ADVERTISEMENT
Payers, Providers Need to Deliver Consumer-Friendly Value-Based Care
Align with providers, understand the patient journey, and provide clear and understandable data, say these experts who operate in managed care’s trenches
Does the following scenario—which describes an actual patient’s journey—seem to be based on evidence-based care?
A middle-aged man who plays recreational tennis could no longer strike a backhand due to shoulder pain. He saw his primary care physician (PCP), who diagnosed a rotator cuff issue, and prescribed rest, an NSAID, and ice. Things didn’t improve, so he was referred to an orthopedic surgeon, who found nothing on physical exam and ordered an MRI. But the patient soon learned that had to get a plain film first, a requirement of his plan, which delayed the MRI.
When he finally showed up for his MRI, the staff discovered that he could not fit into the machine, so they had to reschedule him for an open MRI. He finally had the MRI 3 months after his initial exam, and returned to his surgeon, who asked him for the film. But the patient said he was not told to bring it. Using a poor bedside manner, the surgeon gave him a cortisone injection and sent him on his way.
He returns to his PCP to get another referral. That surgeon finally looks at the film and prescribes surgery, but the surgeon is leaving the country for 4 months on a medical mission. So the patient has to wait.
Believe it or not, this patient’s journey is based on evidence-based principles, says Richard Popiel, MD, MBA, executive vice president, healthcare services and CMO, Cambia Health Solutions and Regence Health Insurance Company. The standard of care is conservative therapy first, an x-ray before an MRI, referral to a specialist if there is no improvement, a more significant intervention, and finally, surgery as a last recourse.
But a value-based care model that does not include the consumer’s perspective is bound to fall short of expectations, he adds. “This patient received all the right care, but it didn’t happen in the best way. Unless you marry the patient’s journey with evidence-based principles, you will end up with unhappy consumers.”
That was one of the tips Dr Popiel and three of his colleagues offered recently as they analyzed alternative payment models and how to get the most out of them. Each of their organizations is in the midst of transitioning to value-based care. Their advice was delivered during America’s Health Insurance Plan’s recent National Health Policy conference in Washington, DC.
Many in managed care limit their view of the patient to the time they are in the provider’s office. “But that is such a miniscule part of the time they spend” navigating the health care system, says Dr Popiel. Once his organization understood that, things changed.
“We have a different vision,” he explains. “We aim to personalize the health care journey, and we know we can’t do it alone. We partner with providers in a way that helps the consumer experience. Together we invest our knowledge and insights about what consumers need.”
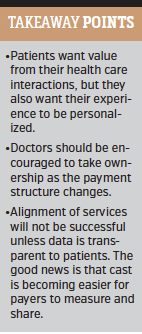
Cambia has found that patients don’t require that much. However, “they want things simple and predictable,” says Dr Popiel. “They want value, but they also want their experience to be personalized.” He notes that payers can learn a lot from the experience customers have on Amazon. And while health care delivery will never become that simple, Cambia has learned to adopt some of Amazon’s approaches, such as asking how consumers want to relate to them.
“We know that we can’t boil the ocean, but we can begin to develop a dramatic understanding of what different segments of the population want, so we can react and provide what the consumer expects,” he says.
For example, the notion of what a doctor is appears to be changing. For some, “a doctor is no longer someone you see face-to-face. Millennials may never want to see their doctor in person if they can help it. Older individuals may prefer to get their care at a senior center and not the office.” The key, he notes, is to understand the various insights and preferences so that value-based care is delivered in the way the consumer demands it.
But don’t expect providers to automatically understand the patient journey. “They are busy seeing patients in 15-minute blocks, so they are not going to take a lot of time to think about it,” says Dr Popiel. The onus is on payers to educate the provider. “Create storyboards, and foster a partnership environment to help providers understand the journey.”
Charles Fazio, MD, MS, medical director, HealthPartners, agrees with Dr Popiel that building trusting relationships with providers is a key to making alternative payment models work. For his organization, it didn’t happen overnight. “We have a long history of collaborating [with clinicians],” he notes. “We are very transparent, which has enabled us to get to a point of trust. That has allowed us to align incentives the right way, and get to a point where there is actual progress.”
 One of HealthPartners’ primary care systems is about to disassociate from the rheumatology group it has used for years as a main source of referrals. Why? “Because one of the many reports we provide them over the years show this group’s costs are much higher than others,” explains Dr Fazio. “They do too many images, and end up making the primary care group look bad.”
One of HealthPartners’ primary care systems is about to disassociate from the rheumatology group it has used for years as a main source of referrals. Why? “Because one of the many reports we provide them over the years show this group’s costs are much higher than others,” explains Dr Fazio. “They do too many images, and end up making the primary care group look bad.”
HealthPartners sees more doctor groups taking ownership as the payment structure changes. The payer keeps providers informed via regular meetings with the finance team, the contract team, and clinical leadership. “We let them know exactly how they’re doing against their cost of care and talk through opportunities. We do this as often as quarterly, and it’s making a difference.”
And like Cambia, HealthPartners is engaging with patients and asking about their journey through the system. “We have had patients help design a clinic,” he says. “They tell us their needs and preferences, and we promise them that they will only have to visit when they need in-person contact with a clinician.”
Meanwhile, Health Care Service Corporation, an independent licensee of Blue Cross and Blue Shield Association, is experiencing the good and the not-so-good as it transitions to alternative pay models. Stephen Ondra, MD, senior vice president and enterprise chief medical officer, explained that his group has about 30% of its contracts in some type of alternative pay model. It is aiming to have three-fourths under such arrangements by 2020. But success, he says, is in the details.
Dr Ondra illustrated by describing two alternative pay models in his system. One is saving about 2% to 3% per year over what would be expected from a traditional PPO. “That’s pretty good, but not perfect,” he said. Meanwhile, another plan is saving 20% to 25% over what would be generated by a traditional PPO.
The difference? “One is a real shared-risk HMO,” says Dr Ondra. As a result, whereas half the care in the first plan take place outside the network, in the HMO only 5% occurs out of network. “That’s because consumers have a stake in the game. Benefit design makes a huge difference.” He calls consumers “the third leg of the tripod,” adding that aligning payers, providers, and patients is key.
However, Dr Ondra was quick to add that all the alignment in the world is not going to help if data is not transparent to patients. “Even if you want to be a good health care consumer today, it’s difficult because you don’t have access to [clear and understandable] quality and cost information,” he says. The good news, he adds, is that cost is becoming easier for payers to measure and share. Quality measures are a bigger challenge. “If we don’t get [a grasp on] quality measures soon it will become a race to the bottom on cost.”
Steven A. Spaulding, senior vice president, Enterprise Networks, Arkansas Blue Cross and Blue Shield, concurred with his colleagues that alignment is key. But it’s more than a simple partnership between payer and clinician.
“The sum of the 2 parts has to be greater,” he explained. “Wouldn’t it be refreshing to see a clinician help solve a payment issue—to actually own it and resolve it? And would it be equally refreshing for me—if I hear about a patient’s clinical problem—to solve it for them? That is the tipping point where patients believe the value proposition.”
Beyond that, it’s not rocket science, says Mr Spaulding. Focus on efforts that make it less profitable for things that are marginal to occur. Reduce reimbursement, create a value pool, and gain a stream of revenue that is not directly tied the consumption of resources.
“That,” he says “is the definition of innovation.” ■





















