An Unfortunate Combination of Tachycardia and Myocardial Bridge: A Case of Myocardial Infarction Related to Atrial Flutter
Abstract
J INVASIVE CARDIOL 2022;34(2):E152-E153.
Key words: angina, atrial flutter, myocardial bridge, tachyarrhythmia-induced myocardial infarction
Case Presentation
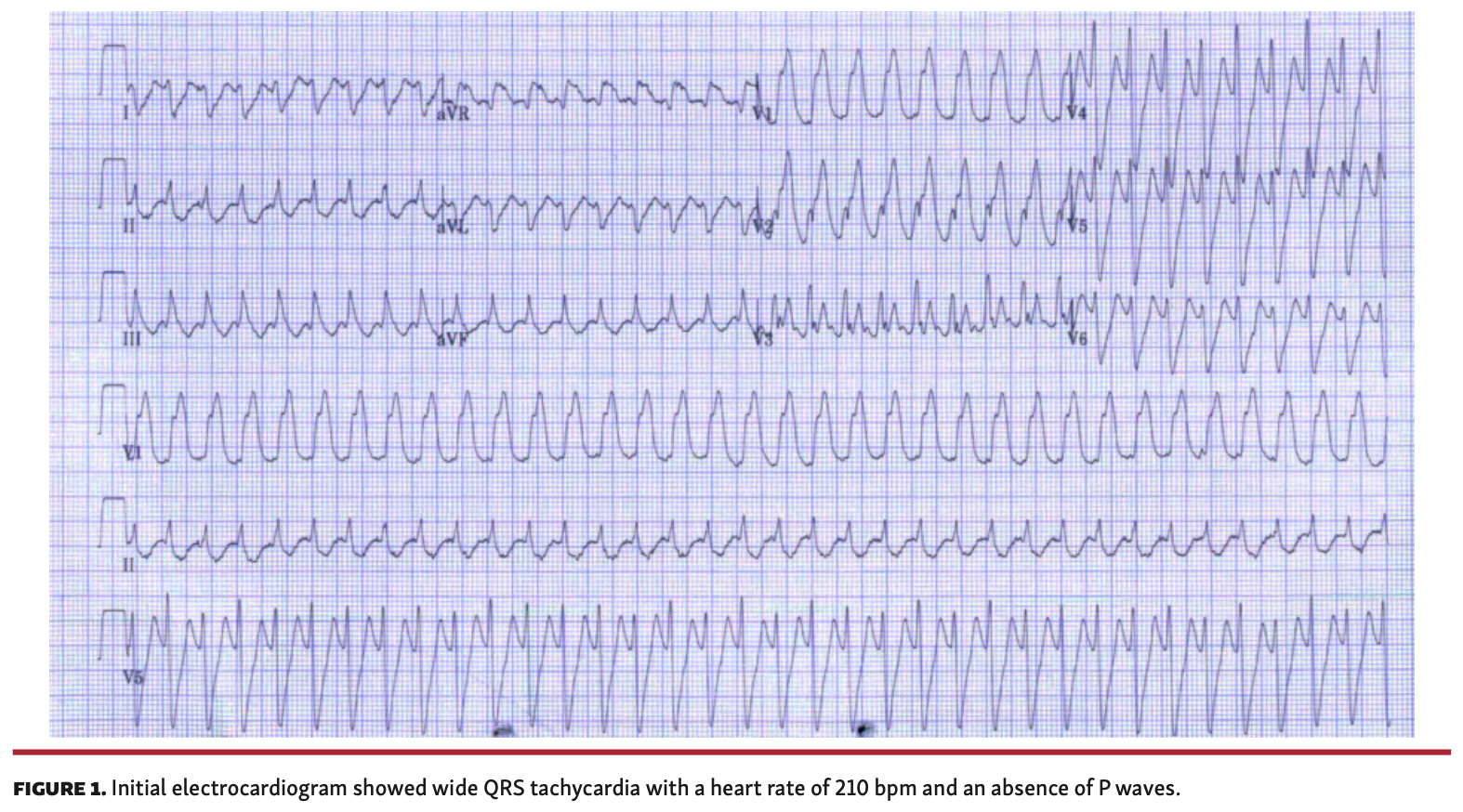
A 58-year-old man presented to the emergency room with squeezing chest pain and palpitations. Electrocardiography (ECG) showed wide QRS tachycardia with a heart rate of 210 bpm and an absence of P waves (Figure 1). After electrical cardioversion, heart rhythm converted to a normal sinus rhythm. Blood chemistry and echocardiography showed normal findings, except for an elevated troponin I level (0.492 ng/mL).
An electrophysiological study (EPS) was performed and atrial flutter (AFL) was induced similar to the initial ECG. Because his presenting symptom was angina, the patient was referred for coronary angiography at this point to rule out significant coronary disease. No significant coronary lesions were detected; however, a myocardial bridge was noted in the mid left anterior descending artery (mLAD) (Figures 2A and 2B). As the patient’s symptoms were combined with tachycardia, coronary angiography was repeated with concurrent EPS. During induced tachycardia, persistent compression and near total obstruction of the mLAD were seen (Figures 2C and 2D), and the patient complained of severe angina similar to his initial episode. Catheter ablation of the AFL was successfully completed, and at the 8-month follow-up visit, the patient remained free from both chest pain and palpitations.
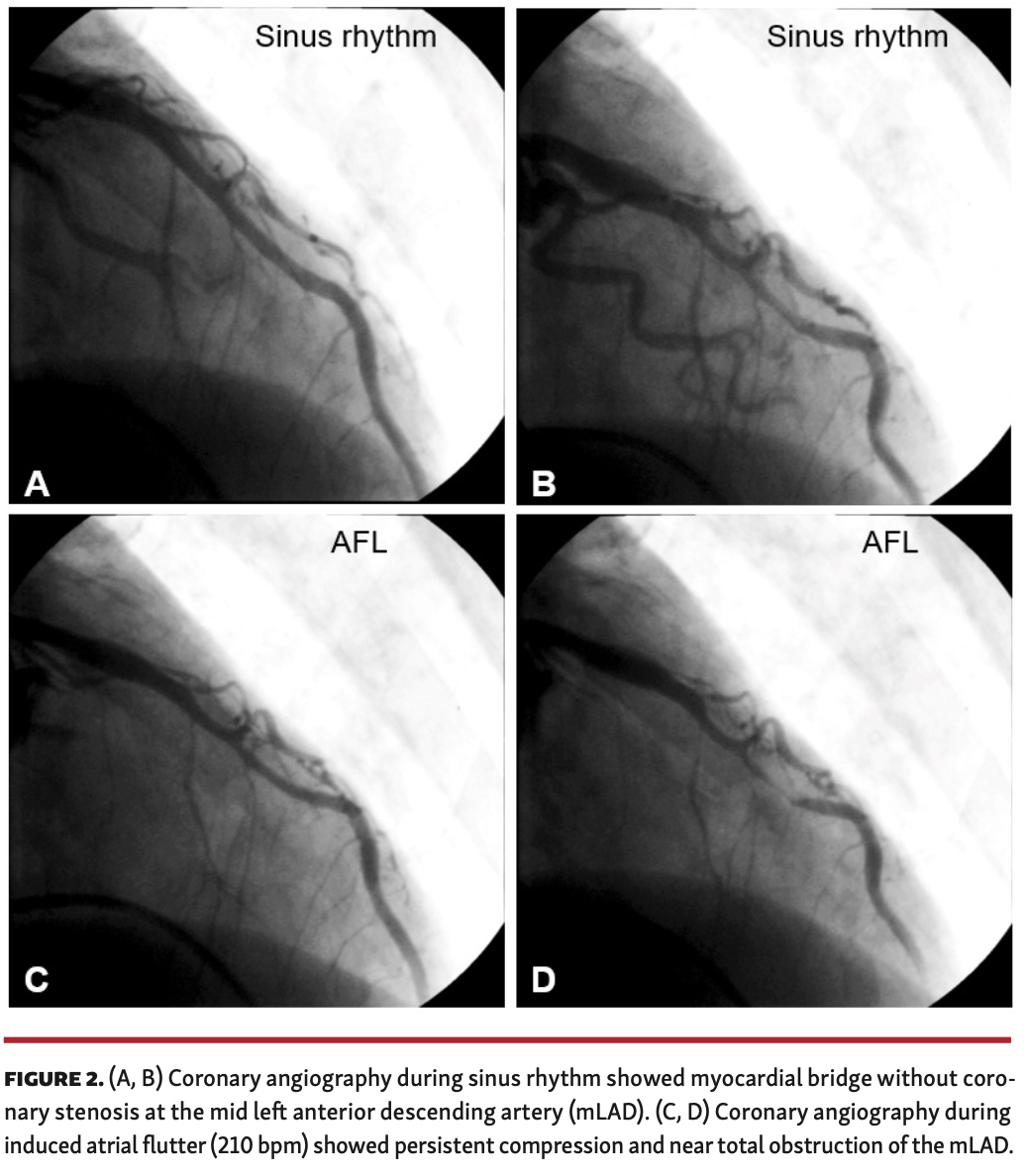
Tachyarrhythmias can lead to chest discomfort, which is usually not severe. However, some patients do complain of severe angina and show evidence of ischemia. As our case study demonstrates, one of the possible mechanisms in these situations is tachyarrhythmia in the presence of an underlying myocardial bridge, resulting in myocardial ischemia due to persistent arterial compression.
Affiliations and Disclosures
†Equal contributors.
From the 1Division of Cardiology, Jeonbuk National University Hospital and Jeonbuk National University Medical School, Jeonju, Korea; 2Research Institute of Clinical Medicine, Jeonbuk National University, Jeonju, Korea; and 3Biomedical Research Institute, Jeonbuk National University Hospital, Jeonju, Korea.
Disclosure: The authors have completed and returned the ICMJE Form for Disclosure of Potential Conflicts of Interest. The authors report no conflicts of interest regarding the content herein.
Manuscript accepted September 16, 2021.
The authors report that patient consent was provided for publication of the images used herein.
Address for correspondence: Lae-Young Jung, MD, PhD, Jeonbuk National University Hospital and Jeonbuk National University Medical School, 20 Geonji-ro, Deokjin-gu, Jeonju, Jeonbuk, 54907, South Korea. Email: lyjung@jbnu.ac.kr
















