H, Auböck J, Fritsch PO. Acquired perforating dermatosis. Transepidermal elimination of DNA material and possible role of leukocytes in pathogenesis. Arch Dermatol. 1991;127(5):695-700. doi:10.1001/archderm.127.5.695
22. Patterson JW, Brown PC. Ultrastructural changes in acquired perforating dermatosis. Int J Dermatol. 1992;31(3):201-205. doi:10.1111/j.1365-4362.1992.tb03937.x
23. Yanagihara M, Fujita T, Shirasaki A, Ishiguro K, Kawahara K, Ueda K. The pathogenesis of the transepithelial elimination of the collagen bundles in acquired reactive perforating collagenosis. A light and electron microscopical study. J Cutan Pathol. 1996;23(5):398-403. doi:10.1111/j.1600-0560.1996.tb01429.x.
24. Beck HI, Brandrup F, Hagdrup HK, Jensen NK, Starklint H. Adult, acquired reactive perforating collagenosis. Report of a case including ultrastructural findings. J Cutan Pathol. 1988;15(2):124-128. doi:10.1111/j.1600-0560.1988.tb00532.x
25. Fujimoto E, Kobayashi T, Fujimoto N, Akiyama M, Tajima S, Nagai R. AGE-modified collagens I and III induce keratinocyte terminal differentiation through AGE receptor CD36: epidermal-dermal interaction in acquired perforating dermatosis. J Invest Dermatol. 2010;130(2):405-414. doi:10.1038/jid.2009.269
26. Kawakami T, Soma Y, Mizoguchi M, Saito R. Immunohistochemical analysis of transforming growth factor-beta3 expression in acquired reactive perforating collagenosis. Br J Dermatol. 2001;144(1):197-199. doi:10.1046/j.1365-2133.2001.03982.x
27. Gambichler T, Birkner L, Stücker M, Othlinghaus N, Altmeyer P, Kreuter A. Up-regulation of transforming growth factor-beta3 and extracellular matrix proteins in acquired reactive perforating collagenosis. J Am Acad Dermatol. 2009;60(3):463-469. doi: 10.1016/j.jaad.2008.06.006
28. Hurwitz RM, Melton ME, Creech FT 3rd, Weiss J, Handt A. Perforating folliculitis in association with hemodialysis. Am J Dermatopathol. 1982;4(2):101-108. doi:10.1097/00000372-198204000-00001.
29. Hurwitz RM. The evolution of perforating folliculitis in patients with chronic renal failure. Am J Dermatopathol. 1985;7(3):231-239. doi:10.1097/00000372-198506000-00004
30. Minami-Hori M, Ishida-Yamamoto A, Komatsu S, Iiduka H. Transient perforating folliculitis induced by sorafenib. J Dermatol. 2010;37(9):833-834. doi:10.1111/j.1346-8138.2010.00885.x
31. Mehregan AH. Perforating dermatoses: a clinicopathologic review. Int J Dermatol. 1977;16(1):19-27. doi:10.1111/j.1365-4362.1977.tb00733.x
32. Hood AF, Hardegen GL, Zarate AR, Nigra TP, Gelfand MC. Kyrle’s disease in patients with chronic renal failure. Arch Dermatol. 1982;118(2):85-88.
33. Saray Y, Seçkin D, Bilezikçi B. Acquired perforating dermatosis: clinicopathological features in twenty-two cases. J Eur Acad Dermatol Venereol. 2006;20(6):679-688. doi:10.1111/j.1468-3083.2006.01571.x
34. Kestner RI, Ständer S, Osada N, Ziegler D, Metze D. Acquired reactive perforating dermatosis is a variant of prurigo nodularis. Acta Derm Venereol. 2017;97(2):249-254. doi:10.2340/00015555-2492
35. Ohe S, Danno K, Sasaki H, Isei T, Okamoto H, Horio T. Treatment of acquired perforating dermatosis with narrowband ultraviolet B. J Am Acad Dermatol. 2004;50(6):892-894. doi:10.1016/j.jaad.2004.02.009.
36. Gambichler T, Altmeyer P, Kreuter A. Treatment of acquired perforating dermatosis with narrowband ultraviolet B. J Am Acad Dermatol. 2005;52(2):363-364. doi:10.1016/j.jaad.2004.08.018
37. Tilz H, Becker JC, Legat F, Schettini AP, Inzinger M, Massone C. Allopurinol in the treatment of acquired reactive perforating collagenosis. An Bras Dermatol. 2013;88(1):94-97. doi:10.1590/s0365-05962013000100012
38. Hoque SR, Ameen M, Holden CA. Acquired reactive perforating collagenosis: four patients with a giant variant treated with allopurinol. Br J Dermatol. 2006;154(4):759-762. doi:10.1111/j.1365-2133.2005.07111.x
39. Lukács J, Schliemann S, Elsner P. Treatment of acquired reactive perforating dermatosis - a systematic review. J Dtsch Dermatol Ges. 2018;16(7):825-842. doi:10.1111/ddg.13561
40. Satchell AC, Crotty K, Lee S. Reactive perforating collagenosis: a condition that may be underdiagnosed. Australas J Dermatol. 2001;42(4):284-287. doi:10.1046/j.1440-0960.2001.00537.x.
41. Miyanaga M, Oyama N, Sakai Y, Imamura Y, Hasegawa M. Successful treatment of acquired reactive perforating collagenosis with topical benzoyl peroxide: a possible therapeutic action underlying structural and metabolic turnover. J Dermatol. 2020;47(1):e12-e14. doi:10.1111/1346-8138.15102
Affiliations
Dr Grayson is a PGY-1 at Florida State University College of Medicine internal medicine residency program in Tallahassee, FL. Dr Deschaine is a PGY-4 at Florida State University College of Medicine dermatology residency program. Dr Cohen is a clinical physician at University of Florida Department of Dermatology in Gainesville, FL. Dr Johnson is a clinical assistant professor at University of Florida Department of Dermatology.





















