ADVERTISEMENT
Diabetes Self-Management Education Underused
Boston, MA—Evidence clearly demonstrates the benefits and cost-effectiveness of diabetes self-management education and support (DSME/S). Still, less than 7% of patients with type 2 diabetes are referred to diabetes educators. Researchers are hoping that a new joint position statement from 3 diabetes organizations that outlines when, how, and what to deliver to patients with type 2 diabetes will help increase referrals and participation. The position statement was released during a press conference at the ADA meeting and published concurrently in Diabetes Care, The Diabetes Educator, and the Journal of the Academy of Nutrition and Dietetics.
The ADA, American Association of Diabetes Educators (AADE), and the Academy of Nutrition and Dietetics collaborated on the statement, which provides an algorithm with guidance to health care providers regarding when to refer patients with diabetes to certified diabetes educators and other trained staff for education and support. DSME/S, recognizing that an individual with diabetes is their own primary care provider, refers to the information and skills diabetics need for proper self-care and the support they need to implement those skills and behaviors.
According to David Marrero, PhD, ADA president, Heath Care & Education, who moderated the press conference, the statement is overdue. Dr Marrero, professor of medicine, Indiana University School Medicine, noted that he has lived with diabetes for 40 years and has found that education makes an enormous difference in the lives of people living with and managing diabetes.
“It is high time we took it [education] much more seriously than we take it and that it is applied systematically with rigor,” Dr Marrero told reporters. “It’s horrifying what we’re not doing in education and it has to stop. Diabetes is not just a simple medication disease. It’s a lifestyle condition.”
Margaret Powers, PhD, RD, CDE, coauthor of the position statement, said, “There is confusion as to why diabetes education is needed, when diabetes education should occur, what is needed in diabetes education, and how it should be provided. In fact, this confusion leads to patients not receiving the needed services of diabetes education and support.”
Dr Powers, research scientist, International Diabetes Center at Park Nicollet, and president-elect, Health Care & Education for ADA, continued. “Our goal with this paper was to reduce this confusion and provide clear guidelines and expectations for clinicians and for patients.”
She noted that diabetes education is critical because 95% of diabetes care is provided daily by the patient at home.
One of the statement’s coauthors pointed to research demonstrating that DSME/S improves diabetes outcomes by lowering hemoglobin A1c levels; helping people improve their lifestyle behaviors; decreasing diabetes distress and depression; improving quality of life; and reducing onset and/or advancement of diabetes complications. The latter is a main objective in the care of diabetes, noted Martha M. Funnell, MS, RN, CDE, research scientist, University of Michigan School of Medicine, and past chair for the National Diabetes Education Program. Diabetes education is also cost-effective in decreasing hospital admissions and readmissions, a major focus of the health system.
“We know diabetes education works,” Ms Funnell said. “But we also know the number of people who receive education is alarmingly small.” She cited data from a recent study of people age 18 to 64 years old that showed less than 7% have been to a formal diabetes education program. “While less than 7% is a great A1c number, it’s a really lousy number for the number of people who get education,” she noted.
Barriers to referrals occur when providers don’t know how to refer, don’t think about it during the office visit, don’t have diabetes educators nearby, or don’t believe that education is helpful or valuable.
“Our hope for this position statement is that it will begin to change some of that perception, so that patients do get the referrals they need so they can effectively manage as they go through their lives with diabetes,” Ms Funnell said.
The Algorithm’s 5 Guiding Principles
The diabetes education algorithm provides an evidence-based visual depiction of when to identify and refer individuals with type 2 diabetes to DSME/S. The algorithm relies on 5 guiding principles and represents how DSME/S should be provided through:
• Patient engagement: Provide DSME/S and care that reflects a person’s life, preferences, priorities, culture, experiences, and capacity (eg, engage the patient in a dialogue about current self-management successes, concerns, and struggles)
• Information sharing: Determine what the patient needs to make decisions about daily self-management (eg, avoid being didactic)
• Psychosocial and behavioral support: Address the psychosocial and behavioral aspects of diabetes (eg, assess and address emotional and psychosocial concerns such as diabetes-related distress and depression)
• Integration with other therapies: Ensure integration and referrals with and for other therapies (eg, recommend additional referrals as needed for behavioral therapy, medication management, and physical therapy)
• Coordinated care: Ensure collaborative care and coordination with treatment goals (eg, understand primary care provider and specialist treatment targets)
Specifically, the algorithm defines 4 critical times for assessing the need for DSME/S referral: (1) with a new diagnosis of type 2 diabetes; (2) annually for health maintenance and prevention of complications; (3) when new complicating factors influence self-management; and (4) when transitions in care occur. The statement also provides guidance on the type of information and support patients might need at these 4 critical junctures. The algorithm outlines the content to be taught, roles, and action steps recommended for both the referring provider and for the diabetes educator.
“This intends to provide much more clarity for physicians and other referring providers to know exactly when to refer for diabetes education, as well as what areas of focus and action steps they can do themselves and expect from others,” said Melinda Maryniuk, MEd, RD, CDE, director, care programs, Joslin Diabetes Center.
Reimbursement For An ‘Underutilized Benefit’
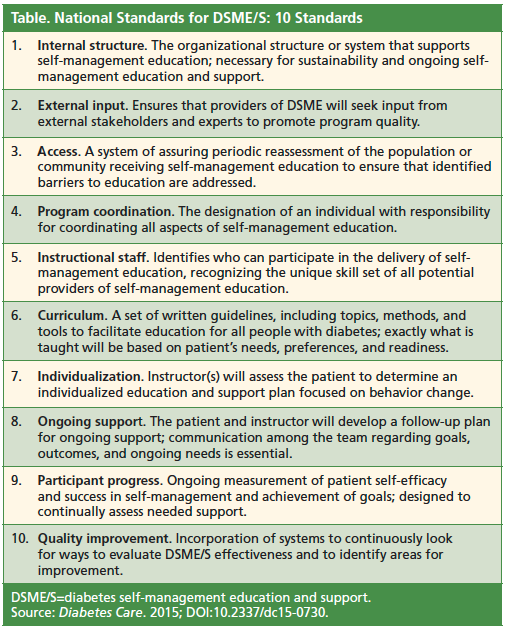
DSME/S is reimbursable under Medicare and from many private payers, according to the coauthors of the statement. In order to be eligible for DSME/S reimbursement, DSME/S programs must be recognized or accredited by the ADA or AADE. Both organizations assess the quality of programs established by the National Standards for DSME/S (Table). Currently, the Centers for Medicare & Medicaid reimburses for 10 hours of initial diabetes education and 2 hours in each subsequent year.
While the reimbursement model is somewhat outdated and needs to be revised, Joan Bardsley, MBA, RN, CDE, FAADE, assistant vice president, Medstar Health Research Institute, and immediate past president, AADE, pointed out that “even though it is reimbursed, people aren’t using the benefit that is there. It’s an underutilized benefit.”—Eileen Koutnik-Fotopoulos