Transcatheter Approach to a Dual Drainage Anomalous Pulmonary Venous Return
Key words: left to right shunt, partial anomalous pulmonary venous return, pulmonary hypertension, right ventricular failure, transcatheter repair
A 76-year-old male with history of a ventricular septal defect (VSD) surgically corrected at the age of 16 years presented with worsening palpitation, dyspnea, and pedal edema. Echocardiography revealed left ventricular ejection fraction of 55%, enlarged right atrium (RA) and right ventricle (RV) with severe RV systolic dysfunction, and pulmonary arterial systolic pressure of 60 mm Hg. The etiology of his RV failure remained intriguing considering his asymptomatic course of almost 60 years post VSD repair. Right heart catheterization revealed evidence of shunt physiology with step-up in RA oxygen saturation and mixed venous saturation (Figure 1).
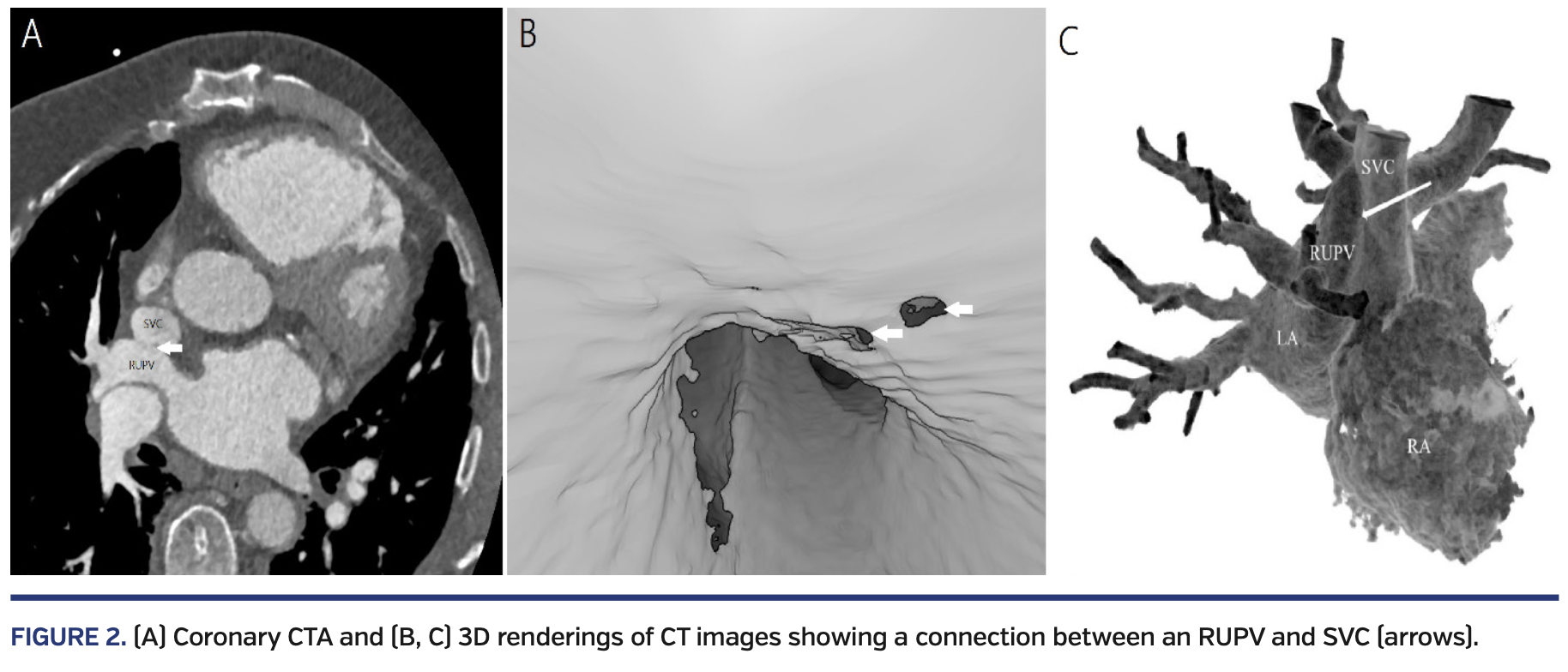
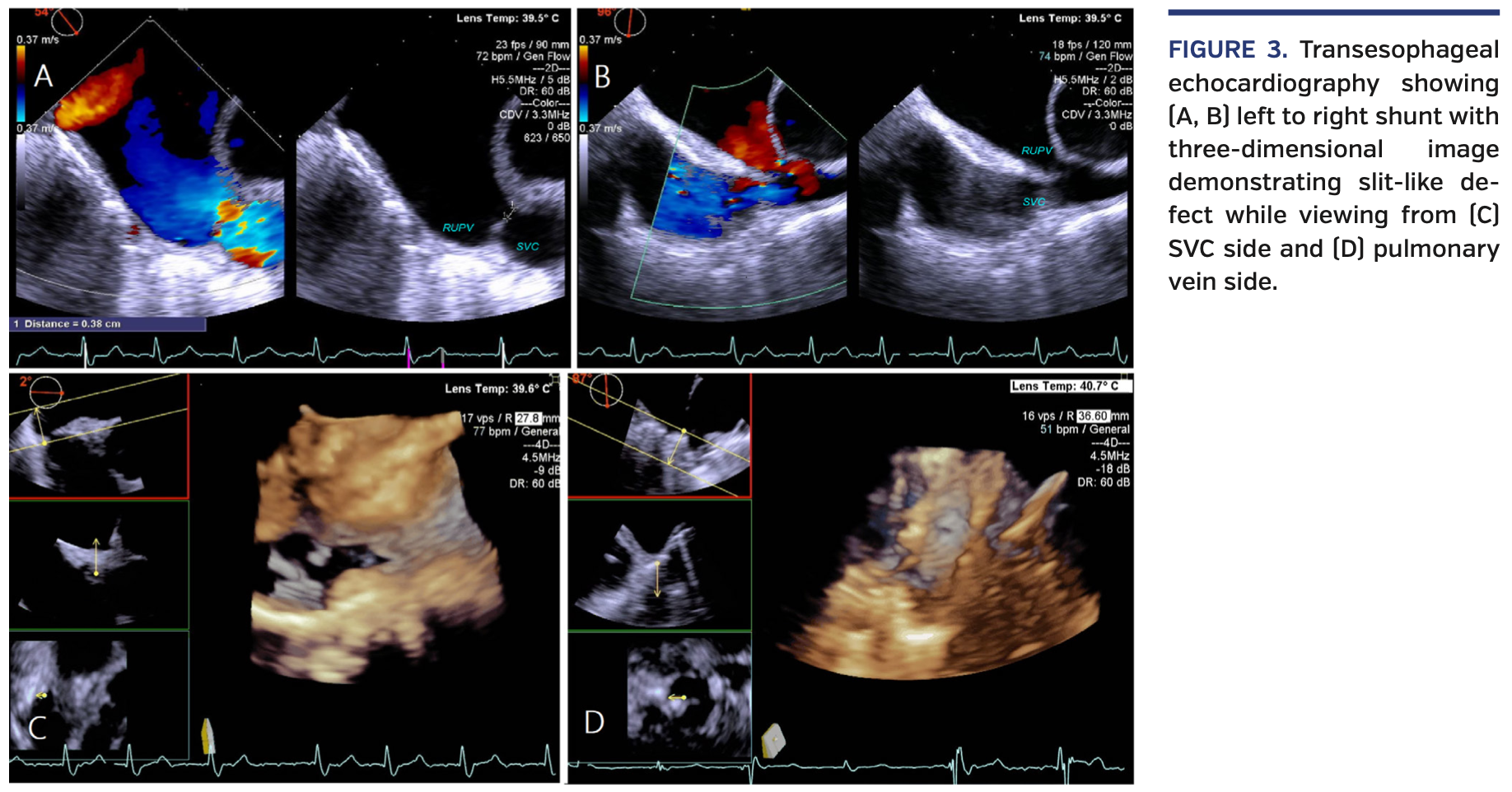
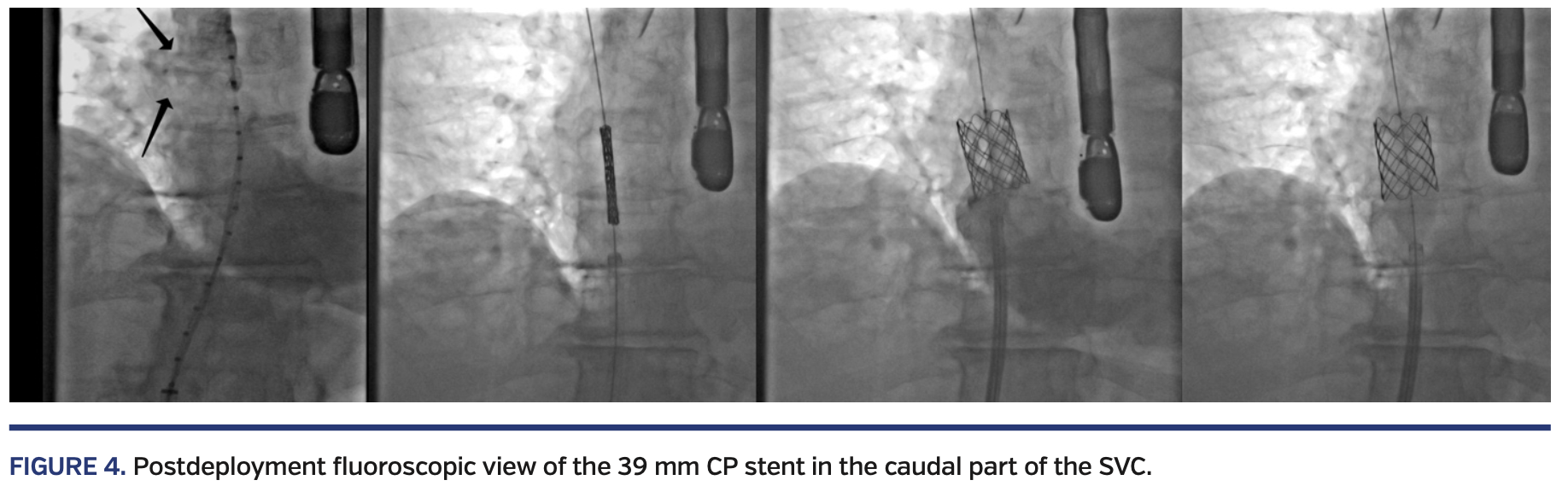
Computed tomography angiography (CTA) revealed partial anomalous pulmonary venous return (PAPVR) with dual drainage from right upper pulmonary vein (RUPV) to the distal superior vena cava (SVC) and left atrium (Figure 2). Given prohibitive surgical risks, we opted for a transcatheter approach. Under transesophageal echocardiography/fluoroscopy guidance, a 39 mm covered CP stent (B. Braun) was deployed at the distal SVC, successfully closing the left-to-right shunt (Figures 3 and 4; Videos 1-3). He had an uncomplicated hospital course and was discharged the next day.
PAPVR is a rare cause of RV failure in adults and can be a diagnostic challenge. It can occur as an isolated defect, but more commonly is associated with other congenital anomalies. Early detection and repair can prevent irreversible RV dilation and failure. Transcatheter approach provides an alternative to surgical repair in patients with prohibitive surgical risks. Surgical closure and robotic repair were reported in other adult cases, but transcatheter approach has been used mainly in pediatric population.
View Supplemental Videos Here.
From the 1Department of Internal Medicine and 2Department of Cardiovascular Disease, the University of Kansas Health System, Kansas City, Kansas; and the 3Department of Pediatric Cardiology, Children’s Mercy Hospital, Kansas City, Missouri.
Disclosure: The authors have completed and returned the ICMJE Form for Disclosure of Potential Conflicts of Interest. The authors report no conflicts of interest regarding the content herein.
The authors report that patient consent was provided for publication of the images used herein.
Manuscript accepted December 12, 2019.
Address for correspondence: Seyed Hamed Hosseini Dehkordi, MD, The University of Kansas Health System, 3901 Rainbow Boulevard Kansas City, KS 66160. Email: shosseinidehkordi@kumc.edu