The Challenges of Managing Complex Populations Through Public Programs
 It is no secret that managing complex populations through public programs can be a daunting task. Four managed care leaders recently shared their expertise and experiences during America’s Health Insurance Plans’ National Health Policy Conference in Washington, DC. All of them agreed that medical care is just the tip of the iceberg. Often, they must first find patients who are usually transient, gain their trust by addressing their most basic and non-health-related needs, and then spend more money on them in the short-term. But the long-term rewards are evident. Overall costs are reduced dramatically, and dignity is returned to an often neglected and forgotten patient population.
It is no secret that managing complex populations through public programs can be a daunting task. Four managed care leaders recently shared their expertise and experiences during America’s Health Insurance Plans’ National Health Policy Conference in Washington, DC. All of them agreed that medical care is just the tip of the iceberg. Often, they must first find patients who are usually transient, gain their trust by addressing their most basic and non-health-related needs, and then spend more money on them in the short-term. But the long-term rewards are evident. Overall costs are reduced dramatically, and dignity is returned to an often neglected and forgotten patient population.
________________________________________________________________________________________________________________________________________________________________________
RELATED CONTENT
CMS Proposes New Rule To Strengthen 2018 ACA Marketplace
CMS: ACOs Generate Over $1 Billion in Medicare Savings Since 2012
________________________________________________________________________________________
The Why of Medicaid
Paul A Tufano, JD, chairman and CEO of AmeriHealth Caritas in Philadelphia, said it’s important to answer the simple question, “Why?”
“Unfortunately, the ‘why’ of Medicaid is usually overshadowed by the ‘how’ and the ‘what,’” he explained. “How does Medicaid work? How should we pay for it? How much longer should we pay for it? What can we do to reduce it?” Mr Tufano follows the principles in Simon Sinek’s book, Start With Why. Success comes when “the ‘why’ of an organization drives the ‘how’ and the ‘what.’”
Mr Tufano believes that “access to health care for the poor and chronically ill is important because it is perhaps the most decent, noble, and important work we can do as human beings.” During his travels, he sees first-hand the disparities among the poor, including higher incidence of illness, mortality, and lack of access to health care.
“Even access to fruits and vegetables—something most of us take for granted—is virtually non-existent in many parts of the country,” he said.
Furthermore, Mr Tufano is alarmed by misconceptions about Medicaid patients. “I do agree that we need to have a respectful debate about the cost of Medicaid benefits, but in some circles that debate is rooted in a harsh and uninformed view of the poor,” he said. “I’ve encountered people who think that Medicaid incentivizes people to stay home and not work. When I have those encounters, I pull out my Blue Cross card and remind people that all we’re talking about is giving people access to the same type of health care that you and I enjoy.”
He also argued that investing in giving the poor better access to care in the short-term will save taxpayers money over time. “Patients will have a greater chance of overcoming the barriers to living healthy and productive lives.”
Mr Tufano said that those who want to successfully serve these complex populations must realize that poor people do not want to be poor; they want to work, they have dreams and aspirations, and they want to be treated with dignity. He emphasized the last point by noting what he often tells people: “I am not in the Medicaid managed care business; rather, I am in the dignity business.”
Providing dignity, he believes, is a privilege that should never be taken for granted, no matter how big the challenges. To live up to the expectation, Mr Tufano believes that it is necessary to:
• have honest dialogue about health care for the poor and the chronically ill;
• leverage health care innovation and focus its power more keenly on the poor;
• make sure the underprivileged have access to information about their health, as well as the ability to learn from it;
• never presume to know what’s best for the poor unless you listen to them; and
• invest more to attract the most qualified people to serve the poor.
“I believe that what we do every day is as cool and exciting as Google and Apple, and as impactful and rewarding as the Peace Corps,” Mr Tufano concluded.
Not Your Typical Patients
Pat Wang, CEO of HealthFirst, a nonprofit health insurance company which serves poor populations in New York City and the surrounding area, understands that the people that her organization manages are not typical patients. “They don’t necessarily know how to schedule and keep an appointment, may not have any means of transportation, no discretionary income to speak of, and may not even have a roof over their head.”
For those reasons, the goal must first be to tend to the patient’s primary problem, even if it is as simple as a lost pair of eyeglasses. “Our nurses will solve that problem first. They have to. We may want them to pay attention to their hypertension, but they’re not going to unless other things in their life are stable,” she said.
Ms Wang also stressed the importance of engaging with the provider community. “We partner with hospitals, health centers, and individual physicians, making sure providers are from the same community or of the same ethnicity as our members,” she said. “We believe this is very important to ensure culturally competent care.” This philosophy of diversity extends to HealthFirst’s staff; for example, its call center is able to communicate in five languages.
Ms Wang concluded by acknowledging the challenges that remain. Most notably, the monumental effort of effectively meeting the needs of specific “carve-ins,” such as those who need behavioral health services or nursing home care.
“There is a steady progression of these carve-ins,” she said. “It is great that we have been able to absorb these complex populations, but it hasn’t been easy. As one of my state regulators said to me jokingly, ‘Why do you think we left it until last?’”
More Than Just Medical Care
J Mario Molina, MD, president and CEO of Molina Healthcare, which serves Medicaid and Medicare patients in 15 states, agrees with Ms Wang that it takes a team that is integrated into the community to make an impact. This management strategy includes home care and social workers, which he said are sometimes more important than the clinicians. Moreover, he stressed the importance of mobilizing integrated teams, as opposed to just one person or a case manager. “Managing complex populations is really only a little bit about medical care and involves many other ancillary provider and social services.”
The organization’s main objective is to return people to the community. It starts, Dr Molina said, in nursing homes. “We provide comprehensive health assessments, determine our members’ needs, and integrate their care.” He said that Molina Healthcare sees nursing home patients more frequently than the typical monthly visit. “We have found that by increasing the frequency of visits we can catch things before a patient has to be admitted to the hospital.” 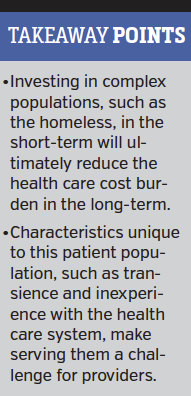
Transitioning people from the nursing home back into the community is crucial, when it is possible, Dr Molina explained. He recalled a patient who had both Medicaid and Medicare benefits, with long-term care costs around $7000 per month. “In order to get her back home we had to put her into a physical rehab program, which Medicare paid for.” Still, the additional cost in the short-term led to long-term savings. Once she was transitioned home, costs decreased to less than $1000 a month.
“This illustrates the benefit of combining Medicare and Medicaid funding into one contract,” he noted, adding that too often, when these agencies are managed separately, “they try to toss you back and forth to each other. For complex patients it is better to have everyone aligned, and our contracts are doing that.”
Dr Molina acknowledged that the percentage of patients who can transition is small. In Florida, his organization has moved about 5% of nursing home patients back into the community. “It may not sound like a lot, but it’s a huge savings for the state even if it’s only a small percentage.”
Find Them, Then Serve Them
Kenneth Burdick, JD, CEO of WellCare Health Plans Inc in Tampa, FL, oversees an organization that manages 3.8 million lives under Medicaid and Medicare. He echoed his colleagues’ observations: “It’s all about wrapping around the members. And I agree that physical health is just a small part of what we agree to take on.”
Mr Burdick explained that his group’s “secret sauce” is local market community advocacy. “It’s a crucial part of trying to help members with chronic care issues.” For him, it starts with finding members, who oftentimes do not have an address. “How do you serve them if you can’t find them?” In order to locate patients, his group partners with organizations that help find people in need of health care services. “We find them under bridges, in public parks, shelters, and elsewhere.”
Once located, they aim to conduct a health assessment. But Mr Burdick echoed his colleagues, noting that before addressing health, they must often resolve other issues first. WellCare not only engages with social service agencies but has a single toll-free number that can connect members with just about any social service in any area where it operates. “These are not Medicaid-covered benefits, but we recognize that you first must address life concerns before physical health issues.”
The strategy eventually pays off, said Mr Burdick. He has seen emergency department visits, hospitalizations, and behavioral health visits decrease dramatically. Meanwhile, physician office visits and behavioral health prescriptions are rising. “That’s a great trade-off,” he said.
This kind of approach reduces costs by as much as 78% just by “helping patients navigate the system,” Mr Burdick said.
Mr. Burdick recalled a patient in New York who had 15 hospitalizations before WellCare could find him. Since the time he was found, “he has had zero hospital admissions. He still struggles with sleep apnea, diabetes, and sciatica, but he is managing his health care for the first time in 49 years.”




















