Guide-Extension Facilitated Antegrade Dissection Re-entry: A Case Series
Abstract: Treatment of chronic total occlusions poses a specific set of challenges above and beyond those encountered in conventional percutaneous coronary intervention. Antegrade dissection and re-entry (ADR) is an established and safe technique with high success rates in experienced centers. CTO techniques frequently require greater-than-usual guide-catheter support and rapid-exchange technologies. Either can be achieved with separate guide extension and a trapping balloon; in this case series of guide-extension facilitated ADR, we highlight the technical advantages gleaned from the use of combined devices such as the TrapLiner guide-extension catheter (Teleflex).
Key words: chronic total occlusion, percutaneous coronary intervention
Treatment of chronic total occlusion (CTO) lesions poses a specific set of challenges1 above and beyond those encountered in conventional percutaneous coronary intervention (PCI) for symptomatic coronary artery disease. The hybrid algorithm for CTO-PCI2,3 was developed to provide a standardized and structured approach and improve procedural outcomes. Antegrade dissection and re-entry (ADR) is an established and safe technique, with high success rates in experienced centers.4 It involves utilization of a dedicated balloon (Stingray; Boston Scientific) to allow re-entry to the true lumen.5 According to the hybrid algorithm,2,3 ADR is the technique of choice in cases with a clear proximal plaque, undiseased distal landing zone free of major sidebranches, and a lesion length >20 mm. The operator circumvents the occlusion by first exiting into the subintimal space. After advancing a wire (eg, Fielder XT-R; Asahi Intecc) or a CrossBoss5 catheter (Boston Scientific), an over-the-wire (OTW) catheter with a blunt tip that is rotated rapidly to facilitate advancement in the subintimal space beyond the occlusion, a wire-based or device-based (Stingray) re-entry is employed to access the distal lumen.
A frequently encountered problem in CTO-PCI is antegrade guide-catheter support. A guide-catheter extension (a mother-and-child system, such as the GuideLiner [Teleflex])6-8 can be employed to optimize support for the treatment of calcified, angulated, or long coronary stenoses.
In addition, CTO techniques frequently require the use of multiple OTW and rapid-exchange technologies. The use of a trapping balloon during CTO procedures reduces procedural time and enhances safety and efficiency. Without the trapping balloon, the use of long or docking wires, or hydraulic exchanges, risks the loss of wire position, damage to the target vessel, and expansion of subintimal space, and ultimately may lead to procedural failure. The TrapLiner guide-extension catheter combines the established benefits of a guide extension with a built-in trapping balloon. We illustrate four cases of guide-extension facilitated ADR.
Case Presentations
Case #1. A 48-year old man presented for CTO-PCI of the left anterior descending coronary artery (J-CTO score, 3) (Figure 1). A previous antegrade attempt with single access by a non-CTO operator was unsuccessful. The antegrade system comprised an EBU 3.5, 7 Fr guide catheter with a Sion blue guidewire (Asahi Intecc) and Corsair microcatheter (Asahi Intecc). A 6 Fr TrapLiner was used from the start of the case in order to optimize support. ADR was facilitated, escalating through Gladius (Asahi Intecc), Pilot 200 (Abbott Vascular), Gaia Third (Asahi Intecc), and Miracle 12 (Asahi Intecc) wires with the utilization of a CrossBoss microcatheter in order to control the subintimal space. The TrapLiner guide extension was advanced into the subintimal space to facilitate delivery of a Stingray balloon and at the same time obstruct antegrade flow in the subintimal space. The “stick and drive” technique using a Hornet 14 guidewire (Boston Scientific) enabled re-entry in the true lumen and successful completion of the case with the deployment of three Ultimaster drug-eluting stents (Terumo).
Case #2. An 81-year old man was admitted for PCI to the native right coronary artery (J-CTO score, 4) following recurrent stent failures in the saphenous vein graft to the posterior descending artery (Figure 2). Retrograde wire escalation (RWE) was unsuccessful in crossing the distal cap. We switched to a TrapLiner-facilitated ADR with the use of an antegrade knuckled Fielder XT wire in the subintimal space followed by CrossBoss catheter and Stingray balloon. An Astato 20 wire (Asahi Intecc) enabled re-entry into the distal true lumen. The guide-catheter extension provided enhanced support through an Amplatz left 1 guide and prevented the expansion of the subintimal space throughout the procedure.
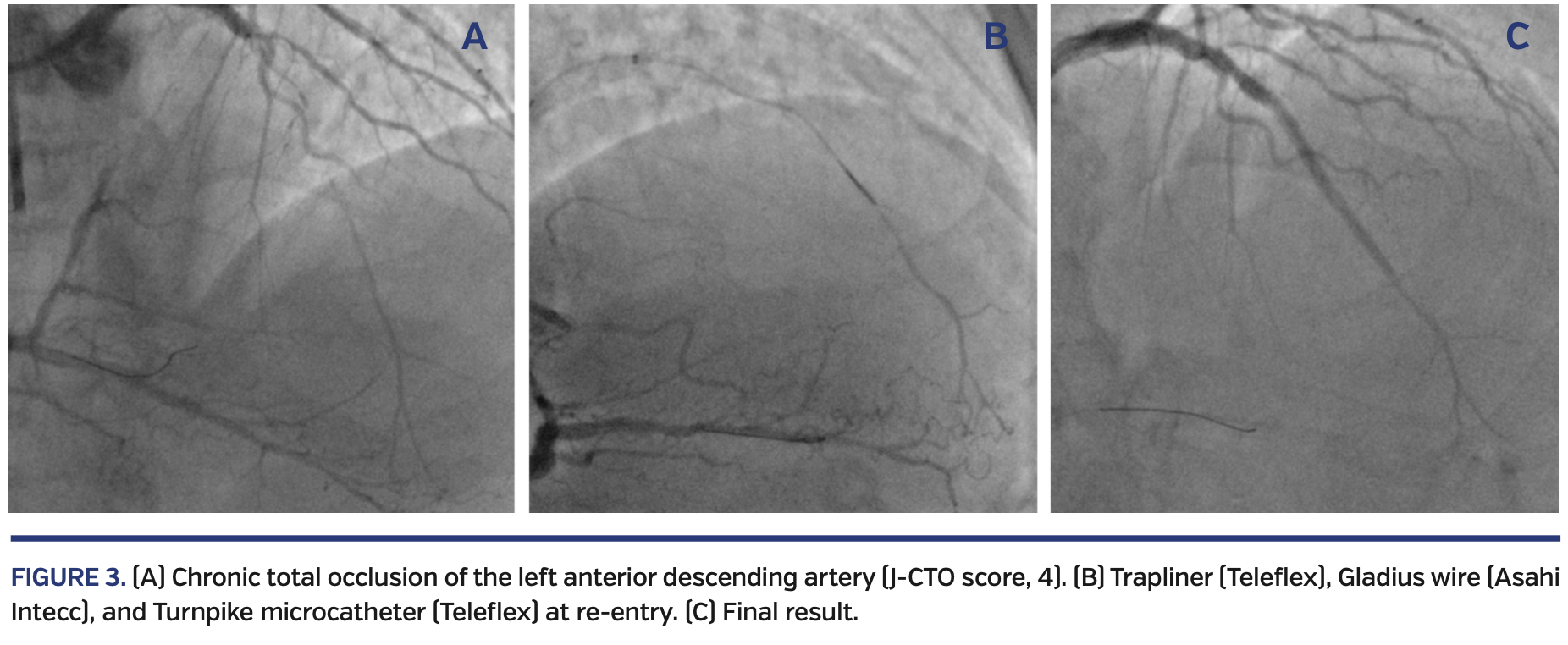
Case #3. A 75-year old man presented for elective PCI to a CTO of the proximal left anterior descending coronary artery (J-CTO score, 4) (Figure 3). Biradial 7 Fr set-up enabled successful antegrade wire escalation (AWE) through the proximal cap with the use of a TrapLiner and a Gladius wire through a Turnpike microcatheter (Teleflex). Rotational atherectomy was performed using a 1.5 mm burr to allow delivery of a Stingray balloon. Subsequently, ADR with the stick and drive technique using the Stingray wire secured access into the distal lumen. The proximal vessel was then treated with intravascular lithotripsy with a 3.5 mm balloon, before treating the proximal to distal vessel with two drug-eluting stents.
Case #4. A 60-year old man presented for PCI to the native right coronary artery (J-CTO score, 3) (Figure 4). An attempted AWE using a Caravel microcatheter (Asahi Intecc), Gaia Third, and Confianza Pro (Asahi Intecc) was unsuccessful, as was a retrograde approach due to lack of interventional collaterals. The proximal cap was crossed into the subintimal space with a Gaia Third wire, enabling balloon dilation of the proximal vessel with a 3.5 x 12 mm non-compliant balloon to lodge a TrapLiner in the proximal segment. A Pilot 200 wire (Abbott Vascular) was used as a knuckle wire, and while using the TrapLiner to secure the subintimal space, distal re-entry was achieved using an Astato XS 20 wire (Asahi Intecc) through a Stingray balloon. Two drug-eluting stents were deployed from distal to proximal vessel.
Discussion
In the four cases described, TrapLiner (Teleflex) guide-catheter extensions were used to achieve three goals:
(1) Increased support. ADR strategies are successful in 63%-78% of cases,4 but the inability to reach the distal target zone or to re-enter commonly leads to failure. Despite the use of supportive guides, additional support is often required to negotiate heavily calcified or long and angulated CTOs in an antegrade fashion. Guide extensions can be advanced further than the guide catheter, potentially intubating the antegrade coronary artery right until the point of exit into the subintimal space. This provides optimized support to counteract at least one of the common causes of ADR failure.
(2) Rapid equipment exchange. When using trapping balloons, the frequent equipment exchange increases procedural length by spending additional time on advancing the monorail catheter to its desired position at the end of the guide catheter and subsequent removal before the guidewire can be used for additional equipment. In complex cases, these exchanges can happen frequently and thus inflate overall procedure time dramatically. A built-in trapping balloon reduces the procedure length by removing the additional steps required with a monorail catheter.
(3) Management of subintimal space by blocking antegrade flow. According to a recent analysis of a United Kingdom registry, subintimal hematoma is responsible for 47% of procedural ADR failures.3 Guide extensions (such as GuideLiner and TrapLiner) can assist in controlling the subintimal space by advancing the catheter to the entry point to the subintimal space and thus reduce antegrade flow, which would otherwise increase the subintimal hematoma. This enhances the chances of successful re-entry into distal true lumen.
We suggest that a combined guide-extension catheter with trapping-balloon is a useful piece of equipment to consider for routine use in the treatment of CTOs. For the reasons outlined above, it is likely to reduce procedure length, increase safety by increasing support, and can even increase success rates by managing the subintimal space, thus enhancing the ADR technique.
From the 1Cardiology Department, St. Thomas’ Hospital, London, United Kingdom; and 2Cardiology Department, Mitera Hospital, Athens, Greece.
Disclosure: The authors have completed and returned the ICMJE Form for Disclosure of Potential Conflicts of Interest. The authors report no conflicts of interest regarding the content herein.
The authors report that patient consent was provided for publication of the images used herein.
Manuscript accepted March 19, 2020.
Address for correspondence: Antonis N. Pavlidis, MD, PhD, Department of Cardiology, St. Thomas’ Hospital, Westminster Bridge Road, London SE1 7EH, United Kingdom. Email: antonis.pavlidis@gstt.nhs.uk
- Galassi AR, Werner GS, Boukhris M, et al. Percutaneous recanalisation of chronic total occlusions: 2019 consensus document from the EuroCTO Club. EuroIntervention. 2019;15:198-208.
- Maeremans J, Walsh S, Knaapen P, et al. The hybrid algorithm for treating chronic total occlusions in Europe. J Am Coll Cardiol. 2016;68:1958-1970.
- Wilson WM, Walsh SJ, Yan AT, et al. Hybrid approach improves success of chronic total occlusion angioplasty. Heart. 2016;102:1486-1493.
- Maeremans J, Dens J, Spratt JC, et al. Antegrade dissection and reentry as part of the hybrid chronic total occlusion revascularization strategy: a subanalysis of the RECHARGE registry (registry of CrossBoss and hybrid procedures in France, the Netherlands, Belgium and United Kingdom). Circ Cardiovasc Interv. 2017;10:e004791.
- Whitlow PL, Burke MN, Lombardi WL, et al. Use of a novel crossing and re-entry system in coronary chronic total occlusions that have failed standard crossing techniques. JACC Cardiovasc Interv. 2012;5:393-401.
- Waterbury TM, Sorajja P, Bell MR, et al. Experience and complications associated with use of guide extension catheters in percutaneous coronary intervention: guide extension catheters in PCI. Catheter Cardiovasc Interv. 2016;88:1057-1065.
- Sharma D, Shah A, Osten M, et al. Efficacy and safety of the GuideLiner mother-in-child guide catheter extension in percutaneous coronary intervention. J Interv Cardiol. 2017;30:46-55.
- Bharadwaj AS, Bhatheja S, Sharma SK, Kini AS. Utility of the GuideLiner catheter for percutaneous coronary interventions in patients with prior transcatheter aortic valve replacement: GuideLiner use for PCI patients with prior TAVR. Catheter Cardiovasc Interv. 2018;91:271-276.