How the Medicaid Transformation Project Helps Address the Opioid Epidemic
David Smith, project executive for the Medicaid Transformation Project at Avia, discusses how the opioid epidemic has evolved and how the Medicaid Transformation Project helps transform health care and the related social needs for vulnerable populations.
Please introduce yourself and tell us a little about your background.
I’m David Smith and I’m the Project Executive for the Medicaid Transformation Project (MTP) at AVIA. I’m also a founding member of Third Horizon Strategies, an organization that supports companies with strategic planning responsive to current and expected policy and market environmental conditions.
My expertise lies in the areas of managed care, alternative payment models, and public health. I’ve established several coalitions focused
on these efforts, most notably in the areas of opioid use disorder recovery, individual market stabilization, and consumer-engagement platforms. I’m the co-founder of the Health Care Council of Chicago, a group of Chicago-based health care businesses focused on economic development, system transformation, and social disparities.
I also serve on the board of the Sinai Hospital System, HIMSS North America, and MoreCare, a new Medicare Advantage plan serving Chicago beneficiaries. I’m also on the Founder’s Council of United States of Care, a non-partisan initiative focused on expanding health care access.
Can you briefly detail how the opioid epidemic has changed over the last several years?
In recent years, the opioid epidemic has evolved from addiction to prescription opioids to heroin to today, illicit fentanyl. Along with this evolution of addiction, the health care industry has importantly also evolved. Medical professionals have come to realize that substance use disorder is a chronic condition and are now treating it as such, as opposed to treating it like an infectious disease or like a defect in character.
This shift is imperative because addiction and overdoses are now the leading cause of death for Americans under 50 years old, and only 10% of people receive any kind of substance use disorder (SUD) health care service, leaving 18.2 million Americans in the current addiction treatment gap.
What work is being done to address substance use disorders?
Three broad areas of effort are expanding access to medication-assisted treatment (MAT), integrating substance use disorder treatment in traditional sites of care—chiefly, the ED and primary care—and reforming payment models.
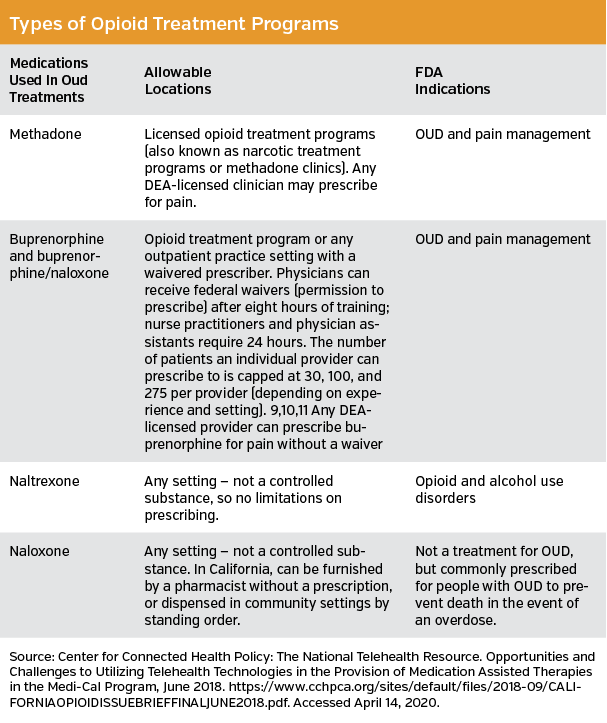
Medicated-Assisted Treatment (MAT) is the use of FDA-approved medications, including Methadone, Naltrexone, and Buprenorphine to treat and manage addiction. This method is used in combination with counseling and behavioral therapies, to provide a whole-patient approach to the treatment of substance use disorders. In recent years, telemedicine is being used to increase access to MAT and has even been shown to have an 11% higher retention rate compared to in person MAT programs.
The second big area of focus is around transforming the emergency department (ED). This looks like integrating substance use disorder screenings for ED patients. Digital solutions enable seamless screening and information-sharing across all ED and health system platforms. Early results show that there can be a 26% decrease in total cost of care if patients are referred out of the ED and into treatment.
The third area is in the realm of payment reform. We are seeing an increasing number of alternative payment model frameworks and pilots seeking to drive greater integration and efficiency within our addiction treatment system aimed at the long-term recovery of people with a SUD. [Editorial note: see accompanying table for types of opioid treatment programs.]
Can you discuss the Medicaid Transformation Project? What is the project? What are each of the phases of the project?
The Medicaid Transformation Project is a collaborative effort to transform health care and the related social needs for vulnerable populations and the nearly 75 million Americans who rely on Medicaid. More than thirty health systems representing 378 hospitals across 28 states have joined the project and committed to implementing innovative solutions, often digitally-enabled, that address challenge areas for this population.
In the first year of the Medicaid Transformation Project, we laid the foundation for health systems and created playbooks in four key areas of action: the emergency department, behavioral health, maternal and infant health, and substance use disorder. In 2020, we’re building off of our work in year one and focusing on areas including community-centered care, maternal and infant health, behavioral health, and chronic disease. We will apply new insights and expertise to enable health systems to accelerate their action, succeed in contract performance metrics, and reduce total cost of care.
What is the importance of this project?
Strategically investing in the Medicaid population can both fulfill a mission and be an opportunity to improve margin. By investing in care improvements for vulnerable populations, healthier communities emerge, and health systems use less expensive resources to deliver more effective care.
Also, our thesis is that working together, we’ll get to results faster and be able to scale successful solutions in parallel, improving care outcomes and results for each health system’s market and its overall communities. We’re already on the path to meaningful impact. After one year in action, MTP has over 140 new projects that are being implemented to improve care for moms and babies, people with mental illness, and those who need care brought closer to them.
What can be learned and taken away from MTP?
Collaborative care models and digital solutions are helping health systems create meaningful change in their communities. One health system has already seen a 22% initial decrease in ED visits in a large Texas county when first responders used a digital solution to intercept people in mental health crises before they were taken to facilities that were not prepared to meet their needs. There are stories like this happening across the 28 states and 378 hospitals in MTP.
Further, the whole basis of the project relies on the importance of improving the financial sustainability and replicability of care models when people and processes can be enhanced through technology.
Pharmacists are a key part in the fight against opioids. How can pharmacists
benefit from MTP?
Pharmacists can work with health systems, payers, and solution companies to develop stronger opioid stewardship programs. They can learn how providers and payers are thinking about deploying SUD strategies across their geographies. They can provide input to solution companies developing interventions focused on SUD and safe opioid prescribing and understand the digital solution landscape to see which solutions they can partner with to improve their practices. They can provide perspective to providers about how to increase access to naloxone, buprenorphine, and naltrexone.
Finally, they can develop community-wide comprehensive strategies to address SUD by collaborating with key stakeholders at health systems, payers, and other community organizations in their communities and geographies.
How do you believe MTP will impact future substance use disorder rates?
By bringing together stakeholders from leading health systems and other health care organizations focused on addressing this epidemic, MTP participants are developing strategies to: better identify individuals at risk for or with an undiagnosed SUD; transform their EDs to better screen, provide brief interventions, and refer to credible treatment (SBIRT); integrate medication-assisted treatment (MAT) in traditional sites of care (eg, primary care, ED); educate their providers on effective SUD treatment options; build networks of peer supports to help individuals engage in treatment; build virtual networks to increase access to MAT; and develop long-term recovery management programs.
Is there anything else you would like to add?
Multiple, converging conditions create reasons for optimism. New payment models will incentivize integrated and coordinated care, as well as a focus on social needs. Rapid innovation has emerged from companies focused on the needs of the vulnerable.
Now is the moment when the business case for better care for the vulnerable aligns with the missions of health systems nationwide. Now is the time to act boldly for the health of all communities.