Real-Time IVUS-Guided Minimal CRUSH for Bifurcation Stenting: The IM-CRUSH Technique
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
J INVASIVE CARDIOL 2025. doi:10.25270/jic/25.00087. Epub April 15, 2025.
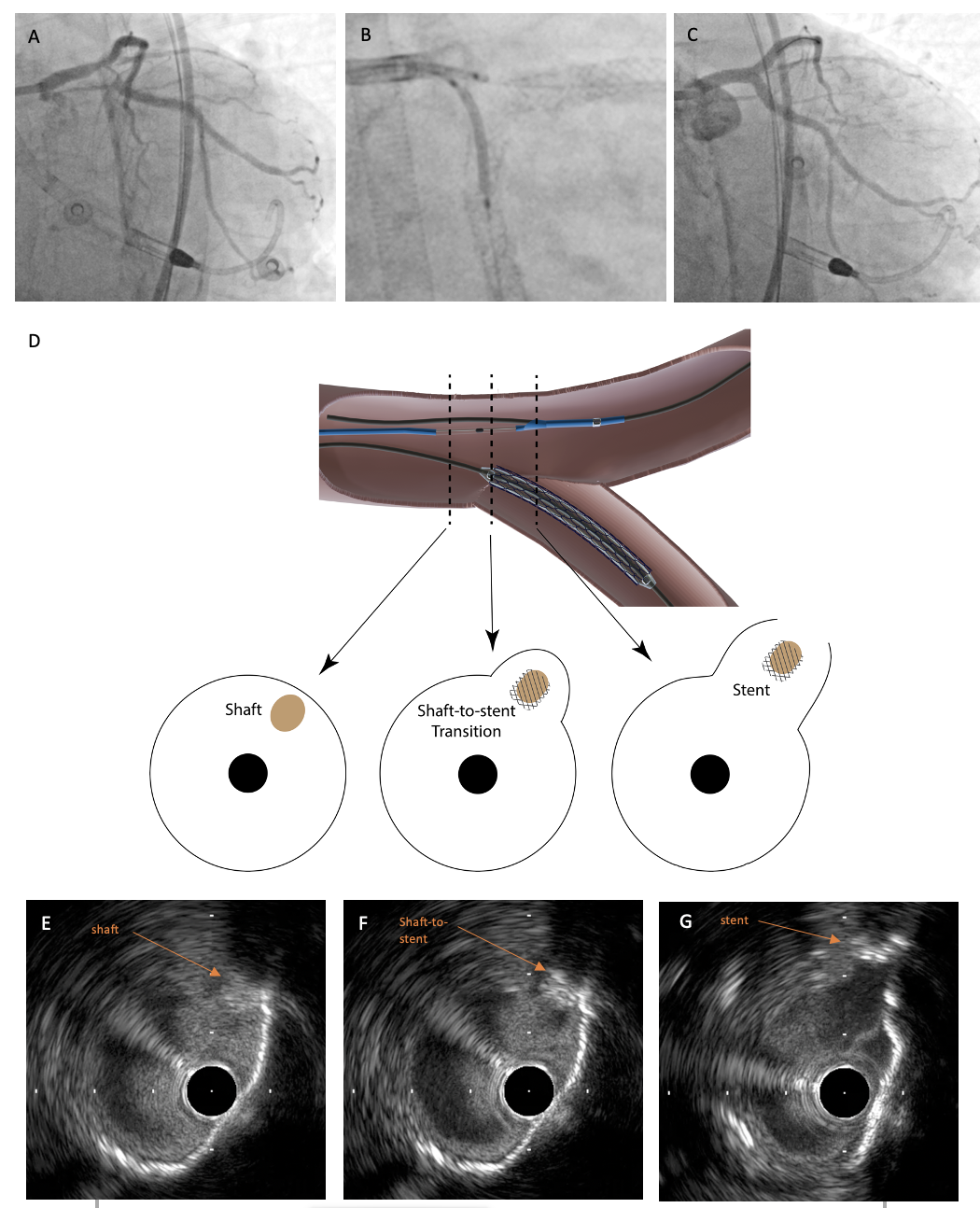
A 72-year-old woman with diabetic nephropathy was admitted for non-ST segment elevation myocardial infarction. She had undergone percutaneous coronary intervention (PCI) to the ostial left anterior descending (LAD) and left circumflex (LCx) arteries 2 years ago. Coronary angiogram showed chronic total occlusion over the right coronary artery and severe stenosis over the proximal LAD. There was also eccentric calcified plaque along the inner curve over the ostial LCx (Figure 1A). Her left ventricular ejection fraction was only 20% to 25%. After discussion by the heart team, supported PCI with left-main (LM) bifurcation stenting using the double kissing (DK) crush technique was planned.
An Impella CP (Abiomed) was inserted over the right femoral artery, and a 7-French guide catheter was engaged into the LM via the Impella sheath. As the patient had undergone previous stenting over the ostial LAD and proximal LCx, minimizing stent protrusion into the left main carina was important. However, there was difficulty in identifying the location of the true LCx ostium because of the eccentric calcified plaque along the inner curve of the carina. Therefore, real-time intravascular ultrasound (IVUS) was used to guide the placement of the LM-LCx stent (Figures 1 and 2, Video):
- After adequate lesion preparation, IVUS (Altaview, Terumo) was parked at the LM-LAD, identifying the most proximal part of the ostial LCx. Under real-time IVUS guidance, the proximal stent edge (shaft-to-stent transition zone) was placed at the true ostium to enable full coverage with minimal protrusion.
- Under real-time IVUS guidance, the LM-LCx stent was deployed.
- The IVUS catheter was withdrawn, while confirming ostial coverage.
- A 4-mm balloon was inserted into the LM-LAD. The LCx stent was post-dilated, if necessary, before crushing the LCx stent. With minimal protrusion of the LCx stent, balloon crossing was smooth. If necessary, a smaller balloon can be used to serially crush the stent.
- Standard bifurcation stenting was undergone using the DK crush technique.
Real-time IVUS guidance can facilitate accurate aorto-ostial stenting.1 In this case, we describe the use of real-time IVUS-guided placement of the side-branch (SB) stent in bifurcation stenting. Conventional fluoroscopic-guided SB stenting risks over-protrusion into the main branch, causing excessive metallic structures in the LM and neo-carina. On the contrary, inadequate protrusion leads to under-coverage of the SB ostium. The use of the real-time IVUS-guided Minimal CRUSH (IM-CRUSH) technique offers solution to these limitations; however, further studies are needed to verify its benefits.

Reference
- Leung C, Ho CB, Wong IMH, Yeung JYK, Chan AKC, Lee MKY. Floating IVUS technique for accurate placement of aorto-ostial stent. JACC Cardiovasc Interv. 2024;17(13):1609-1611. doi:10.1016/j.jcin.2024.05.024
Affiliations and Disclosures
Cheuk Bong Ho, MBBS; Calvin Leung, MBChB; Michael Chi Shing Chiang, MBBS; Esmond Yan Hang Fong, MBBS; Shing Fung Chui, MBBS; Ka Chun Chan, MBBS; Chi Yuen Wong, MBBS; Michael Kang Yin Lee, MBBS
Drs Ho and Leung contributed equally to the manuscript
From the Division of Cardiology, Queen Elizabeth Hospital, Hong Kong SAR.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Ethics statement: The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate.
Address for correspondence: Cheuk Bong Ho, MBBS, Division of Cardiology, Queen Elizabeth Hospital, Hong Kong SAR. Email: bongii2001@gmail.com; X: @RonnieCB_Ho, @drcleung












