Improving Population Health Management to Achieve the Triple Aim
 An interview with Virginia Gurley, MD, chief medical officer at AxisPoint Health.
An interview with Virginia Gurley, MD, chief medical officer at AxisPoint Health.
Patient-centered, personalized health care is becoming more and more important to clinicians, hospitals, and health system—is this something payers also need to be focused on?
Absolutely. Making health care more personalized and tailored to the individual is the path to realizing the Triple Aim of improving health outcomes, reducing costs, and optimizing the patient experience.
What population health strategies can payers employ to help achieve the Triple Aim?
Payers should think about their data, the analytics they use to understand that data, and how to make it actionable. Payers also should think about implementing payment methodologies that lead to improvements in quality and positive health outcomes. As well, payers should ensure they have the tools in place to look at their entire population and target the most impactable members for interventions. Payers will need collaborative partnerships with providers and community service organizations to ensure that members have access to the care and services they need, and that all parties are working together to achieve those Triple Aim goals.
Care management typically focuses on core, higher-cost disease states—is a more holistic approach necessary to broadly reduce costs and improve care?
Yes. At AxisPoint Health, we’ve taken a condition-agnostic approach. Instead of focusing on the Big 5 chronic diseases, we look at universal processes of care to support those members with chronic conditions beyond the Big 5. For example, we look at whether members are adherent to their medication regimen, and if not, deliver interventions to support the member getting their medications and remembering to take their medications as prescribed. Similarly, we also help members who have been in the hospital postdischarge so that they avoid unnecessary readmissions. These processes of care aren’t condition-specific, but support member health and cost reduction across a population. By addressing barriers to care, that supports achievement of the Triple Aim.
Can you explain what AxisPoint’s CarePoint is and how it works? Can you also explain what Analytix is and how this system works to help management of high-cost patients?
CarePoint and Analytix work together to enable payers to engage and intervene with their impactable members.
CarePoint is best described as innovative and analytically-driven condition and case management services that provide precision focus and quantified results for payers and other risk-bearing organizations who seek to drive targeted member engagement, improve health outcomes, and reduce medical expense.
CarePoint takes the most current and relevant biometric, symptom, lab, pharmacy, claims, and nontraditional consumer data and makes it relevant, actionable, and impactful. This data is leveraged from a continually updated data warehouse to create a comprehensive, real-time 360 degree view of each member. Analytix, our predictive intelligence service, uses this data to identify the members with the most clinical immediacy, cost impact, and opportunity to maximize results—that is, the most impactable members. Once identified, Analytix prioritizes each identified member by weighing multiple variables to establish a unique ranking score based upon their condition and how easy their individual issue is to prevent or resolve. Next, Analytix assigns each member to the most clinically appropriate care track (medication adherence, visit compliance, readmission avoidance, monitoring, or palliative/end of life) based on what is at the root cause of their health issue. We continually stratify and re-prioritize members, applying a new ranking score, as we receive new data points to maintain relevancy. This approach is quite different, as traditional disease management programs have looked at individual conditions, and not the whole person.
Story continues on page 2
Once identified and prioritized, Analytix places targeted members on care tracks that transcend conditions and comorbidities and takes into account their behavioral and social needs. By focusing on care tracks that cross all conditions, we are able to reach opportunities for clinical impact that would have been missed with a traditional condition-only approach.
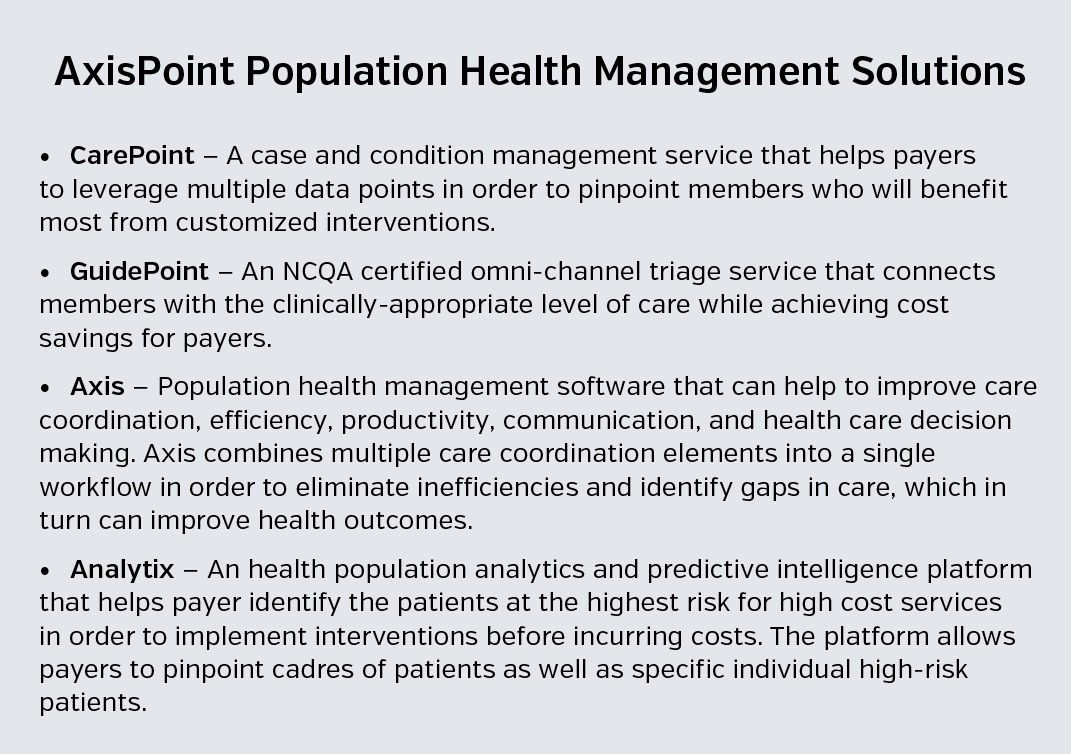
Analytix matches each member to a multi-disciplinary, condition-agnostic care team whose skill set matches the member’s specific clinical and behavioral health needs. The care team uses AXIS, our advanced care management software, to implement focused, pulsed touches that drive positive behavior change for maximum effectiveness. We reach the member across communication channels to engage with them where and when it creates the most value. Compass, our digital health experience, creates a social, interactive experience to support the member and their support circle around the clock to drive behavior change and generate success in their health.
Our targeted, dynamic intervention model stands in stark contrast to the low impact, transactional, measured touches typical of traditional disease management programs. We believe in working with a member, their medical team, and their support circle to solve an addressable challenge, celebrate that victory, pause, and then repeat the process to achieve lasting behavior change.
Is there any positive outcomes data to support the use of systems like CarePoint and Analytix? Do you have any anecdotal of research-based positive outcomes to support these programs?
AxisPoint Health began delivering traditional condition management programs on behalf of payers in 1998, and those programs have achieved over $1 billion in total savings, driving [return on investments] (ROIs) for our clients of greater than 2:1 with an average 12.3% net cost savings.
With the innovations we’ve made with CarePoint and Analytix, we are able to go even deeper to look at a client’s data and provide prospective savings estimations, including the causal chain of what activities and interventions will drive the savings and the ROI we expect to achieve. Once a program is up and running, we can then use our Analytix solution and our team of experienced analysts to show our clients if and how we hit those estimations. We can shine a light on the “black box” of how positive ROIs in condition management programs are produced.
No other solution available today can offer this prospective savings estimation or is as transparent in showing the causal chain leading to results.
Care coordination is another aspect of health care that is getting wide adoption across the industry. Is this something payers need to be focused on?
Yes, because of the complexity of navigating the health care system, payers need to ensure care coordination is happening to avoid unintended duplication of interventions and services. Strong coordination of care is necessary to achieving the Triple Aim.
Is there anything else you would like to add about AxisPoint Health’s tools for large payers?
AxisPoint Health brings 30 years of experience in the care management industry to inform our innovations and solutions. We understand that with the aging of the population and the ongoing increases in chronic disease rates we’re seeing, in order to achieve the Triple Aim, as an industry we can’t simply think of disease or condition management as a “check the box” requirement that doesn’t really deliver results.
We must find new and more effective ways of addressing self-management of chronic conditions and engagement of individuals in their health care outcomes. That’s what we seek to do at AxisPoint Health.
Because CarePoint has been redesigned from the ground up, our solution is able to target and engage the most impactable members across a payer’s population regardless of their condition(s), address the barriers that increase risk and obstruct ability to change, and deliver focused interventions through multiple communication channels to make the biggest impact.
Higher levels of engagement will drive behavior change and care plan adherence for a broader range of a payer’s population, thus improving overall member health outcomes and in turn realizing reduced medical costs and increased member satisfaction. The benefit to payers is in the ability to achieve the Triple Aim.




















