ADVERTISEMENT
Chronic Pain Management Is Complex
San Antonio—The Institute of Medicine estimates that chronic pain affects about 100 million American adults—more than the total affected by heart disease, cancer, and diabetes combined. Pain also costs the nation up to $635 billion each year in medical treatment and productivity loss. Unfortunately, there is no nationally accepted consensus for the treatment of chronic pain; concerns about drug misuse, diversion and addiction, and regulatory scrutiny further hinder optimal pain management.
During a session at the AMCP meeting titled Challenges and Opportunities in the Management of Chronic Pain, Chris Herndon, PharmD, associate professor at Southern Illinois University Edwardsville School of Pharmacy, reviewed current concepts in the treatment of chronic pain and strategies for reducing controlled substance abuse.
Dr. Henderson started the session with a brief overview on the scope of the chronic pain problem in the United States. The prevalence of pain is staggering, with the majority of individuals suffering from pain in any joint and low back pain. He noted that chronic pain also produces widespread disability. Patients with low back pain, knee pain, headache, or neck pain report being unable to perform basic daily activities due to their pain. While chronic pain also affects patients in all age ranges, nearly 60% of patients aged ≥65 years report chronic pain lasting 1 year or longer.
He described the pain assessment PQRST method, which is a series of questions designed to facilitate analysis of a patient’s symptoms and history. This tool can help clinicians in determining an appropriate course of treatment:
• P: Any precipitating or palliating factors?
• Q: What is the quality of the pain?
• R: In what region of the body? Does it radiate to other locations?
• S: How severe is the pain? Sites of pain?
• T: Is there a temporal relationship?
• U: Medications previously utilized?
With chronic pain so prevalent, Dr. Henderson said how pain is classified is important because there are many overlapping complaints. He also reviewed common chronic conditions under the umbrella of nociceptive pain (eg, coronary artery disease, osteoarthritis, and rheumatoid arthritis), neuropathic pain (eg, central post-stroke, nutritional neuropathies, and peripheral neuropathies), and mixed pain (fibromyalgia, myofascial pain).
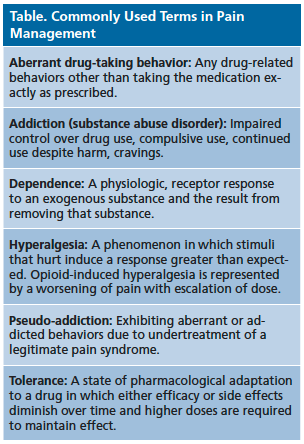
Along with classification of pain, Dr. Henderson said it is important to correctly define commonly used terms in pain management. He reviewed the definitions of terms that are often misunderstood by patients and some healthcare professionals. These terms are defined in the Table.
He continued the presentation with a discussion of current-based treatment guidelines for the management of chronic pain conditions. For example, management of chronic low back pain can include physical therapy, manipulation, acupuncture, massage, and surgical interventions. The American College of Physicians and the American Pain Society released a joint clinical practice guideline on the diagnosis and treatment of low back pain in 2007, which includes the following pharmacological agents:
• Acetaminophen
• Nonsteroidal anti‐inflammatory drugs
• Opioids
• Antidepressants
• Anticonvulsants
• Benzodiazepines and skeletal muscle relaxants
• Topical therapy
The diagnostic criteria for fibromyalgia was also highlighted. Symptom assessment includes evaluation using the Widespread Pain Index and Symptom Severity Score. Recommendations for pharmacological treatments of fibromyalgia from the European League Against Rheumatism include antidepressants, tropisetron, pramipexol, pregabalin, and tramadol.
Dr. Henderson concluded the presentation underscoring the importance of developing policies for the treatment and management of chronic pain. Policies should address the following situations:
• Acute pain with or without risk factors for abuse
• Emergency department or hospital follow-up appointments
• New patient establishing care
• Established patient transitioning from acute to chronic pain
Input from all practice stakeholders is needed for these policies, including medical assistants, nurses, lab technicians, and providers, according to Dr. Henderson.