Outcomes of Brachial Plexus Neurolysis in 40 Patients With Obstetric Brachial Plexus Injury
© 2024 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of ePlasty or HMP Global, their employees, and affiliates.
Abstract
Background. Severe traction injury to the brachial plexus (BP) during childbirth can induce the formation of intraneural scar tissue or neuroma in continuity. This can lead to nerve entrapment and demyelination, which inhibit axonal transport to the target muscles. Secondary complications include muscle weakness, contractures, joint deformity, and altered limb growth with prolonged and persistent disability. These patients find difficulty performing activities of daily living. BP neurolysis is one of the multistage reconstructive procedures in patients with obstetric brachial plexus injury (OBPI). The successful outcome of BP neurolysis is reported in patients with OBPI. We report improvements in all Mallet functional movements, including forearm supination angle (the Nath-modified Mallet), in 40 OBPI patients after BP neurolysis.
Methods. Forty OBPI patients (25 female and 15 male with a mean age of 14 years, range 2-25 years; 29 on the right and 11 on the left) underwent BP neurolysis and follow-up evaluations with the lead author and surgeon (RKN). All these patients had undergone multiple previous surgeries, such as primary exploration, Botox, nerve transfer, humeral or forearm osteotomy, wrist tendon transfer, mod Quad, triangle tilt, and biceps tendon lengthening. Patients’ pre- and postoperative shoulder functions were evaluated by the surgeon in the clinic and from photos/videos. These functional movements include shoulder abduction, external rotation, hand-to-mouth movement, hand-to-neck movement, and hand-to-spine movement, which score from 1 (no movement) to 5 (normal movement). In addition to the Mallet functional movements, the supination angle (the angle between the midline of the body and the tangential line to the palm with arms straight; neutral = 0, full supination = 90°, full pronation = −90°) was also evaluated and scored using the Nath-modified Mallet before and after BP neurolysis.
Results. Of the 40 patients in this report, 37 (93%) achieved a Mallet grade of 5/5 (n = 23, 58%) or 4/5 (n = 14, 35%) in shoulder abduction after BP neurolysis. The other 3 patients had a Mallet grade of 3/5 (90 degrees) postoperatively in shoulder abduction. There was statistically highly significant improvement after BP neurolysis in shoulder abduction (3.9 ± 0.7 to 4.5 ± 0.6, P < .0001), external rotation (2.9 ± 1.0 to 3.8 ± 1.1, P < .0001), hand-to-mouth (4.2 ± 0.7 to 4.5 ± 0.7, P < .03), hand-to-neck (3.6 ± 0.8 to 4.2 ± 0.8, P < .0001), hand-to-spine (2.9 ± 1.1 to 3.4 ± 1.2, P < .004), forearm supination (3.8 ±1.1 to 4.2 ±1.0, P < .0001), the Nath-modified total Mallet score (21 ± 3.1 to 25 ± 3.3, P < .0001), including supination angle (40.5 ± 48.8 to 56.3 ± 41.6, P < .001). Improvement in the Nath-modified total Mallet functions was weakly associated with follow-up time after BP neurolysis (R = 0.17, P = .0003).
Conclusions. Among the 40 patients, 37 (93%) achieved a Mallet grade of 5/5 or 4/5 in shoulder abduction after surgery with a mean follow-up of 2 years. All upper-limb functional movements improved significantly as BP neurolysis improves axonal transport to the target muscles after surgically removing the external and internal scarring of the upper trunk and its terminal branches. Additionally, neurolysis decompresses the BP from external compression by the surrounding connective tissues and densely scarred scalene muscles. Thus, it can provide these patients with an effective and rapid functional recovery. These children and their parents are pleased with the progress and increased ability to perform their activities of daily living after surgery.
Introduction
Obstetric brachial plexus injury (OBPI) is rare (0.5-2.6 in 1000)1 yet the most frequent type of birth injury that results from traumatic stretching of the brachial plexus during childbirth. Spontaneous recovery is common, with only 10% to 30% of patients having prolonged and persistent disability,2 leading to secondary complications including persistent muscle weakness, contractures, joint deformity, and altered limb growth,3 and these patients find difficulties with the activity of daily living (ADL).4
Severe traction injury to the brachial plexus (BP) in these patients induces the formation of intraneural scar tissue or neuroma in continuity5-7 that can cause nerve entrapment and axon demyelination and inhibit axonal transport.8 The regenerating nerve fibers from the proximal injury site to send motor signal conduction to the distal target muscles can be compromised by (1) intraneural scar or neuroma formation by the excessive proliferation of fibroblasts, which produce axon growth inhibitory proteins and scar-associated proteins such as semaphorins 3A (sema3A) and 3F (sema3F), as shown in neuroma tissue in permanent OBPI; 9 (2) poor axonal movement and abnormal branching patterns; and (3) axonal crosstalk of regenerating nerve fibers.
Scar formation at the site of nerve lesion is deleterious to functional recovery. Treatment of OBPI is multifaceted, focused on repairing nerve injury and preventing and treating secondary musculoskeletal deformities. Neurolysis is indicated to remove scar tissue, treat hampered axonal growth, and transport to the target muscles. Studies have shown a significant improvement in upper-limb functional movements after microsurgical neurolysis in OBPI.5,6,10-27 Wells et al28 recently reported that the proportion of OBPI patients treated with neurolysis alone had no significant change in 3 decades.
Here, we report the outcomes of BP neurolysis in 40 OBPI patients with an average age of 14 years old (2-25) who had undergone multiple previous surgeries, including nerve, muscle, and bony surgical procedures.
Methods and Materials
Forty OBPI patients (25 female and 15 male with a mean age of 14 years, range 2-25; 29 on the right and 11 on the left) underwent BP neurolysis and follow-up evaluations with the lead author and surgeon (RKN). All these patients had undergone multiple previous surgeries, such as primary exploration, Botox, nerve transfer, humeral or forearm osteotomy, wrist tendon transfer, mod Quad, triangle tilt, and biceps tendon lengthening (Table 1). Patients' pre- and postoperative shoulder functions were evaluated by the surgeon in the clinic and from photo/video records. We adopted the Mallet grading system to evaluate the patients’ all upper-limb functional movements. These functional movements include shoulder abduction, external rotation, hand-to-mouth movement, hand-to-neck movement, and hand-to-spine movement, which score from 1 (no movement) to 5 (normal movement). In addition to the Mallet functional movements,29 the supination angle (the angle between the midline of the body and the tangential line to the palm with arms straight; neutral = 0, full supination = 90°, full pronation = −90°) was also evaluated and scored using the Nath-modified Mallet30-33 (shown in Figure 1): full pronation −90°, grade 1; supination angle (<-30°), grade 2; supination angle (-30 to 30°), grade 3; supination angle (>30 to 80°), grade 4; and supination angle (>80°), grade 5.
Table 1


Abd, abduction; BP, brachial plexus; BTL, biceps tendon lengthening; ER, external rotation; F, female; FO, forearm osteotomy; HM, hand-to-mouth; HN, hand-to-neck; HS, hand-to-spine; HO, humeral osteotomy L, left; M, male; MQ, mod Quad; NT, nerve transfer; R, right; SNG, sural nerve grafting; Sup, supination; TT, triangle tilt

Figure 1. The Nath-modified Mallet evaluation of function and arm appearance. Supination and the resting position are assessed in addition to the traditional modified Mallet grading. The total Nath-modified Mallet score is calculated from the scores for shoulder abduction, external rotation, hand to mouth, hand to the neck, hand to spine, and supination, giving a maximum score of 30. Angles for abduction and forearm supination are measured from video stills. The Nath-modified scoring method is reported in detail33 as the modified Mallet system in the literature.
Other investigators reported the Nath-modified scoring method in detail33 as one of the modified Mallet grading systems in the literature. Twenty-nine patients had upper and middle plexus injuries, 4 had C5-C8, and 7 had total plexus (C5-T1) injuries.
Surgical technique
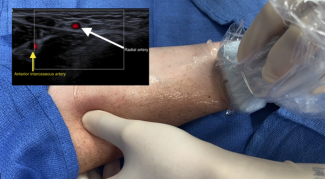
The patient was brought to the operating room, where they underwent general anesthesia. The injured side of the neck and arm was prepped and draped in the usual sterile fashion. An initial incision was created over the area where the upper trunk of the brachial exited through the anterior scalene muscle, about 2 cm superior to the upper clavicular border. A dense scar in the neck required extra care to dissect to reach the affected nerves in this region. The upper trunk of the brachial plexus was identified deep within the scalene fat pad. The fat pad was retracted, and the underlying upper trunk of the brachial plexus was identified. It appeared to have quite a thick epineurial scar consistent with the injury to the upper trunk and its terminal branches, including the anterior and posterior divisions and suprascapular nerve. The posterior divisions of the upper trunk and suprascapular nerve appeared most affected. The thickened epineurium of the anterior division was externally neurolyzed through microsurgical technique and high magnification. Subsequently, the posterior division similarly underwent external neurolysis. The suprascapular nerve was externally neurolyzed through a microsurgical technique.
The anterior scalene muscle was densely scarred, impinging the upper trunk. Consequently, the muscle was surgically freed to alleviate the compression on the upper trunk. The substance of the upper trunk was entered, and the perineurium was dissected through microsurgical technique and high magnification. Major fascicle groups of the posterior division were separated, and an internal scar was removed by internal neurolysis. Subsequently, the suprascapular nerve was treated similarly by separating the fascicles and performing internal neurolysis. Internal neurolysis was also performed on the anterior division. Direct electrical stimulation improved the conduction to the biceps and shoulder muscles following surgery, based on intraoperative monitoring.
Subsequently, another incision was created in the medial upper arm, where the neurovascular bundle of the arm was located. A sharp and blunt dissection revealed the median, ulnar, and radial nerves. All were noted to be scarred and compressed, with poor electrical conductivity. The median, ulnar, and radial nerves underwent external neurolysis, followed by internal neurolysis.
In summary, direct electrical stimulation improved the conduction to the muscles innervated by all operated muscles after surgery, based on intraoperative monitoring measured in the operating room by a third-party electrophysiology team. Blood loss was minimal, and there were no complications.
Statistical analyses
Excel 2013 (Microsoft Corp) was used to analyze descriptive statistical data and generate graphs. Paired Student t tests were conducted to determine if differences between preoperative and postoperative modified Mallet scores for each function were statistically significant. The P values were two-tailed and considered significant if they were less than or equal to .05. We used the Pearson correlation coefficient to assess the associations between the follow-up time and the surgical outcomes.
Results
Among the 40 patients in this report, 37 (93%) achieved a Mallet grade of 5/5 (n = 23, 58%) or 4/5 (n = 14, 35%) in shoulder abduction after BP neurolysis. The other 3 patients had a Mallet grade of 3/5 (90 degrees) postoperatively in shoulder abduction. The mean shoulder abduction angle was 148 ± 30 after BP neurolysis, improved from 125 ± 29 degrees. There was statistically highly significant improvement after BP neurolysis in shoulder abduction (3.9 ± 0.7 to 4.5 ± 0.6, P < .0001), external rotation (2.9 ± 1.0 to 3.8 ± 1.1, P < .0001), hand-to-mouth (4.2 ± 0.7 to 4.5 ± 0.7, P < .03), hand-to-neck (3.6 ± 0.8 to 4.2 ± 0.8, P < .0001), hand-to-spine (2.9 ± 1.1 to 3.4 ± 1.2, P < .004), forearm supination (3.8 ±1.1 to 4.2 ±1.0, P < .0001), the Nath-modified total Mallet score30-33(21 ± 3.1 to 25 ± 3.3, P < .0001), including supination angle (40.5 ± 48.8 to 56.3 ± 41.6, p<0.001) 30-32 (Tables 1 and 2; Figures 1-7). The Mallet score for hand-to-spine remained unchanged in 13 patients. Thirty-one of 40 patients (78%) achieved a Mallet score of 4 or 5/5 in ER postoperatively. Fourteen patients with a Mallet score of 2/5 for ER preoperatively improved to 4 or 5/5 after neurolysis.
Table 2


Figure 2. Nath-modified total Mallet functions, including forearm supination, before and after BP neurolysis in 40 patients with OBPI.

Figure 3. The Nath-modified total Mallet functions, including forearm supination, before and after BP neurolysis in 40 patients with OBPI.

Figure 4. A mean of forearm supination and the other classical Mallet functional movements before and after BP neurolysis in 40 patients with OBPI.

Figure 5. Shoulder abduction angle before and after BP neurolysis in 40 patients with OBPI.

Figure 6. External rotation and hand-to-neck movement before and after BP neurolysis in 40 patients with OBPI.

Figure 7. Nath-modified Mallet functional movements of a 3-year-old male patient before BP neurolysis (upper panel) and images of the same patient 3.8 years after BP neurolysis with significant improvement to near-normal functional movements (lower panel).
Improvements in patients with C5-T1 injury after BP neurolysis
External rotation and hand-to-spine or back movements significantly improved from a Mallet grade of 2 to 4 in patient 6 in Table 1. Hand-to-neck movements improved from a Mallet score of 3 to 5 in patient 15 in Table 1. Patient 22 in Table 1 improved all upper-limb functional movements except supination and hand-to-spine.
We found that the postoperative follow-up time was weakly associated with improvement in the Nath-modified total Mallet functions (R = 0.17, P = .0003). There were no significant postoperative complications in any of the patients in this report.
Figure 7 shows representative patient images of the Nath-modified Mallet functional movements of a 3-year-old male patient before BP neurolysis and pictures of the same patient 3.8 years after BP neurolysis, with significant improvement to near-normal functional movements.
Discussion
Though the injury patterns are significantly different in OBPI and traumatic brachial plexus injury (TBPI) patients, neuroma, or scar formation at the site of the lesion resulting from nerve injury and compression by surrounding connective tissue and scarred scalene muscles, is similar. Decompression and BP neurolysis are performed on both obstetric and adult TBPI and long-thoracic nerve injuries.5,6,10-27,35,36 Studies have demonstrated that neurolysis improved nerve conduction,36,37 muscle grade, and functional movements in OBPI patients.5,6,10-28 We and other investigators 35, 36 have demonstrated rapid recovery and long-term improvements in upper-limb functions after neurolysis in patients with long-thoracic nerve injury35,36 and neurogenic thoracic outlet syndrome.38. The postoperative follow-up time was weakly associated with improved total modified Mallet functions in OBPI patients in this report.
Chin et al20 showed that about two-thirds of surgically treated OBPI patients (22 of 32) underwent neurolysis alone, which resulted in good recovery of abduction and elbow flexion but poor recovery of external rotation. Postoperatively, 78% of patients in our report achieved a Mallet score of 4 or 5/5 in external rotation.
Clarke et al11 reported that neurolysis alone showed functional recovery in patients with upper trunk injury but not in patients with total plexus injury (C5-T1). In contrast to those findings, El-Gammal et al26showed that OBPI patients with lower trunk palsy also achieved a total Raimondi score after neurolysis. Further, these authors26 recently performed neurolysis in 57.6 % (n = 15) of OBPI patients and demonstrated functional recovery in shoulder abduction, external rotation, and elbow flexion in 4 of 6 late-presenting cases.
Andrisevic et al13 reported that 14 of 16 OBPI patients achieved elbow flexion, and 11 of 16 patients regained shoulder abduction after neurolysis performed in infants with neuroma-in-continuity with over 50% conduction.
Among the 40 patients in this report, 37 (93%) achieved a Mallet grade of 5/5 (n = 23, 58%) or 4/5 (n = 14, 35%) in shoulder abduction after BP neurolysis. The other 3 patients had a Mallet grade of 3/5 (90 degrees) postoperatively in shoulder abduction.
Functional recovery is weeks to months in complete axonal and demyelinating injuries. Nine patients with less than 6-month postoperative follow-ups in our report show that functional recovery was not due to the completion of nerve regeneration but was reversed once the compression was relieved by nerve decompression and internal and external neurolysis of the densely formed scar tissue. By directly measuring the nerve conduction before and after surgical procedures, we found that the nerve conduction improved after the decompression and neurolysis.36,37
In addition, McComas39-41 demonstrated that neurapraxic injuries could be rapidly reversed once the compression was relieved by neurolysis, as the conduction is obstructed at the site of compression caused by neural fibrosis.6,42 In these clinical situations, peripheral nerves may remain anatomically intact; however, since lesions in continuity can be reversed even after prolonged paralysis through decompression and neurolysis, signal conduction may be compromised due to slowed axonal transport by chemical factors.9,34
Conclusions
Among the patients, 37 (93%) achieved a Mallet grade of 5/5 or 4/5 in shoulder abduction after surgery with a mean follow-up of 2 years. All upper limb functional movements improved significantly as BP neurolysis improves axonal transport to the target muscles after surgically removing the external and internal scarring of the upper trunk and its terminal branches. Additionally, neurolysis decompresses the BP from external compression by the surrounding connective tissues and densely scarred scalene muscles. Thus, it can provide these patients with an effective and rapid functional recovery. These children and their parents are pleased with the progress and increased ability to perform their activities of daily living after surgery.
Acknowledgments
Authors: Rahul K. Nath, MD; Chandra Somasundaram, PhD
Affiliation: Texas Nerve and Paralysis Institute, Houston, Texas
Correspondence: Rahul K. Nath, MD; rnath@drnathmedical.com
We thank the patients and their families who participated in this study.
Informed consent: Patients were treated ethically in compliance with the Helsinki Declaration. Documented informed consent was obtained for all patients. The patient provided written consent to use the images in this report.
Disclosures: The authors disclose no relevant financial or nonfinancial interests.
References
- Simona Z, Francesco PB, Fabrizio S, et al. Obstetric brachial plexus palsy: a population-based retrospective case-control study and medicolegal considerations. J Matern Fetal Neonatal Med. 2018;31(11):1412-1417. doi:10.1080/14767058.2017.1317737
- Buchanan PJ, Grossman JAI, Price AE, Reddy C, Chopan M, Chim H. The use of botulinum toxin injection for brachial plexus birth injuries: a systematic review of the literature. Hand (N Y). 2019 Mar;14(2):150-154. doi:10.1177/1558944718760038
- Pondaag W, Malessy MJA, van Dijk JG, et al. Natural history of obstetric brachial plexus palsy: a systematic review. Dev Med Child Neurol. 2004;46(2):138-144. doi:10.1017/s0012162204000258
- Dorich JM, Whiting J, Plano Clark VL, Ittenbach RF, Cornwall R. Impact of brachial plexus birth injury on health-related quality of life in adulthood: a mixed methods survey study. Disabil Rehabil. 2023:1-14. doi:10.1080/09638288.2023.2212917
- McQuarrie IG. Peripheral nerve surgery. Neurol Clin. 1985;3(2):453-466.
- Sakurai M, Miyasaka Y. Neural fibrosis, and the effect of neurolysis. J Bone Joint Surg Br. 1986;68(3):483-488. doi:10.1302/0301-620X.68B3.3015976
- MacKinnon SE, Dellon AL. Surgery of the peripheral nerve. New York: Thieme Medical; 1988.
- Sunderland S. Nerve injuries and their repair: a critical appraisal. Melbourne: Chuchill Livingstone; 1991.
- Tannemaat MR, Korecka J, Ehlert EM, et al. Human neuroma contains increased levels of semaphorin 3A, which surrounds nerve fibers and reduces neurite extension in vitro. J Neurosci. 2007;27(52):14260-14264.
- Terzis JK, Kokkalis ZT. Pediatric brachial plexus reconstruction. Plast Reconstr Surg. 2009;124(6 Suppl):e370-e385. doi:10.1097/PRS.0b013e3181bcf01f
- Clarke HM, Al-Qattan MM, Curtis CG, Zuker RM. Obstetrical brachial plexus palsy: results following neurolysis of conducting neuromas-in-continuity. Plast Reconstr Surg. 1996;97(5):974-982; discussion 983-984. doi:10.1097/00006534-199604001-00014
- Gosk J, Rutowski R, Urban M, Wiącek R, Mazurek P, Wnukiewicz W. Neurolysis of the conducting neuroma-in-continuity in perinatal brachial plexus palsy - evaluation of the results of surgical treatment. Folia Neuropathol. 2011;49(3):197-203.
- Andrisevic E, Taniguchi M, Partington MD, Agel J, Van Heest AE. Neurolysis alone as the treatment for neuroma-in-continuity with more than 50% conduction in infants with upper trunk brachial plexus birth palsy. J Neurosurg Pediatr. 2014;13(2):229-237. doi:10.3171/2013.10.PEDS1345
- Al-Qattan MM, El-Sayed AA. A case of Klumpke's obstetric brachial plexus palsy following a Cesarean section. Clin Case Rep. 2016;4(9):872-875. doi:10.1002/ccr3.644
- Patra S, Narayana Kurup JK, Acharya AM, Bhat AK. Birth brachial plexus palsy: a race against time. BMJ Case Rep. 2016;2016:bcr2016215996. doi:10.1136/bcr-2016-215996.
- Pondaag W, Malessy MJ. Neurolysis and upper trunk brachial plexus birth palsy. J Neurosurg Pediatr. 2014;14(3):322-324. doi:10.3171/ped.2014.14.3.18
- Chantaraseno N, Precha V, Supichyangur K, Cholpranee K. Brachial plexus birth palsy: the natural history, outcome of microsurgical repair and operative reconstruction. J Med Assoc Thai. 2014;97 Suppl 11:S96-S101.
- Pondaag W, Malessy MJA. Evidence that nerve surgery improves functional outcome for obstetric brachial plexus injury. J Hand Surg Eur Vol. 2021;46(3):229-236. doi:10.1177/1753193420934676
- Lin JC, Schwentker-Colizza A, Curtis CG, Clarke HM. Final results of grafting versus neurolysis in obstetrical brachial plexus palsy. Plast Reconstr Surg. 2009;123(3):939-948. doi:10.1097/PRS.0b013e318199f4eb
- Chin KF, Misra VP, Sicuri GM, Fox M, Sinisi M. Intra-operative neurophysiological prediction of upper trunk recovery in obstetric brachial plexus palsy with neuroma in continuity. Bone Joint J. 2013;95-B (5):699-705. doi:10.1302/0301-620X.95B5.30948
- Laurent JP, Lee RT. Birth-related upper brachial plexus injuries in infants: operative and nonoperative approaches. J Child Neurol. 1994;9(2):111-117; discussion 118. doi:10.1177/088307389400900202
- Gilbert A, Pivato G, Kheiralla T. Long-term results of primary repair of brachial plexus lesions in children. Microsurgery. 2006;26:334-342. doi:10.1002/micr.20248
- Buterbaugh KL, Shah AS. The natural history and management of brachial plexus birth palsy. Curr Rev Musculoskelet Med. 2016;9:418-426. doi:10.1007/s12178-016-9374-3
- Grossman JA, DiTaranto P, Yaylali I, Alfonso I, Ramos LE, Price AE. Shoulder function following late neurolysis and bypass grafting for upper brachial plexus birth injuries. J Hand Surg Br. 2004;29(4):356-358. doi:10.1016/j.jhsb.2004.03.008
- Shenaq SM, Kim JY, Armenta AH, Nath RK, Cheng E, Jedrysiak A. The surgical treatment of obstetric brachial plexus palsy. Plast Reconstr Surg. 2004;113(4):54E-67E. doi:10.1097/01.prs.0000110215.61220.72
- El-Gammal TA, El-Sayed A, Kotb MM, et al. Total obstetric brachial plexus palsy: results and strategy of microsurgical reconstruction. Microsurgery. 2010;30(3):169-78. doi:10.1002/micr.20726
- El-Gammal TA, El-Sayed A, Kotb MM, et al. Long-term results of microsurgical brachial plexus reconstruction in late-presenting cases of brachial plexus birth injury. J Hand Surg Am. 2023;48(2):126-133. doi:10.1016/j.jhsa.2022.11.003
- Wells ME, Tihista MC, Diamond S. Brachial plexus birth injury: trends in early surgical intervention over the last three decades. Plast Reconstr Surg Glob Open. 2022;10(5):e4346. doi:10.1097/GOX.0000000000004346
- Mallet J. Obstetrical paralysis of the brachial plexus. II. Therapeutics. Treatment of sequelae. Results of different therapeutic techniques and therapeutic indications. Rev Chir Orthop Reparatrice Appar Mot. 1972;58(Suppl 1):192-196.
- Nath RK, Liu X, Melcher SE, Fan J. Long-term outcomes of triangle tilt surgery for obstetric brachial plexus injury. Pediatr Surg Int. 2010;26(4):393-399. doi:10.1007/s00383-010-2550-4
- Nath RK, Karicherla P, Mahmooduddin F. Shoulder function and anatomy in complete obstetric brachial plexus palsy: long-term improvement after triangle tilt surgery. Childs Nerv Syst. 2010;26(8):1009-1019. doi:10.1007/s00381-010-1174-2
- Nath RK. Obstetric brachial plexus injuries - Erb’s palsy: the Nath method of diagnosis and treatment. College Station, TX: VirtualBookworm.com Publishing; 2007.
- Thatte MR, Shah HR, Hiremath A. Birth brachial plexus palsy: an Indian perspective. Semin Plast Surg. 2023;37(2):117-133. doi:10.1055/s-0043-1767782
- Huber AB, Kania A, Tran TS, et al. Distinct roles for secreted semaphorin signaling in spinal motor axon guidance. Neuron. 2005;48(6):949-64. doi:10.1016/j.neuron.2005.12.003
- Burton JS, Mackinnon SE, McKee PB, Henderson KM, Goestenkors DM, Thompson RW. Rapid functional recovery after thoracic outlet decompression in a series of adolescent athletes with chronic atraumatic shoulder-girdle pain, scapular winging/dyskinesis, and normal electrodiagnostic studies. Hand (N Y). 2023:15589447231187088. doi:10.1177/15589447231187088
- Nath RK, Melcher SE. Rapid recovery of serratus anterior muscle function after microneurolysis of long thoracic nerve injury. J Brachial Plex Peripher Nerve Inj. 2007; 2:4. doi:10.1186/1749-7221-2-4
- Nath RK, Somasundaram C. Significant improvement in nerve conduction, arm length, and upper extremity function after intraoperative electrical stimulation, neurolysis, and biceps tendon lengthening in obstetric brachial plexus patients. J Orthop Surg Res. 2015;10:51. doi:10.1186/s13018-015-0191-y
- Yoshizumi T, Murata H, Kanno H, Shinonaga M. Efficacy of supraclavicular scalenotomy followed by external neurolysis without rib resection for post-traumatic neurogenic thoracic outlet syndrome. Spine (Phila Pa 1976). 2021;46(11):E632-E638. doi:10.1097/BRS.0000000000003859
- McComas AJ, Jorgensen PB, Upton AR: The neurapraxic lesion: a clinical contribution to the study of trophic mechanisms. Can J Neurol Sci. 1974,1(3):170-179.
- McComas AJ, White CM. Distal dysfunction, and recovery in ulnar neuropathy. Muscle Nerve. 1996;2(12):1617-1619.
- McComas AJ, DeBruin H, Quartly C. In: Plasticity of motoneuronal connections. Wernig A, ed. Amsterdam; Elsevier; 1991. Non-transmitting synapses in human neuromuscular disorders? pp. 223-229.
- Kim DH, Han K, Tiel RL, Murovic JA, Kline DG: Surgical outcomes of 654 ulnar nerve lesions. J Neurosurg. 2003;98(5):993-1004. doi:10.3171/jns.2003.98.5.0993