 1. This generalized eruption has been present intermittently for 6 weeks. Assuming that “discoid” lesions are also present, which of the following tests has the highest sensitivity and specificity to confirm the clinical diagnosis of systemic lupus erythematosus (SLE)?
1. This generalized eruption has been present intermittently for 6 weeks. Assuming that “discoid” lesions are also present, which of the following tests has the highest sensitivity and specificity to confirm the clinical diagnosis of systemic lupus erythematosus (SLE)?
a) Serum antinuclear antibody (ANA) test
b) Direct immunofluorescence of lesional skin
c) Routine histology of lesional skin
d) Response to systemic antimalarial therapy
e) Sm antibody test
 2. The most likely diagnosis is:
2. The most likely diagnosis is:
a) Pemphigus foliaceus
b) Pemphigus vulgaris
c) Familial pemphigus (Hailey-Hailey disease)
d) Pemphigus erythematoides
e) Pemphigus vegetans
ANSWERS:
1. This generalized eruption has been present intermittently for 6 weeks. Assuming that “discoid” lesions are also present, which of the following tests has the highest sensitivity and specificity to confirm the clinical diagnosis of systemic lupus erythematosus?
ANSWER: c) Routine histology of lesional skin
 Clinically this young woman has the typical butterfly eruption of SLE. The differential diagnosis of this eruption, based solely on morphology, includes rosacea, polymorphous light eruption (PMLE), seborrheic dermatitis, pemphigus foliaceus (masquerading as seborrheic dermatitis), and an allergic contact dermatitis. The histologic finding in lupus erythematosus are very characteristic, including epidermal atrophy; follicular plugging (“carpet tacking”); hyperkeratosis; vacuolar degeneration of the epithelial basal cell layer; periodic acid–Schiff-positive thickening of the dermoepidermal junction basement membrane; deposition of mucin within the papillary dermis; and the presence of a chronic inflammatory cellular infiltrate along the dermoepidermal junction, around hair follicles, and around dermal vasculature. An eruption of lupus erythematosus that has been present for up to 6 weeks should demonstrate at least several of these diagnostically useful features (which is why the duration was listed in the question).
Clinically this young woman has the typical butterfly eruption of SLE. The differential diagnosis of this eruption, based solely on morphology, includes rosacea, polymorphous light eruption (PMLE), seborrheic dermatitis, pemphigus foliaceus (masquerading as seborrheic dermatitis), and an allergic contact dermatitis. The histologic finding in lupus erythematosus are very characteristic, including epidermal atrophy; follicular plugging (“carpet tacking”); hyperkeratosis; vacuolar degeneration of the epithelial basal cell layer; periodic acid–Schiff-positive thickening of the dermoepidermal junction basement membrane; deposition of mucin within the papillary dermis; and the presence of a chronic inflammatory cellular infiltrate along the dermoepidermal junction, around hair follicles, and around dermal vasculature. An eruption of lupus erythematosus that has been present for up to 6 weeks should demonstrate at least several of these diagnostically useful features (which is why the duration was listed in the question).
An empiric trial of antimalarial therapy is not diagnostically helpful because these patients with PMLE, also usually respond rapidly and completely to such therapy as will patients with some other diseases (eg, sarcoid). An ANA test is not very specific, because a low-positive ANA may occur in many otherwise healthy young white females. Direct immunofluorescence, although a sensitive test for SLE (up to 90% plus positivity), may also be infrequently positive in other facial eruptions (to include rosacea), as well as rarely in normal appearing or photoaged facial skin. Although highly specific for SLE, anti-Sm antibodies are present in only a minority of these patients, making it a highly insensitive marker of the disease.
Reference
Histopathology of the Skin. 7th ed. Lever et al. (eds.). pp. 494-505.
2. The most likely diagnosis is:
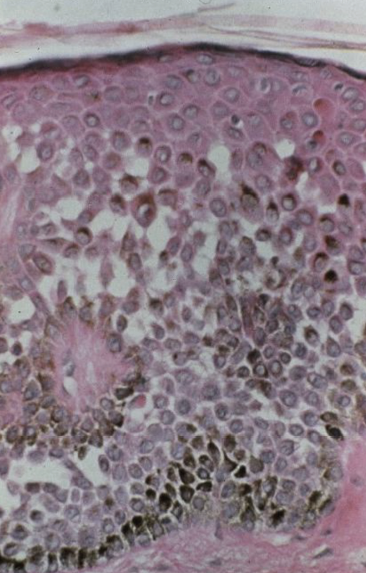
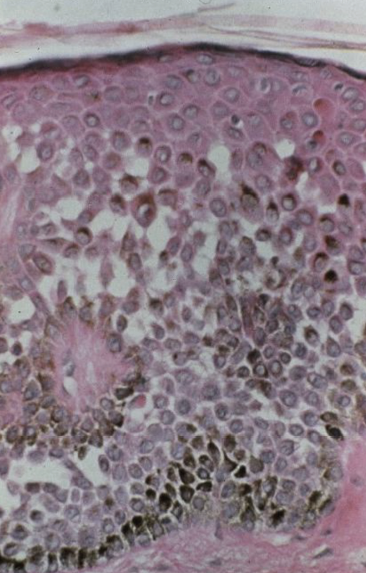
ANSWER: c) Familial pemphigus (Hailey-Hailey disease)
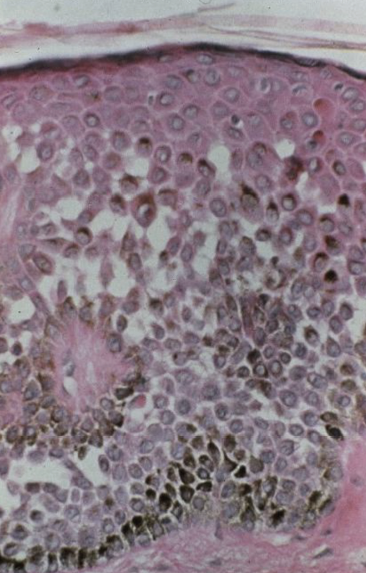 Histologic features characteristic of familial pemphigus include the absence of inflammation and widespread intraepidermal acantholysis affecting multiple layers of keratinocytes and mainly located in the lower epidermis (“dilapidated brick wall”). The widespread nature of acantholysis in familial pemphigus distinguishes it from other forms of pemphigus, in which acantholysis is relatively localized to the subcorneal (pemphigus foliaceus) or suprabasilar (pemphigus vulgaris) regions. Hailey-Hailey disease results from mutations in the ATP2C1 gene, a gene encoding for a novel Ca2+ pump.
Histologic features characteristic of familial pemphigus include the absence of inflammation and widespread intraepidermal acantholysis affecting multiple layers of keratinocytes and mainly located in the lower epidermis (“dilapidated brick wall”). The widespread nature of acantholysis in familial pemphigus distinguishes it from other forms of pemphigus, in which acantholysis is relatively localized to the subcorneal (pemphigus foliaceus) or suprabasilar (pemphigus vulgaris) regions. Hailey-Hailey disease results from mutations in the ATP2C1 gene, a gene encoding for a novel Ca2+ pump.
References
Ackerman AB, Sanchez J, Guo Y, Chongchitnant N, Bennin B. Histologic Diagnosis of Inflammatory Skin Diseases: An Algorithmic Method Based on Pattern Analysis. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 1997:532-534.
Chao SC, Tsai YM, Yang MH. Mutation analysis of ATP2C1 gene in Taiwanese patients with Hailey-Hailey disease. Br J Dermatol. 2002;146(4):595-600.
Yokota K, Yasukawa K, Shimizu H. Analysis of ATP2C1 gene mutation in 10 unrelated Japanese families with Hailey-Hailey disease. J Invest Dermatol. 2002;118(3):550-551.
Ton VK, Mandal D, Vahadji C, Rao R. Functional expression in yeast of the human secretory pathway Ca(2+), Mn(2+)-ATPase defective in Hailey-Hailey disease. J Biol Chem. 2002;277(8):6422-6427.
 1. This generalized eruption has been present intermittently for 6 weeks. Assuming that “discoid” lesions are also present, which of the following tests has the highest sensitivity and specificity to confirm the clinical diagnosis of systemic lupus erythematosus (SLE)?
1. This generalized eruption has been present intermittently for 6 weeks. Assuming that “discoid” lesions are also present, which of the following tests has the highest sensitivity and specificity to confirm the clinical diagnosis of systemic lupus erythematosus (SLE)?
a) Serum antinuclear antibody (ANA) test
b) Direct immunofluorescence of lesional skin
c) Routine histology of lesional skin
d) Response to systemic antimalarial therapy
e) Sm antibody test
 2. The most likely diagnosis is:
2. The most likely diagnosis is:
a) Pemphigus foliaceus
b) Pemphigus vulgaris
c) Familial pemphigus (Hailey-Hailey disease)
d) Pemphigus erythematoides
e) Pemphigus vegetans
ANSWERS:
1. This generalized eruption has been present intermittently for 6 weeks. Assuming that “discoid” lesions are also present, which of the following tests has the highest sensitivity and specificity to confirm the clinical diagnosis of systemic lupus erythematosus?
ANSWER: c) Routine histology of lesional skin
 Clinically this young woman has the typical butterfly eruption of SLE. The differential diagnosis of this eruption, based solely on morphology, includes rosacea, polymorphous light eruption (PMLE), seborrheic dermatitis, pemphigus foliaceus (masquerading as seborrheic dermatitis), and an allergic contact dermatitis. The histologic finding in lupus erythematosus are very characteristic, including epidermal atrophy; follicular plugging (“carpet tacking”); hyperkeratosis; vacuolar degeneration of the epithelial basal cell layer; periodic acid–Schiff-positive thickening of the dermoepidermal junction basement membrane; deposition of mucin within the papillary dermis; and the presence of a chronic inflammatory cellular infiltrate along the dermoepidermal junction, around hair follicles, and around dermal vasculature. An eruption of lupus erythematosus that has been present for up to 6 weeks should demonstrate at least several of these diagnostically useful features (which is why the duration was listed in the question).
Clinically this young woman has the typical butterfly eruption of SLE. The differential diagnosis of this eruption, based solely on morphology, includes rosacea, polymorphous light eruption (PMLE), seborrheic dermatitis, pemphigus foliaceus (masquerading as seborrheic dermatitis), and an allergic contact dermatitis. The histologic finding in lupus erythematosus are very characteristic, including epidermal atrophy; follicular plugging (“carpet tacking”); hyperkeratosis; vacuolar degeneration of the epithelial basal cell layer; periodic acid–Schiff-positive thickening of the dermoepidermal junction basement membrane; deposition of mucin within the papillary dermis; and the presence of a chronic inflammatory cellular infiltrate along the dermoepidermal junction, around hair follicles, and around dermal vasculature. An eruption of lupus erythematosus that has been present for up to 6 weeks should demonstrate at least several of these diagnostically useful features (which is why the duration was listed in the question).
An empiric trial of antimalarial therapy is not diagnostically helpful because these patients with PMLE, also usually respond rapidly and completely to such therapy as will patients with some other diseases (eg, sarcoid). An ANA test is not very specific, because a low-positive ANA may occur in many otherwise healthy young white females. Direct immunofluorescence, although a sensitive test for SLE (up to 90% plus positivity), may also be infrequently positive in other facial eruptions (to include rosacea), as well as rarely in normal appearing or photoaged facial skin. Although highly specific for SLE, anti-Sm antibodies are present in only a minority of these patients, making it a highly insensitive marker of the disease.
Reference
Histopathology of the Skin. 7th ed. Lever et al. (eds.). pp. 494-505.
2. The most likely diagnosis is:
ANSWER: c) Familial pemphigus (Hailey-Hailey disease)
 Histologic features characteristic of familial pemphigus include the absence of inflammation and widespread intraepidermal acantholysis affecting multiple layers of keratinocytes and mainly located in the lower epidermis (“dilapidated brick wall”). The widespread nature of acantholysis in familial pemphigus distinguishes it from other forms of pemphigus, in which acantholysis is relatively localized to the subcorneal (pemphigus foliaceus) or suprabasilar (pemphigus vulgaris) regions. Hailey-Hailey disease results from mutations in the ATP2C1 gene, a gene encoding for a novel Ca2+ pump.
Histologic features characteristic of familial pemphigus include the absence of inflammation and widespread intraepidermal acantholysis affecting multiple layers of keratinocytes and mainly located in the lower epidermis (“dilapidated brick wall”). The widespread nature of acantholysis in familial pemphigus distinguishes it from other forms of pemphigus, in which acantholysis is relatively localized to the subcorneal (pemphigus foliaceus) or suprabasilar (pemphigus vulgaris) regions. Hailey-Hailey disease results from mutations in the ATP2C1 gene, a gene encoding for a novel Ca2+ pump.
References
Ackerman AB, Sanchez J, Guo Y, Chongchitnant N, Bennin B. Histologic Diagnosis of Inflammatory Skin Diseases: An Algorithmic Method Based on Pattern Analysis. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 1997:532-534.
Chao SC, Tsai YM, Yang MH. Mutation analysis of ATP2C1 gene in Taiwanese patients with Hailey-Hailey disease. Br J Dermatol. 2002;146(4):595-600.
Yokota K, Yasukawa K, Shimizu H. Analysis of ATP2C1 gene mutation in 10 unrelated Japanese families with Hailey-Hailey disease. J Invest Dermatol. 2002;118(3):550-551.
Ton VK, Mandal D, Vahadji C, Rao R. Functional expression in yeast of the human secretory pathway Ca(2+), Mn(2+)-ATPase defective in Hailey-Hailey disease. J Biol Chem. 2002;277(8):6422-6427.
 1. This generalized eruption has been present intermittently for 6 weeks. Assuming that “discoid” lesions are also present, which of the following tests has the highest sensitivity and specificity to confirm the clinical diagnosis of systemic lupus erythematosus (SLE)?
1. This generalized eruption has been present intermittently for 6 weeks. Assuming that “discoid” lesions are also present, which of the following tests has the highest sensitivity and specificity to confirm the clinical diagnosis of systemic lupus erythematosus (SLE)?
a) Serum antinuclear antibody (ANA) test
b) Direct immunofluorescence of lesional skin
c) Routine histology of lesional skin
d) Response to systemic antimalarial therapy
e) Sm antibody test
 2. The most likely diagnosis is:
2. The most likely diagnosis is:
a) Pemphigus foliaceus
b) Pemphigus vulgaris
c) Familial pemphigus (Hailey-Hailey disease)
d) Pemphigus erythematoides
e) Pemphigus vegetans
,
 1. This generalized eruption has been present intermittently for 6 weeks. Assuming that “discoid” lesions are also present, which of the following tests has the highest sensitivity and specificity to confirm the clinical diagnosis of systemic lupus erythematosus (SLE)?
1. This generalized eruption has been present intermittently for 6 weeks. Assuming that “discoid” lesions are also present, which of the following tests has the highest sensitivity and specificity to confirm the clinical diagnosis of systemic lupus erythematosus (SLE)?
a) Serum antinuclear antibody (ANA) test
b) Direct immunofluorescence of lesional skin
c) Routine histology of lesional skin
d) Response to systemic antimalarial therapy
e) Sm antibody test
 2. The most likely diagnosis is:
2. The most likely diagnosis is:
a) Pemphigus foliaceus
b) Pemphigus vulgaris
c) Familial pemphigus (Hailey-Hailey disease)
d) Pemphigus erythematoides
e) Pemphigus vegetans
ANSWERS:
1. This generalized eruption has been present intermittently for 6 weeks. Assuming that “discoid” lesions are also present, which of the following tests has the highest sensitivity and specificity to confirm the clinical diagnosis of systemic lupus erythematosus?
ANSWER: c) Routine histology of lesional skin
 Clinically this young woman has the typical butterfly eruption of SLE. The differential diagnosis of this eruption, based solely on morphology, includes rosacea, polymorphous light eruption (PMLE), seborrheic dermatitis, pemphigus foliaceus (masquerading as seborrheic dermatitis), and an allergic contact dermatitis. The histologic finding in lupus erythematosus are very characteristic, including epidermal atrophy; follicular plugging (“carpet tacking”); hyperkeratosis; vacuolar degeneration of the epithelial basal cell layer; periodic acid–Schiff-positive thickening of the dermoepidermal junction basement membrane; deposition of mucin within the papillary dermis; and the presence of a chronic inflammatory cellular infiltrate along the dermoepidermal junction, around hair follicles, and around dermal vasculature. An eruption of lupus erythematosus that has been present for up to 6 weeks should demonstrate at least several of these diagnostically useful features (which is why the duration was listed in the question).
Clinically this young woman has the typical butterfly eruption of SLE. The differential diagnosis of this eruption, based solely on morphology, includes rosacea, polymorphous light eruption (PMLE), seborrheic dermatitis, pemphigus foliaceus (masquerading as seborrheic dermatitis), and an allergic contact dermatitis. The histologic finding in lupus erythematosus are very characteristic, including epidermal atrophy; follicular plugging (“carpet tacking”); hyperkeratosis; vacuolar degeneration of the epithelial basal cell layer; periodic acid–Schiff-positive thickening of the dermoepidermal junction basement membrane; deposition of mucin within the papillary dermis; and the presence of a chronic inflammatory cellular infiltrate along the dermoepidermal junction, around hair follicles, and around dermal vasculature. An eruption of lupus erythematosus that has been present for up to 6 weeks should demonstrate at least several of these diagnostically useful features (which is why the duration was listed in the question).
An empiric trial of antimalarial therapy is not diagnostically helpful because these patients with PMLE, also usually respond rapidly and completely to such therapy as will patients with some other diseases (eg, sarcoid). An ANA test is not very specific, because a low-positive ANA may occur in many otherwise healthy young white females. Direct immunofluorescence, although a sensitive test for SLE (up to 90% plus positivity), may also be infrequently positive in other facial eruptions (to include rosacea), as well as rarely in normal appearing or photoaged facial skin. Although highly specific for SLE, anti-Sm antibodies are present in only a minority of these patients, making it a highly insensitive marker of the disease.
Reference
Histopathology of the Skin. 7th ed. Lever et al. (eds.). pp. 494-505.
2. The most likely diagnosis is:
ANSWER: c) Familial pemphigus (Hailey-Hailey disease)
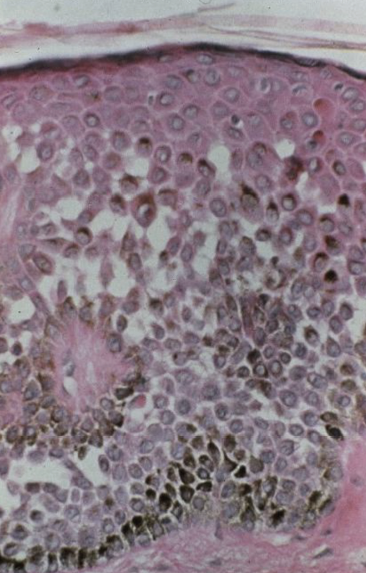 Histologic features characteristic of familial pemphigus include the absence of inflammation and widespread intraepidermal acantholysis affecting multiple layers of keratinocytes and mainly located in the lower epidermis (“dilapidated brick wall”). The widespread nature of acantholysis in familial pemphigus distinguishes it from other forms of pemphigus, in which acantholysis is relatively localized to the subcorneal (pemphigus foliaceus) or suprabasilar (pemphigus vulgaris) regions. Hailey-Hailey disease results from mutations in the ATP2C1 gene, a gene encoding for a novel Ca2+ pump.
Histologic features characteristic of familial pemphigus include the absence of inflammation and widespread intraepidermal acantholysis affecting multiple layers of keratinocytes and mainly located in the lower epidermis (“dilapidated brick wall”). The widespread nature of acantholysis in familial pemphigus distinguishes it from other forms of pemphigus, in which acantholysis is relatively localized to the subcorneal (pemphigus foliaceus) or suprabasilar (pemphigus vulgaris) regions. Hailey-Hailey disease results from mutations in the ATP2C1 gene, a gene encoding for a novel Ca2+ pump.
References
Ackerman AB, Sanchez J, Guo Y, Chongchitnant N, Bennin B. Histologic Diagnosis of Inflammatory Skin Diseases: An Algorithmic Method Based on Pattern Analysis. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 1997:532-534.
Chao SC, Tsai YM, Yang MH. Mutation analysis of ATP2C1 gene in Taiwanese patients with Hailey-Hailey disease. Br J Dermatol. 2002;146(4):595-600.
Yokota K, Yasukawa K, Shimizu H. Analysis of ATP2C1 gene mutation in 10 unrelated Japanese families with Hailey-Hailey disease. J Invest Dermatol. 2002;118(3):550-551.
Ton VK, Mandal D, Vahadji C, Rao R. Functional expression in yeast of the human secretory pathway Ca(2+), Mn(2+)-ATPase defective in Hailey-Hailey disease. J Biol Chem. 2002;277(8):6422-6427.
 1. This generalized eruption has been present intermittently for 6 weeks. Assuming that “discoid” lesions are also present, which of the following tests has the highest sensitivity and specificity to confirm the clinical diagnosis of systemic lupus erythematosus (SLE)?
1. This generalized eruption has been present intermittently for 6 weeks. Assuming that “discoid” lesions are also present, which of the following tests has the highest sensitivity and specificity to confirm the clinical diagnosis of systemic lupus erythematosus (SLE)?
a) Serum antinuclear antibody (ANA) test
b) Direct immunofluorescence of lesional skin
c) Routine histology of lesional skin
d) Response to systemic antimalarial therapy
e) Sm antibody test
 2. The most likely diagnosis is:
2. The most likely diagnosis is:
a) Pemphigus foliaceus
b) Pemphigus vulgaris
c) Familial pemphigus (Hailey-Hailey disease)
d) Pemphigus erythematoides
e) Pemphigus vegetans
ANSWERS:
1. This generalized eruption has been present intermittently for 6 weeks. Assuming that “discoid” lesions are also present, which of the following tests has the highest sensitivity and specificity to confirm the clinical diagnosis of systemic lupus erythematosus?
ANSWER: c) Routine histology of lesional skin
 Clinically this young woman has the typical butterfly eruption of SLE. The differential diagnosis of this eruption, based solely on morphology, includes rosacea, polymorphous light eruption (PMLE), seborrheic dermatitis, pemphigus foliaceus (masquerading as seborrheic dermatitis), and an allergic contact dermatitis. The histologic finding in lupus erythematosus are very characteristic, including epidermal atrophy; follicular plugging (“carpet tacking”); hyperkeratosis; vacuolar degeneration of the epithelial basal cell layer; periodic acid–Schiff-positive thickening of the dermoepidermal junction basement membrane; deposition of mucin within the papillary dermis; and the presence of a chronic inflammatory cellular infiltrate along the dermoepidermal junction, around hair follicles, and around dermal vasculature. An eruption of lupus erythematosus that has been present for up to 6 weeks should demonstrate at least several of these diagnostically useful features (which is why the duration was listed in the question).
Clinically this young woman has the typical butterfly eruption of SLE. The differential diagnosis of this eruption, based solely on morphology, includes rosacea, polymorphous light eruption (PMLE), seborrheic dermatitis, pemphigus foliaceus (masquerading as seborrheic dermatitis), and an allergic contact dermatitis. The histologic finding in lupus erythematosus are very characteristic, including epidermal atrophy; follicular plugging (“carpet tacking”); hyperkeratosis; vacuolar degeneration of the epithelial basal cell layer; periodic acid–Schiff-positive thickening of the dermoepidermal junction basement membrane; deposition of mucin within the papillary dermis; and the presence of a chronic inflammatory cellular infiltrate along the dermoepidermal junction, around hair follicles, and around dermal vasculature. An eruption of lupus erythematosus that has been present for up to 6 weeks should demonstrate at least several of these diagnostically useful features (which is why the duration was listed in the question).
An empiric trial of antimalarial therapy is not diagnostically helpful because these patients with PMLE, also usually respond rapidly and completely to such therapy as will patients with some other diseases (eg, sarcoid). An ANA test is not very specific, because a low-positive ANA may occur in many otherwise healthy young white females. Direct immunofluorescence, although a sensitive test for SLE (up to 90% plus positivity), may also be infrequently positive in other facial eruptions (to include rosacea), as well as rarely in normal appearing or photoaged facial skin. Although highly specific for SLE, anti-Sm antibodies are present in only a minority of these patients, making it a highly insensitive marker of the disease.
Reference
Histopathology of the Skin. 7th ed. Lever et al. (eds.). pp. 494-505.
2. The most likely diagnosis is:
ANSWER: c) Familial pemphigus (Hailey-Hailey disease)
 Histologic features characteristic of familial pemphigus include the absence of inflammation and widespread intraepidermal acantholysis affecting multiple layers of keratinocytes and mainly located in the lower epidermis (“dilapidated brick wall”). The widespread nature of acantholysis in familial pemphigus distinguishes it from other forms of pemphigus, in which acantholysis is relatively localized to the subcorneal (pemphigus foliaceus) or suprabasilar (pemphigus vulgaris) regions. Hailey-Hailey disease results from mutations in the ATP2C1 gene, a gene encoding for a novel Ca2+ pump.
Histologic features characteristic of familial pemphigus include the absence of inflammation and widespread intraepidermal acantholysis affecting multiple layers of keratinocytes and mainly located in the lower epidermis (“dilapidated brick wall”). The widespread nature of acantholysis in familial pemphigus distinguishes it from other forms of pemphigus, in which acantholysis is relatively localized to the subcorneal (pemphigus foliaceus) or suprabasilar (pemphigus vulgaris) regions. Hailey-Hailey disease results from mutations in the ATP2C1 gene, a gene encoding for a novel Ca2+ pump.
References
Ackerman AB, Sanchez J, Guo Y, Chongchitnant N, Bennin B. Histologic Diagnosis of Inflammatory Skin Diseases: An Algorithmic Method Based on Pattern Analysis. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 1997:532-534.
Chao SC, Tsai YM, Yang MH. Mutation analysis of ATP2C1 gene in Taiwanese patients with Hailey-Hailey disease. Br J Dermatol. 2002;146(4):595-600.
Yokota K, Yasukawa K, Shimizu H. Analysis of ATP2C1 gene mutation in 10 unrelated Japanese families with Hailey-Hailey disease. J Invest Dermatol. 2002;118(3):550-551.
Ton VK, Mandal D, Vahadji C, Rao R. Functional expression in yeast of the human secretory pathway Ca(2+), Mn(2+)-ATPase defective in Hailey-Hailey disease. J Biol Chem. 2002;277(8):6422-6427.
ANSWERS:
1. This generalized eruption has been present intermittently for 6 weeks. Assuming that “discoid” lesions are also present, which of the following tests has the highest sensitivity and specificity to confirm the clinical diagnosis of systemic lupus erythematosus?
ANSWER: c) Routine histology of lesional skin
 Clinically this young woman has the typical butterfly eruption of SLE. The differential diagnosis of this eruption, based solely on morphology, includes rosacea, polymorphous light eruption (PMLE), seborrheic dermatitis, pemphigus foliaceus (masquerading as seborrheic dermatitis), and an allergic contact dermatitis. The histologic finding in lupus erythematosus are very characteristic, including epidermal atrophy; follicular plugging (“carpet tacking”); hyperkeratosis; vacuolar degeneration of the epithelial basal cell layer; periodic acid–Schiff-positive thickening of the dermoepidermal junction basement membrane; deposition of mucin within the papillary dermis; and the presence of a chronic inflammatory cellular infiltrate along the dermoepidermal junction, around hair follicles, and around dermal vasculature. An eruption of lupus erythematosus that has been present for up to 6 weeks should demonstrate at least several of these diagnostically useful features (which is why the duration was listed in the question).
Clinically this young woman has the typical butterfly eruption of SLE. The differential diagnosis of this eruption, based solely on morphology, includes rosacea, polymorphous light eruption (PMLE), seborrheic dermatitis, pemphigus foliaceus (masquerading as seborrheic dermatitis), and an allergic contact dermatitis. The histologic finding in lupus erythematosus are very characteristic, including epidermal atrophy; follicular plugging (“carpet tacking”); hyperkeratosis; vacuolar degeneration of the epithelial basal cell layer; periodic acid–Schiff-positive thickening of the dermoepidermal junction basement membrane; deposition of mucin within the papillary dermis; and the presence of a chronic inflammatory cellular infiltrate along the dermoepidermal junction, around hair follicles, and around dermal vasculature. An eruption of lupus erythematosus that has been present for up to 6 weeks should demonstrate at least several of these diagnostically useful features (which is why the duration was listed in the question).
An empiric trial of antimalarial therapy is not diagnostically helpful because these patients with PMLE, also usually respond rapidly and completely to such therapy as will patients with some other diseases (eg, sarcoid). An ANA test is not very specific, because a low-positive ANA may occur in many otherwise healthy young white females. Direct immunofluorescence, although a sensitive test for SLE (up to 90% plus positivity), may also be infrequently positive in other facial eruptions (to include rosacea), as well as rarely in normal appearing or photoaged facial skin. Although highly specific for SLE, anti-Sm antibodies are present in only a minority of these patients, making it a highly insensitive marker of the disease.
Reference
Histopathology of the Skin. 7th ed. Lever et al. (eds.). pp. 494-505.
2. The most likely diagnosis is:
ANSWER: c) Familial pemphigus (Hailey-Hailey disease)
 Histologic features characteristic of familial pemphigus include the absence of inflammation and widespread intraepidermal acantholysis affecting multiple layers of keratinocytes and mainly located in the lower epidermis (“dilapidated brick wall”). The widespread nature of acantholysis in familial pemphigus distinguishes it from other forms of pemphigus, in which acantholysis is relatively localized to the subcorneal (pemphigus foliaceus) or suprabasilar (pemphigus vulgaris) regions. Hailey-Hailey disease results from mutations in the ATP2C1 gene, a gene encoding for a novel Ca2+ pump.
Histologic features characteristic of familial pemphigus include the absence of inflammation and widespread intraepidermal acantholysis affecting multiple layers of keratinocytes and mainly located in the lower epidermis (“dilapidated brick wall”). The widespread nature of acantholysis in familial pemphigus distinguishes it from other forms of pemphigus, in which acantholysis is relatively localized to the subcorneal (pemphigus foliaceus) or suprabasilar (pemphigus vulgaris) regions. Hailey-Hailey disease results from mutations in the ATP2C1 gene, a gene encoding for a novel Ca2+ pump.
References
Ackerman AB, Sanchez J, Guo Y, Chongchitnant N, Bennin B. Histologic Diagnosis of Inflammatory Skin Diseases: An Algorithmic Method Based on Pattern Analysis. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 1997:532-534.
Chao SC, Tsai YM, Yang MH. Mutation analysis of ATP2C1 gene in Taiwanese patients with Hailey-Hailey disease. Br J Dermatol. 2002;146(4):595-600.
Yokota K, Yasukawa K, Shimizu H. Analysis of ATP2C1 gene mutation in 10 unrelated Japanese families with Hailey-Hailey disease. J Invest Dermatol. 2002;118(3):550-551.
Ton VK, Mandal D, Vahadji C, Rao R. Functional expression in yeast of the human secretory pathway Ca(2+), Mn(2+)-ATPase defective in Hailey-Hailey disease. J Biol Chem. 2002;277(8):6422-6427.
 1. This generalized eruption has been present intermittently for 6 weeks. Assuming that “discoid” lesions are also present, which of the following tests has the highest sensitivity and specificity to confirm the clinical diagnosis of systemic lupus erythematosus (SLE)?
1. This generalized eruption has been present intermittently for 6 weeks. Assuming that “discoid” lesions are also present, which of the following tests has the highest sensitivity and specificity to confirm the clinical diagnosis of systemic lupus erythematosus (SLE)? 2. The most likely diagnosis is:
2. The most likely diagnosis is:





 1. This generalized eruption has been present intermittently for 6 weeks. Assuming that “discoid” lesions are also present, which of the following tests has the highest sensitivity and specificity to confirm the clinical diagnosis of systemic lupus erythematosus (SLE)?
1. This generalized eruption has been present intermittently for 6 weeks. Assuming that “discoid” lesions are also present, which of the following tests has the highest sensitivity and specificity to confirm the clinical diagnosis of systemic lupus erythematosus (SLE)?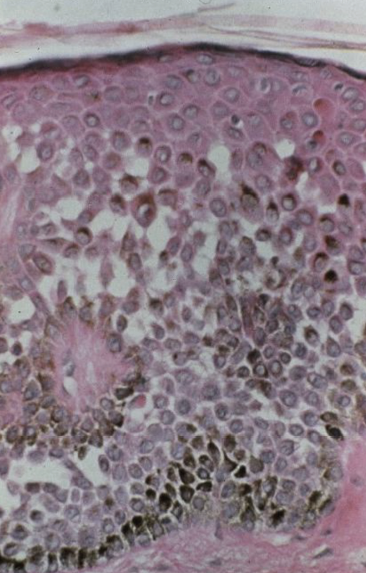 2. The most likely diagnosis is:
2. The most likely diagnosis is:














