ADVERTISEMENT
CMS rewrite of medicaid Managed Care Rule addresses criticisms
On November 8, 2018, the Centers for Medicare & Medicaid Services (CMS) issued a notice of proposed rulemaking (NPRM) regarding its rewrite of the 2016 final rule updating federal regulations of the Medicaid and Children’s Health Insurance Program (CHIP).
The 2016 final Medicaid managed care rule was an effort to update managed care regulations for Medicaid and CHIP. An article published in May 2016’s First Report Managed Care provided a summary of the key provisions in the final rule, along with comment from the Medicaid experts citing the pros and cons of the new regulations. Among the concerns cited, unease was expressed about implementation of the key provisions of the rule, particularly given the proposed timetables. Other stakeholders also shared concern over the unnecessary administrative burden imposed by the new regulations.
“This rule rewrite is meant to help ameliorate the difficulties states have been encountering since the 2016 rule was published,” said Alexander Shekhdar, vice president of federal and state policy, Medicaid Health Plans of America, Washington, DC.
In response to these concerns and difficulties, CMS issued its proposed rewrite of the managed care rule that was open for public comment until January 14, 2019.
Key Provisions of Managed Care Final Rule Rewrite 2018
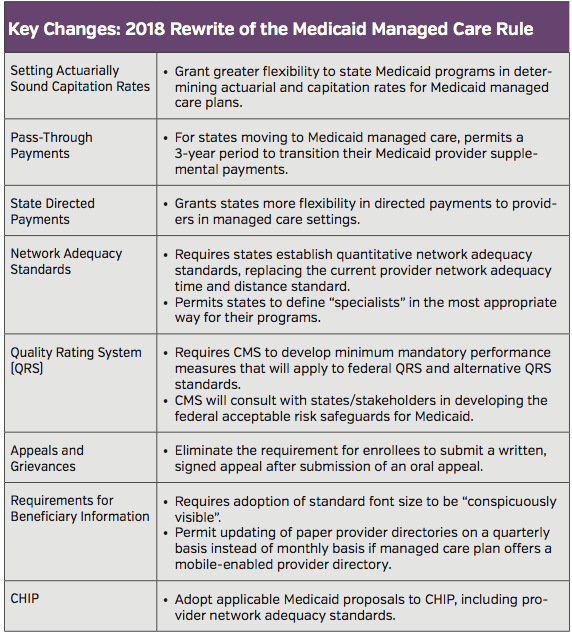
Recommendations for changes to the 2016 final rule were made by a CMS working group that included individual state Medicaid Directors and the National Association of Medicaid Directors (Table).
“In terms of what we see in this current rewrite, that we think is prudent on CMS’ behalf in light of implementation issues like undue administrative burden, are the changes to network adequacy that allow for the potential to move away from time and distance as standards to a more quantitative minimum that takes into consideration other alternative metrics,” said Mr Shekhdar. He added that it permits a more creative approach for states to develop networks, such as telehealth.
While Mr Shekhdar thinks the rewrite is fairly innocuous overall because it is primarily focused on giving states more flexibility while maintaining the bulk of the old rule.; However, he said that some of the other tweaks are positive, such as changes to requirements for marketing materials to beneficiaries — notably not having to update provider directories every month.
For managed care plans in particular, Mr Shekhdar said that the changes to how states can direct payments as supplemental payments will be of interest. “That’s a big concern, or unresolved concern, of managed care plans but the rewrite gives further guidance on where [CMS] expects they’ll go [next] on the use of these two payments streams,” he said.
Margaret A. Murray, CEO, Association for Community Affiliated Plans, sees positive changes in the rewrite include the provision for a 3-year transition period for states transitioning Medicaid populations or services to managed care from fee-for-service providers. “This helps smooth the transition for states that adopt managed care in their Medicaid programs,” she said.
Ms Murray also highlighted the benefit of not having to update paper provider directories monthly, saying that quarterly updates as proposed in the rewrite is less labor intensive and is a “better minimum.”
Not All Positive: Rewrite Still is Lacking
Both Mr Shekhdar and Ms Murray pointed to several areas of in the rewrite that remain problematic for managed care plans. One area is transparency and accountability.
“We would have liked to have seen CMS go further in promoting transparency in rate-setting between states and plans,” said Ms Murray, adding that plans should know what states base their rates on so they can replicate the calculations to determine a rate before it is certified.
Although she acknowledged that CMS has taken a good first step by releasing a Medicaid Scorecard with information on states’ managed care rate resubmissions, Ms Murray emphasized that only 38% of base rate certifications were submitted before contracts began.
“We are eager to see continued improvement in this area,” said Ms Murray. “CMS could even take the transparency a step further by setting up a real-time, state-by-state dashboard which would show when CMS received states’ rates for review, the status of reviews currently under way, and when reviews were concluded.”
For Ms Murray, the rate-setting process is foundational to the operations of plans and will get the most scrutiny in the rewrite of the final rule.
Mr Shekhdar mentioned an aspect of the 2016 final rule that is not addressed in the rewrite, one he wished had been eliminated, is the provision on the medical-loss-ratio in the 2016 rule that mandates all payers to spend at least 85% of their Medicaid revenue on medical care.
Another issue Mr Shekhdar wished had been addressed in the rewrite that was also not addressed initially, is payment policies for plans for mental health and substance use disorders. The Medicaid Institutions for Mental Diseases (IMD) exclusion prohibits the use of federal Medicaid dollars to treat patients with these disorders in residential treatment facilities larger than 16 beds. While Mr Shekhdar recognized that CMS can’t change the statute and states can apply for a new waiver that provides some guidance on how to pay for these patients, he still wishes this issue had been touched on.
“Even though [the waiver] provides some latitude on how plans can be paid for IMD, which is advantageous especially in light of the current opioid epidemic, it wasn’t addressed in the Medicaid managed care final rule,” said Mr Shekhdar.
Another issue that both Mr Shekhdar and Ms Murray raised was the quality rating system in the rewrite. Calling it “attention-grabbing,” Ms Murray said that her organization “supports the use of standardized measures of quality that cut across as much of the Medicaid program as possible to allow for apples-to-apples comparisons,” she continued. “It’s crucial to use variations among state Medicaid programs as an opportunity for learning and improvement.”
Mr Shekhdar referred to the quality rating system as interesting. “It still depends on outlining or rolling out a new quality rating system for Medicaid, which itself would necessitate a new NPRM,” he said. “But [CMS] also signals the ability of states to perhaps have an alternative to whatever the federal standard is.”
According to Mr Shekhdar, the rewrite is overall positive in terms of granting states more flexibility, which he thinks will “cascade down in terms of implementation.”
Given these and other large issues that remain challenging under the Medicaid managed care rule, Mr Shekhdar thinks that there will be future opportunities to revisit the rules effectiveness as they are implemented and their practical implications become more manifest.























