ADVERTISEMENT
Game Changer: How CVS & Aetna Could Transform Health Care
Amazon is known for disrupting entire industries. It upended the book business before it went on to forever alter the retail landscape at large, so as speculation spreads that the company is eyeing up an entrance into the health care market it is making for some interesting ripple effects.
After the company acquired Whole Foods, some experts pointed out this type of brick-and-mortar retail base could lead to a pharmacy or a pharmacy benefit manager (PBM). A whole new wave of speculation surfaced after the St. Louis Post-Dispatch reported that Amazon received approval for wholesale pharmacy licenses in at least 12 states. Although a closer look revealed that these licenses allow the company to sell medical equipment and not prescription medications. Some say the mere possibility of the company’s entrance into the pharmacy business has been encouraging a new wave of mergers and acquisitions as health care entities position themselves this for future.
As if on cue, these rumors were abruptly interrupted by the announcement that CVS Health would purchase Aetna, creating a massive health care services umbrella that encompasses everything from health insurance to retail pharmacy sales—a deal that seems at least somewhat inspired by the harbinger of Amazon into the health care space.
Integrating services to lower costs
Whether we are seeing a reaction to Amazon or deals that would have occurred regardless, the frenetic pace of combination signals that market participants are realizing “that this business is going to get leaner and that some people are going to get their lunch eaten,” Kathy Hempstead, PhD, senior advisor with the Robert Wood Johnson Foundation, told First Report Managed Care.
The Optum unit of UnitedHealth Group recently announced that it was purchasing home-care provider DaVita Medical Group for $4.9 billion, according to a Forbes report, and Humana’s potential acquisition of Kindred Healthcare could further the insurer’s strategy to keep Medicare patients out of hospitals and in lower-cost settings.
These are just a couple of recent examples that are part of a larger wave of strategic partnerships bringing insurance companies and health care providers together to offer integrated services, lower the cost of medical care, and minimize the chance that it is their “lunch” being taken away by others as the landscape continues to change and evolve.
But the early December announcement that CVS plans to acquire Aetna for $69 billion offers up a unique combination considering the delivery is focused on pharmacies. The hope is that the combined company will remake the consumer health care experience by offering more services within CVS drugstores and creating a platform “that is easier to use and less expensive for consumers,” CVS Health President and CEO Larry J Merlo said in a statement.
Eliminating Middlemen
While massive mergers between health insurance companies Aetna and Humana as well as Anthem and Cigna were blocked by antitrust regulators in early 2017 and a deal between drug store chains Walgreens and Rite Aid was more recently called off because of similar concerns, the CVS/Aetna deal is less likely to be blocked, according to experts, because it pairs entities from two different sectors.
“The bottom line,” Ken Kaitin, PhD, professor of medicine and director of the Tufts Center for the Study of Drug Development, told First Report Managed Care, “is that in the United States we have perhaps the most complex distribution system for pharmaceuticals in the world.”
There are a whole group of stakeholders that stand between the developer of a drug and the prescribing of a drug product, and the value of the product is spread across that entire distribution network. More and more, we will likely see companies trying to get into this area of mergers in order to simplify the process, increase their leverage, and obtain better prices.
Amazon has the potential to become the distributor of the products but also the wholesaler as well, he explained, with its enormous purchasing power and tremendous reach. This would allow the company to negotiate competitive rates from the developers, which would make it more difficult for the smaller distributors and PBMs.
And the combination of CVS and Aetna would constitute a formidable negotiator as well.
“What this does is it cuts out one of the parties,” he said, “because now the health plan is dealing directly with the distributor of the drug.” And anybody who can cut out one of those parties and increase their leverage in this market has a competitive advantage.
Article continues on page 2
There is a half full and half empty way of looking at this merger. “As wary as we all should be about the prospect of consolidation in health care and potentially the threat to competition,” Dr Hempstead said, “I also think there is truly a lot of fresh thinking going on.”
This combination of Aetna and CVS carries with it the potential for “rethinking a lot of how health care is delivered” and facilitating “some different approaches to care utilization and ways of trying to keep people in less expensive settings.”
A huge pain point for consumers is the way that the fragmentation in the current system affects them and just the overall lack of convenience that comes from one link in the chain not knowing or seeming to care to know anything about the next link in the chain, she explained, which oftentimes turns into a hassle for consumers.
Bigger is not always worse for consumers, Dr Hempstead added, noting that she remains “cautiously optimistic to see what might come out of some of these new combinations and new ways of working together.” That being said, “combining the cultures of Aetna and CVS isn’t going to be trivial, and they may find that it’s a lot harder than they thought.”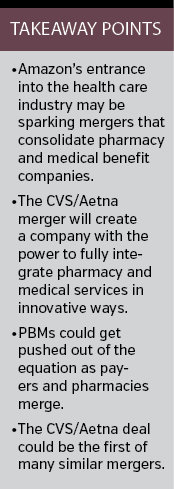
Start of a Trend?
“I think what you see a lot of in this sector is a wait and see,” Dr Kaitin said, “so I suspect what’s going to happen is a number of the other major players—the health insurers and PBMs and others—are going to see how this works out.”
There are cases over the years where new relationships do not live up to their hope. Right around the time that PBMs started to come into their own, for example, some pharma companies decided to own them in order to avoid the need to negotiate with them. That only lasted for about 5 years, he said, when they all realized this is not in their sweet spot.
More importantly, it raised conflict of interest concerns because a PBM has to offer a whole range of drugs for patients who need them and not just the drugs made by one manufacturer. “So it led to all sorts of questions,” he said, “and ultimately every single one of the large pharma companies that owned PBMs got rid of them.”
This seems like the type of scenario where many will be observing and determining whether the partnership seems to make good sense over time. “If it looks like it’s successful,” he added, “I do think we’ll see a lot more of these types of mergers.”
As some have pointed out, the CVS/Aetna deal, and others like it, could wind up changing the way many major US corporations buy health coverage for their employees, and it raises new questions over the cost of those benefits, according to a Reuters report. Most companies employing over 20,000 people keep their prescription drug benefits separate from medical coverage, believing they are paying less by shopping those contracts around.
CVS and Aetna argue that their deal will provide added leverage in price negotiations with drug makers, an ability to better manage the use of those medications, and the opportunity to lower health care costs for employees of its large corporate customers. But employers are expected to scrutinize these types of assertions.
Those buying coverage for their workers could experience difficulty figuring out how much they are paying for a certain medicine or service, one consultant told The New York Times. Drug prices and a lack of transparency tend to go hand in hand as is, and employers could have even less information available in this situation.
A Future with Amazon
So will Amazon actually enter this sector? While some say that a journey into the regulated realm of pharmacy distribution would be a slower and more difficult one than its spread into other sectors, it is not as if the company would need to chart new territory, Dr Kaitin pointed out.
Although there would be a licensing element to contend with, it is silly to think that Amazon could not figure out how to make it work.
“I suspect this is a logical step for them to get into the pharmacy business,” he said.
Similarly, Dr Hempstead would not be surprised to see Amazon move forward. Although it is a complex business environment, the company has some significant advantages in terms of
distribution and the potential to eliminate pain points.
“I think the expectation is that they will but I don’t think it’s clear when or how,” she said.
If Amazon does push ahead, it will be interesting to see if it can make any headway in terms of negotiating with drug manufacturers. If not, Dr Hempstead said, “then I’m not sure how big their advantage will be.”























