The Rise of Value-Based Drug Pricing: Is It Effective?
 More payers and pharmacy benefit managers (PBMs) are entering into value-based agreements for prescription medications in an effort to curb rising drug costs and share the risk with pharmaceutical companies, but whether these types of agreements will have their intended effect is still unclear.
More payers and pharmacy benefit managers (PBMs) are entering into value-based agreements for prescription medications in an effort to curb rising drug costs and share the risk with pharmaceutical companies, but whether these types of agreements will have their intended effect is still unclear.
“Clients are looking for new ways to reign in wasteful drug spending and justify higher cost entrance,” Eileen Pincay, BS, RPh, senior pharmacy consultant for the Segal Group’s national pharmacy benefits practice, said. “We are seeing more PBMs propose these new concepts (and) we’re just beginning to evaluate and negotiate them for our clients.”
PBMs are not the only stakeholders trying to find a way to tie value to the price of a drug, experts report seeing greater interest among payers and drug manufacturers as well.
Earlier this year, for example, Cigna announced that it had entered into two value-based contracts with Amgen and Sanofi/Regneron that would modify the cost of cholesterol-lowering drugs Repatha (evolocumab; Amgen) and Praluent (alirocumab; Sanofi/Regneron) based on patient outcomes. It’s been reported that Aetna, Humana, and UnitedHealth have also entered new value-based drug pricing arrangements.
“I would say some of these initiatives are being pushed by the payers and some are pushed by pharma,” Jason Gomberg, a consulting actuary at Milliman, said in an interview.
Medical organizations are also offering their support to the concept. In November, the American Medical Association (AMA) announced the adoption of a policy supporting value-based drug pricing.
“The policy’s adoption adds to the AMA’s long-standing support for market-driven mechanisms to control pharmaceutical costs, while recognizing that improvements need to be made to ensure that the prescription drug market operates efficiently and effectively,” the announcement read.
Continued on next page
Rationale For Value-based Drug Pricing
The rising cost of specialty drugs and an industry-wide movement toward more value-based initiatives has helped drive the concept of value-based drug pricing.
“Both PBMs and payers are committed to affordability and sustainability of drugs, so I think this value -based pricing idea is great in that we want to hold Pharma accountable,” Ms Pincay said. “We do want them to be included in the risk sharing, because as of right now, they are getting paid regardless of any health outcomes.”
According to some, the advantage of these types of arrangements is that it could help drive competition among manufacturers leading to more affordable pricing models.
“In theory, I mean I think the reason why a lot of people are pursuing it is because they think they can control the increases in drugs a little better—so, maybe it will help,” Mr Gomberg said.
However, David Blumenthal, MD, the president of The Commonwealth Fund, explained that he does not believe value-based drug pricing is a viable strategy for every situation.
“Value-based pricing is not a substitute for competition,” he said. “The best way to manage the drug market if you believe... in competitive markets, is to have products from multiple providers that compete for consumers. That’s the reason why we have generic drugs. That’s the reason why drug prices in many generic markets have become pretty low over time.”
For example, Dr Blumenthal said that drugs like penicillin are very versatile and effective and serve a valuable role in patient care, in part, due to their affordable cost.
“If you price these drugs according to the value, it would be extremely expensive and unaffordable and much less used and the public would get much less benefit for it,” Dr Blumenthal explained.
However, he also noted value-based drug pricing could play a role in situations where drug manufacturers essentially have a monopoly on a product, whether it is because of a patent or due to exclusive rights granted by the government.
“The rationale I see for value-based pricing here would be of the equivalent of the public regulatory commission,” Dr Blumenthal said. “We’d be saying collectively in the absence of a market, this is the best way to price.”
It may not be the only pricing strategy in these types of scenarios though and Dr Blumenthal emphasized that other strategies need to be considered as well.
“It’s an artificial pricing mechanism,” he said. “There are potentially other artificial pricing mechanisms that one could use and it’s in that range of pricing mechanisms that you have to balance one against the other.”
Continued on next page
Details of the Deal
For those payers and manufacturers who have chosen to enter into value-based drug pricing arrangements, there is no set structure to the arrangements.
In some of the arrangements, an initial price is set for the drug based on value and that is what gets paid. In others, there is a risk-sharing component to the arrangement where the price is determined based on the value seen among a patient group.
“The pharmaceutical company shares risk with the insurer and if there isn’t benefit, the price goes down or maybe there’s no compensation at all,” Dr Blumenthal said.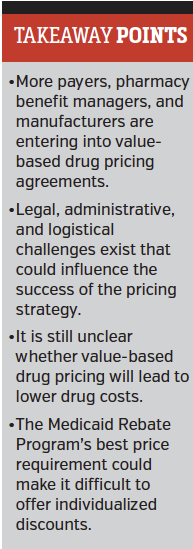
According to Mr Gomberg, there is no typical structure to how value is determined. Some deals are even pricing the same drug at different price points based on the indication it is being used for. In these designs, insurers may be willing to pay a higher cost for a disease state where the drug is more effective.
“There are a lot of flavors to what these can look like,” he said, adding that value-based pricing arrangements could also be established between hospital systems and manufacturers.
It is still unclear just which type of structure will be most effective. Dr Blumenthal explained that the Commonwealth Fund is trying to collect more information about the current applications of value-based drug pricing to learn more about what works well and what does not.
Ms Pincay said that PBMs and payers should evaluate the potential deals by considering the utilization in their patient population, the utilization management strategies they have in place to monitor outcomes, and the level of disruption it could cause to implement the deal.
More questions than answers?
The optimal structure for value-based drug pricing arrangements is not the only question that remains in the emerging market. Experts say value-based drug pricing is a strategy that is still in its infancy and still has many variables, including whether or not value-based drug pricing will actually result in savings to the health care system.
Ms Pincay explained that one of the challenges is that it is still not clear how outcomes will be measured or whether companies are seeing the value they hoped would be there.
“The details of the outcomes are really hidden, so there is no way to monitor or verify success or failure,” she said.
Contracts based on value also can introduce administrative hassles for payers, who need to have effective means in place to track and evaluate patient outcomes.
It is also unclear whether there will be cost savings under these arrangements, and if there are, whether those cost savings will be reinvested into the program or passed on to patients.
Ms Pincay said she thinks the idea behind value-based pricing is great and there is value in pursuing these type of deals; however, it is still so new and the outcomes are difficult to measure making it difficult to truly evaluate the strategy overall.
In addition to lingering questions about the effectiveness of value-based drug pricing, experts say there are also legal hurdles to overcome.
The first, Mr Gomberg explained, is that there could be legal concerns if the contracts are based on metrics that are not specifically outlined on the FDA label.
“For instance, a statin may lower cholesterol, but we may not have linked cholesterol to overall mortality yet,” he said.
There is also the issue of the Medicaid Rebate Program’s best price requirement, which requires drug manufacturers to give the Medicaid program the lowest price they are offering in the drug marketplace.
Mr Gomberg said this requirement could make it difficult to discount each person individually based on their outcomes. For instance, if a deal was structured where a payer did not have to pay for a drug if it didn’t work on a particular patient, that could create a 100% discount, which would then need to be passed down to Medicaid patients.
Despite the challenges, experts said they expect to see more value-based drug pricing arrangements entering the market.
While the complexity of the arrangements and data requirements may be a challenge for some of the smaller payers, Mr Gomberg said he believes the industry will see more of these agreements between manufacturers and the larger health plans and PBMs.
“I don’t see why they are going to stop,” he said.
Whether value-based drug pricing will be the answer to keeping rising drug prices down remains to be seen.
“I think it has to be judged on whether it produces an affordable result for individuals in the health care system and one that adequately balances the interest of the consumers and suppliers,” Dr Blumenthal concluded.




















