Understanding the Neurobiologic Basis of Pediatric Bipolar Spectrum Disorder Can Help Target Interventions
San Diego, CA—As the knowledge of the role neurobiology plays in pediatric bipolar spectrum disorders grows, so do clinicians’ abilities to use more targeted psychopharmacologic and psychotherapeutic interventions. These interventions were discussed during Psych Congress by Julie A. Carbray, PhD, clinical professor, Pediatric Brain Research and Innovation Center at the Institute for Juvenile Research, University of Illinois at Chicago.
There is now a greater understanding of the neurobiologic basis of pediatric bipolar spectrum disorder. Evidence has shown that brain development differs for patients with pediatric bipolar spectrum disorder, compared to those children who are developing normally.
Studies are also showing the role of circuitry function on clinical impairment. For example, one test used the Penn Emotion Differentiation Task to examine how patients interpret the emotional expression of 40 pairs of faces. It found that patients who had pediatric bipolar spectrum disorder were more sensitive to negative stimuli and had a more excessive reaction in the fronto-limbic circuitry than a control group. Further, those in the control group were more likely to use emotional and cognitive processing areas together than the bipolar group.
Research has also found that there is a decrease in activation in the higher cortical centers in response to affective stimuli for pediatric bipolar spectrum disorder patients. These patients also have greater activation of the amygdale when experiencing negative emotions rather than positive ones. Six brain circuits may have dysfunction in pediatric bipolar spectrum disorder: fronto-limbic, face response, occipito-limbic association, inhibiting impulsive behavior, response inhibition, and cognitive.
As clinicians gain a greater understanding of what the differences in brain circuitry are for pediatric bipolar spec- trum disorder patients, they are able to identify and prioritize the best psycho-pharmacologic and psychotherapeutic interventions for them.
Evidence has shown support for psy- chotherapies such as family-focused approaches, multifamily groups, cognitive-behavioral therapy (CBT), group psychoeducation, dialectical behavior therapy, interpersonal and social rhythm therapy, and systematic care management.
According to Dr Carbray, mood stabi- lizers or second generation antipsychotics can be used as monotherapy or in combination depending on underlying symptomatology. Contingency-based intervention strategies can also be effective.
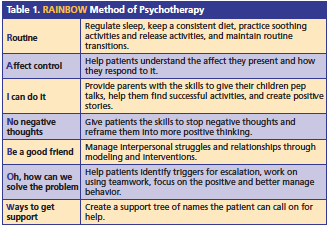
She said that family-focused psycho-therapy targets distinct brain circuitry dysfunction and results in improved outcomes. One such strategy is known as RAINBOW (Table 1).—Jill Sederstrom