COPD: Challenges and Consequences for Stakeholders
 Chronic obstructive pulmonary disease (COPD) is a formidable disease state with no known cure. COPD is an umbrella term encompassing a group of lung pathologies that include emphysema, chronic bronchiolitis, bronchiectasis, and nonreversible asthma. It remains a major cause of morbidity and mortality in the United States, despite advances in lowering smoking rates and preventive measures. While prolonged exposure to tobacco is recognized as the most significant risk factor for COPD, additional risk factors include, age, genetic factors, exposure to occupational toxins, and poor indoor quality in the home. COPD is also associated with a significant clinical and economic burden. Consensus guidelines have been developed for the identification and management of COPD; however, COPD remains an underdiagnosed and undertreated condition.
Chronic obstructive pulmonary disease (COPD) is a formidable disease state with no known cure. COPD is an umbrella term encompassing a group of lung pathologies that include emphysema, chronic bronchiolitis, bronchiectasis, and nonreversible asthma. It remains a major cause of morbidity and mortality in the United States, despite advances in lowering smoking rates and preventive measures. While prolonged exposure to tobacco is recognized as the most significant risk factor for COPD, additional risk factors include, age, genetic factors, exposure to occupational toxins, and poor indoor quality in the home. COPD is also associated with a significant clinical and economic burden. Consensus guidelines have been developed for the identification and management of COPD; however, COPD remains an underdiagnosed and undertreated condition.
Assessment of COPD, according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines is based on the patient’s level of symptoms, degree of airflow limitation using spirometry, future risk of exacerbations, and identification of comorbidities. Several classes of medications are used for the treatment of COPD. GOLD recommends long-acting bronchodilators, including long-acting beta2-agonists, over short-acting bronchodilators for patients with either more COPD symptoms or who are at higher risk for COPD exacerbations. For most patients with COPD, long-acting bronchodilators with or without inhaled corticosteroids are the first or second choice controller therapies.
COPD: By the Numbers
According to the Centers for Disease Control and Prevention (CDC), 15 million Americans reported that they had been diagnosed with COPD in 2011; however, the actual number of adults with COPD is thought to be much higher. The American Lung Association reported that studies suggest it is an underdiagnosed disease state with up to 24 million Americans having evidence of comprised lung function.
COPD has a substantial impact on health care expenditures and utilization because of comorbidities and the high rate of hospitalization and readmissions. A 2015 study from CDC researchers published in Chest showed that the national medical costs attributable to COPD and its consequences were estimated at $32 billion annually and total absenteeism costs were about $4 billion in 2010. Of the medical costs, 18% were paid by private insurance, 51% by Medicare, and 25% by Medicaid. The researchers projected that national medical costs are expected to increase to $49 billion in 2020.
However, the actual cost could be higher than these estimates since a considerable proportion of patients with COPD are undiagnosed. “I think it’s difficult to completely quantify the economic impact of COPD misdiagnosis, but data suggest th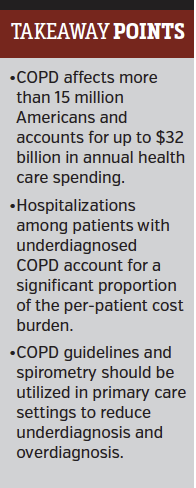 at undiagnosed COPD has a significant impact on health care costs.” Meilan Han, MD, associate professor, University of Michigan, said in article published in Medical Economics. “We know that appropriate therapy can help reduce the frequency of exacerbations and that exacerbations account for 50% to 75% of direct COPD health care costs.”
at undiagnosed COPD has a significant impact on health care costs.” Meilan Han, MD, associate professor, University of Michigan, said in article published in Medical Economics. “We know that appropriate therapy can help reduce the frequency of exacerbations and that exacerbations account for 50% to 75% of direct COPD health care costs.”
One study of 6864 COPD patients enrolled in a managed care plan, from Dr Mapel and colleagues in Value Health, found that total costs were higher by an average of $1182 per patient in the 2 years before the initial COPD diagnosis, and $2489 in the 12 months just before the initial diagnosis as compared with matched controls. Most of the higher cost for undiagnosed COPD was attributable to hospitalization.
Challenges for Stakeholders
A comprehensive view of COPD care in the United States from key stakeholders looked at the needs, challenges, and potential health solutions of this disease state (Lancet Resp Med. 2016;4[6]:473-526). One of the challenges is there is no best approach for identification of patients with COPD who are undiagnosed. Diagnosis in primary care is also often done without the use of spirometry, leading to both overdiagnosis and underdiagnosis. The report also found that COPD therapy in primary care is often inconsistent with guidelines or evidence, resulting in suboptimal or no treatment for many patients.
From an economic perspective, rising costs are prompting payers to collaborate with health care providers and health systems to improve care coordination. The challenge, however, is that COPD-specific quality initiatives and management programs remain mostly isolated initiatives driven by individual health systems. Provisions in the Centers for Medicare and Medicaid Services (CMS) Hospital Readmission Reduction Program (HRRP) are placing increased pressure on hospitals to integrate with health care providers. In 2014, CMS included COPD in HRRP, which penalized hospitals for excessive 30-day, all-cause readmission after a hospitalization for an acute exacerbation of COPD.
“While the HRRP is not a perfect national policy, it does bring important stakeholders together to focus on value-based care for patients with COPD,” according to Dr Shah and colleagues in a study published in Chest.
The challenges faced by the medical community in identifying and managing patients with COPD was the focus of advisory panel of respiratory specialists and payer stakeholders and reported March 2016 in American Health & Drug Benefits supplement. There panel agreed on the importance of specialty care in COPD; maintaining open access to pharmacologic therapy; and increased focus on reducing acute exacerbations, hospital admissions, and hospital readmissions associated with COPD.




















