ADVERTISEMENT
Policy Change: The Impact of 340B Cuts on Hospitals
In November 2017, the Centers for Medicare & Medicaid Services (CMS) issued its Hospital Outpatient Prospective Payment System final rule that reduces the payment rate for certain Medicare Part B drugs purchased by hospitals through the 340B program. Under the final rule, Medicare payments for outpatient drugs to hospitals in the 340B program will be cut by 28.5%, which represents an estimated $1.6 billion in funding.
Although CMS states that such cuts will benefit patients by lowering out-of-pocket expenses and giving patients more choices, a growing coalition of health care groups, patient groups, and members of Congress are pushing back on what they see as the opposite: such reductions will come at a cost to patients and hospitals, particularly rural hospitals, that serve them under the 340B program.
“If the regulation is allowed to go into effect, it will force many 340B hospitals to reduce services, close service sites, and potentially lay off clinicians and other employees,” said Richard Sorian, senior vice president, 340B Health, an organization representing more than 1300 public and private nonprofit hospitals and health systems in the 340B program.
In an effort to stop the regulation from taking effect on January 1, 2018, health care stakeholders against the regulation are lobbying hard through legislative action and legal challenges to ensure cuts are not made to the program. A bipartisan bill (HR 4392) to block the cuts currently has 165 sponsors in the House, and coalition of hospital associations is challenging the legality of the Department of Health and Human Services to make the changes to the program.
Others health care stakeholders, however, see the regulation as overdue pointing to the expansion of the 340B program beyond its original intent. These stakeholders, among them pharmaceutical companies and some oncology groups as well, focus on the misuses of the program.
“My major objection is that this is a misuse of the program in regard to how it was intended; it was intended to shore up safety-net institutions, so that it took care of poor and indigent patients,” said Peter B. Bach, MD, director of the center for health policy and outcomes, Memorial Sloan Kettering Cancer Center, in an interview with Medscape in 2014.
Sayeh Sander Nikpay, PhD, assistant professor of health policy at Vanderbilt University, who finds merit on both sides of the issue as discussed in an article published in Health Affairs, also emphasizes the importance of updating the definition of what constitutes a safety-net provider to ensure that the program is actually serving the population for which it was designed.
“The response from hospitals and policy makers [to the CMS final rule] has been swift,” she said, “which suggests a need for precision policy making in order to redirect the program back to its original purposes while not endangering safety-net providers.”
Redirect Program to Original Purpose
Proponents of more oversight and regulation to the 340B program cite the expansion of hospitals and centers in the program. Created in 1992, the program is intended to help low-income and uninsured patients pay for outpatient drugs by giving the safety-net hospitals that provide care for these patients deep discounts on these drugs. Since 1992 the number of hospitals and centers participating in the program and qualifying for 340B discounts has grown substantially, with about 40% of US hospitals now buying drugs through the program. One main criticism of this expansion is that many of these hospitals who now qualify for the 340B discounts are not using the discounts as intended (to offset the high cost to patients) but to generate profits.
A strong proponent of this view is from oncology groups who report a substantial shift in oncology services from physician offices to the hospital outpatient setting as more and more 340B hospitals expand into providing oncology services. This shift has generated large profits for hospitals, as documented in a recently published report showing a 49% increase in the average profit margin on oncology drugs purchased by hospitals through the 340B program in 2015. Commissioned by the Community Oncology Alliance, and conducted by the Berkley Research Group, the report details the increasingly large role 340B hospitals are playing in delivering oncology care, the large financial benefits generated by delivering oncology services through the hospital outpatient setting vs the physician office, and the overall affect this is having on health care costs in general and increased cost to patients in specific areas.
Article continues on page 2
In the interview with Medscape, Dr Bach highlighted the impact of this shift from providing oncology services from the doctor’s office to the outpatient hospital setting. By acquiring physician practices that provide oncology services, hospitals are able to make significant profits by the larger reimbursement for oncology drugs they receive under the 340B program. “Say the average chemotherapy from UnitedHealthcare given by a doctor’s office gets reimbursed about 22% above sale price. Once that same office in the same location with the same staff and the same doctors gets purchased by a hospital, they are making 140% of the sale price,” he said.
This type of markup not only adds to the total cost of health care, he said, but also increases the cost of care to patients. One key finding of the Berkley Research Group report was the upward pricing pressure on oncology drugs driven primarily by the increasing statutory discounts and rebates on oncology drugs paid by manufacturers through the 340B program. These discounts and rebates nearly tripled between 2010 and 2015, from $1 billion in 2010 to $3 billion in 2015 and accounted for 7.4% and 14.4%, respectively, of the total gross sales for these drugs.
Saying that oncology drugs, like most specialty drugs, incur coinsurance costs to patients, Dr Bach said that the out-of-pocket costs to patients will go up. “The out-of-pocket cost for patients is indexed to the price of the drug, and that price is not what the doctor paid, which will be discounted under 340B,” he said. It is what the insurer pays.”
Regulation Will Cut Needed Costs and Services
Opponents of the regulation essentially argue that that the substantial cuts to Medicare payments for outpatient drugs to hospitals in the 340B program will adversely affect patients by, among other things, eliminating important services that these hospitals can provide for low-income patients.
“Hospitals that participate in the program utilize the savings they achieve by these reduced costs to expand services for low income and rural patients to provide free or reduced cost drugs but also other services that support patients and their care,” said Mr Sorian.
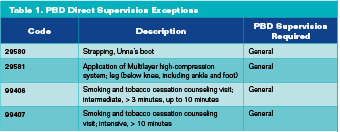
Examples of how hospitals use the savings they achieve under the 340B program to provide services for uninsured and low-income patients were recently provided by The Association of American Medical Colleges, one of many health care groups against the cuts to the 340B program (Table 1).
 As to the charge that the increasing discounts and rebates mandated through the 340B program are pushing the costs of drugs higher, Mr Sorian emphasized that no evidence supports this. “Drug prices are going up because drug companies have increased their prices and set prices on new drugs at very high levels,” he said. “There is absolutely no evidence that the discounts that drug companies are required to offer have an upward impact on the cost of drugs.”
As to the charge that the increasing discounts and rebates mandated through the 340B program are pushing the costs of drugs higher, Mr Sorian emphasized that no evidence supports this. “Drug prices are going up because drug companies have increased their prices and set prices on new drugs at very high levels,” he said. “There is absolutely no evidence that the discounts that drug companies are required to offer have an upward impact on the cost of drugs.”
Mr Sorian also dismissed the idea that the discounts offered through the 340B program are making it necessary for drug companies to raise drug costs. “The total discounts for 340B facilities, hospitals, and clinics in 2015 was $6 billion; that is 1.3% of total US drug sales,” he said. “In contrast, the drug companies have spent four times that amount on marketing and advertising their products.”
Under the final rule, Medicare payments for outpatient drugs to hospitals in the 340B program will be cut by 28.5% beginning on January 1, 2018. Representing an estimated $1.6 billion in cuts, opponents of the program changes argue that such cuts will cause a reduction in serves to low income and uninsured patients and will do little to stem the increasing cost of drugs. Proponents of the changes point to the need for better regulation of the program, citing the expansion of 340B hospitals beyond the original intent and the incentives of hospitals to profit from the program.




















