Fighting Opioid Misuse With Advanced Management
 An interview with Snezana Mahon, PharmD, vice president, clinical product development at Express Scripts.
An interview with Snezana Mahon, PharmD, vice president, clinical product development at Express Scripts.
What role can companies like Express Scripts play in the fight against the nationwide opioid epidemic?
As an independent pharmacy benefit manager, Express Scripts is uniquely positioned to work across the care continuum to engage prescribers, mobilize payers, and protect patients and comprehensively address the opioid issue.
Through our data analytics, specialized pharmacy practice, fraud, waste and abuse management capabilities, and application of behavioral science, we have the ability to help stop abuse before it starts. Our work starts before a patient receives a first prescription for an opioid medication.
Can you give an overview of the Advanced Opioid Management solution?
Our solution seeks to minimize early exposure and prevent progression to overuse and abuse at three critical touchpoints:
1. At the Pharmacy
• First-time users of short-acting opioids restricted to an initial fill days’ supply of seven days.
• Enhanced prior authorization for all long-acting opioids to block fills for naïve, or new, users.
• Morphine Equivalent Dose (MED) edit giving visibility to, and requiring prior authorization for, members accumulating quantities of opioid medication exceeding 200Mg morphine equivalent dose/day.
• Our concurrent drug utilization review (CDUR) will also ensure opioid prescriptions are appropriate, medically necessary and unlikely to result in adverse medical consequences.
2. With Physicians
• We send automated messages directly to all opioid-writing physicians at the point-of-care via their Electronic Health/Medical Records (EHR/EMR) portal to inform them of potential duplicate therapy, misuse and abuse, drug-drug interactions, use of multiple prescribers or pharmacies – or when their patient is approaching morphine equivalent dose (MED) thresholds.
3. With the Patient:
• We send an educational letter after first fill to educate members of the serious potential risks of opioid use, safe handling instructions, important restrictions, and proper disposal of unused medication.
• Our Opioid Neuroscience Specialist Pharmacists conduct proactive outreach to patients triggered by one of several scenarios where our data signals concerning patterns of use. For example, filling 2 or more different short-acting opioids within the last 30 days.
• We provide deactivation disposal bags to first-time opioid utilizers who our data indicate are likely to have leftover medications. The bags include clear instructions for handling and disposal in member’s home – no driving or special disposal day required.
• We limit patients to obtaining an opioid prescription from doctor and filling that Rx at one pharmacy (otherwise known as lock-in), when our Fraud Waste and Abuse (FWA) program detects drug seeking behavior.
How was the program developed?
Express Scripts has a history of industry leadership in the fight against opioid abuse, including its Fraud, Waste and Abuse program, and advocacy for pharmacy and physician lock-in and prescription drug monitoring programs (PDMP).
We created our Advanced Opioid Management solution, building on that legacy and on our experience caring for patients using these medications. We also analyzed opioid use among our members and listened to our clients’ feedback and concerns about safe opioid use.
Most importantly, we tested our approach in the Express Scripts Lab. In a recent pilot study of more than 100,000 Express Scripts members new to opioid therapy, we observed a 38 percent reduction in hospitalizations and 40 percent reduction in emergency room (ER) visits in the intervention group versus control group during six months of follow up. Half of patients received an educational letter from the Express Scripts Neuroscience Therapeutic Resource Center (TRC) and half no intervention at all. A subset of patients receiving the TRC educational letter who had high-risk patterns of opioid use also received a counseling call from a Neuroscience TRC specialist pharmacist. Among this subset, we observed a 19 percent decrease in the day’s supply of opioid dispensing during six-months of follow up. Patients got the medicine they need while we helped prevent unnecessary refills that could put patients at risk of significant harm.
 The program seems multifaceted, in that it tackles multiple points of care where misuse could arise, can you discuss this aspect of the program?
The program seems multifaceted, in that it tackles multiple points of care where misuse could arise, can you discuss this aspect of the program?
Driving change in the opioid crisis requires addressing the full care continuum, and influencing behavior at every touchpoint. Drug utilization management alone is not the answer. To impact care and costs, doing the minimum won’t do anything. Simply put, plan sponsors need a treatment plan, not a bandage.
From a managed care perspective, is a program like this cost-effective/cost-beneficial?
The program is an investment with significant benefits: decreased pharmacy cost, decreased medical and treatment costs, and improved member care. With this solution, plan sponsors can stay ahead of additional government regulation to address the rising tide of opioid abuse. For example, for health plans, this will be a demonstration of innovation and commitment to solving a serious national problem your employer clients are facing.
Most importantly, plan sponsors in our program can directly contribute stopping our nation’s deadly opioid crisis. Consider the following:
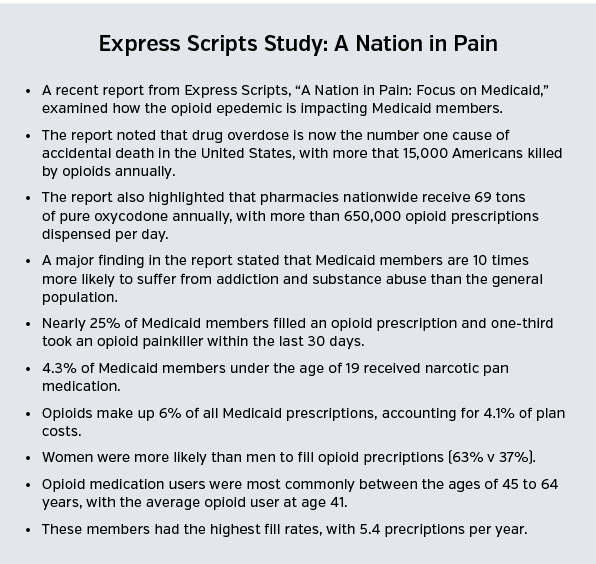
• In 2015, more than 15,000 people fatally overdosed on prescription pain killers, according to the Centers for Disease Control and Prevention (CDC).
• 6 of 10 overdose deaths involve an opioid.
• The average time between that patient’s first opioid prescription and death is 2.6 years.
Does Express Scripts’ position in the marketplace, as both a PBM and pharmacy, give it any unique ability to enact a program like this?
Express Scripts’ opioid solution is designed to lower risk at each touchpoint of the care continuum – including prescribers, pharmacies and patients – in a way that far exceeds what other PBMs offer today.
We believe our one-of-a-kind, specialized pharmacy practice, our independent model and our commitment to research and innovation make us uniquely able to address this issue at multiple touchpoints. By focusing across the entire care continuum – from over-prescribing to over-dispensing, and unsafe overutilization of pain medications – we found we can make a significant and meaningful difference in this national epidemic.
Will the Advanced Opioid Management program be tailored to payers that work with Express Scripts?
Plan sponsors can tailor the program; however, we recommend implementing the program completely to maximize the results.
Are there any barriers to implementing a program like the Advanced Opioid Management solution?
Safe opioid use does require the commitment of each of our touchpoints: physicians, pharmacists and patients.
We know from our research in the pilot, along with our experience in behavioral science, that we can activate people’s good intentions and make a meaningful impact through our program and the various types of outreach we conduct at each touchpoint.




















