Utility of Ultrasound in Performing a Reverse Allen’s Test in Patients At Risk for Radial Artery Occlusion
© 2023 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of ePlasty or HMP Global, their employees, and affiliates.
Questions
1. What is a reverse Allen’s test, and how does it differ from an Allen’s test?
2. What is the utility of performing a reverse Allen’s test prior to attempting cannulation of the radial artery?
3. Does using ultrasound offer benefits over the conventional method?
4. Are there any risks or adverse consequences to using ultrasound to perform this test?
Case Description
A 30-year-old male multi-trauma patient was transferred from the surgical intensive care unit (SICU) to the operating room (OR) for open reduction and internal fixation (ORIF) of his orthopaedic injuries. The anesthetic plan included the insertion of an arterial catheter for continuous blood pressure monitoring and periodic blood sampling. Only the right upper extremity was available for arterial cannulation due to injuries to the left upper extremity and pelvis. Upon admission to the OR it was observed that the patient had undergone previous arterial blood gas punctures to the right radial artery while in the ICU. A distal radial pulse was present on physical exam. Due to concern for proximal radial artery occlusion, a reverse Allen’s test was performed and revealed loss of the distal radial pulse with occlusion of the ulnar artery. Ultrasound (US) visualization of the radial artery confirmed the presence of a distal radial pulse and the absence of radial artery pulsation proximally. US confirmed the loss of the distal radial pulse during occlusion of the ulnar artery. An arterial catheter was placed uneventfully into the brachial artery using US guidance, and the case proceeded as planned.
Q1. What is a reverse Allen’s test, and how does it differ from an Allen’s test?
Blood flow to the hand is supplied by the radial artery laterally and ulnar artery medially, forming anastomotic palmar arches distally.1 The original Allen’s test was developed in 1929 by Dr Edgar Allen as a technique to diagnose thromboangiitis obliterans of ulnar artery.2 A modified Allen’s test has since replaced the original and is intended to assess the adequacy of the ulnar artery to perfuse the hand prior to instrumenting the radial artery. This test begins with the patient exsanguinating the hand by tightly clenching the fist as the examiner simultaneously compresses the distal ulnar and radial arteries. The fist is then unclenched, revealing pallor of the hand. Normally, the release of pressure on the ulnar artery will promptly restore perfusion to the hand, generally within 10 seconds. A negative test suggests blood flow from the ulnar artery alone will adequately perfuse the hand should blood flow from the radial artery become impaired. Performing this test in “reverse” is performed by palpating the distal radial artery and then occluding the ulnar artery to demonstrate patency of the radial artery. The loss of a distal radial pulse with occlusion of the ulnar artery confirms radial artery occlusion (RAO).
Q2. What is the utility of performing a reverse Allen’s test prior to attempting cannulation of the radial artery?
The incidence of RAO varies widely, ranging from 0.8% upwards to 38%, and is especially common in patients with prior radial artery cannulation as is often seen in ICU patients.3 Though the modified Allen’s test is taught to assess the sufficiency of collateral blood flow to the hand prior to cannulation, the evidence fails to support that it is a useful clinical predictor of an increased risk for ischemic complications in the setting of RAO.4 In our case, the patient had an occlusion of the radial artery with preservation of a palpable distal radial pulse, occurring from the transmission of the ulnar pulse wave across the palmar arch. This finding was revealed by performing a reverse Allen’s test and confirmed using doppler US demonstrating the absence of pulsatile flow in the proximal radial artery. Failing to recognize this proximal arterial occlusion would have resulted in unsuccessful efforts to cannulate the radial artery and a delay in surgical start time.

Q3. Does using ultrasound offer benefits over the conventional method?
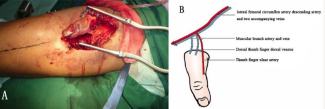
US guidance is often used to assist with the insertion of arterial cannulae for the purpose of continuous blood pressure monitoring and periodic blood sampling. Our case demonstrates the additional benefit of using US to visualize the radial and ulnar arteries prior to radial artery cannulation in order to assess the patency and flow within these arteries and provide an objective assessment of the suitability for cannulation. We believe that using US is superior to using the clinical exam alone. The ready availability of ultrasound in current practice supports performing this assessment prior to attempted arterial cannulation, particularly in patients with prior instrumentation of the artery. US permits clinicians to visualize the radial artery and distinguish true patency of the radial artery from the presence of distal radial pulse transmitted from the ulnar artery across the palmar arch in the presence of proximal RAO (Figure 1).
Q4. Are there any risks or adverse consequences to using ultrasound to perform this test?
As the use of US visualization is noninvasive and easily performed, there are no contraindications to using this method. The additional benefit of using US diagnostically is that it can be further used to assist with the cannulation of the artery under direct vision, thereby increasing the probability of successful cannulation.
Our trauma patient presented in the OR requiring arterial cannulation with the right extremity as the only reasonable candidate for arterial cannulation due to the nature of his injuries. Proximal RAO was diagnosed via reverse Allen’s test and confirmed with US guidance. The brachial artery was then accessed uneventfully, and the case proceeded without further issue.
Acknowledgments
Affiliation: 1Department of Anesthesiology, University of Oklahoma Health Science Center, Oklahoma City, Oklahoma; 2Department of Anesthesiology and Critical Care Medicine, Johns Hopkins School of Medicine. Baltimore, Maryland
Correspondence: Kevin B Gerold, DO; kgerold@jhmi.edu
Disclosures: The authors disclose no financial or other conflicts of interest.
References
- Sgueglia GA, Di Giorgio A, Gaspardone A, Babunashvili A. Anatomic Basis and Physiological Rationale of Distal Radial Artery Access for Percutaneous Coronary and Endovascular Procedures. JACC Cardiovasc Interv. 2018;11(20):2113-2119. doi:10.1016/j.jcin.2018.04.045
- Foreman A, de Almeida JR, Gilbert R, Goldstein DP. The Allen's test: revisiting the importance of bidirectional testing to determine candidacy and design of radial forearm free flap harvest in the era of trans radial endovascular access procedures. J Otolaryngol Head Neck Surg. 2015;44:47. Published 2015 Nov 4. doi:10.1186/s40463-015-0096-0
- Rashid M, Kwok CS, Pancholy S, et al. Radial Artery Occlusion After Transradial Interventions: A Systematic Review and Meta-Analysis. J Am Heart Assoc. 2016;5(1):e002686. Published 2016 Jan 25. doi:10.1161/JAHA.115.002686
- Brzezinski M, Luisetti T, London MJ. Radial artery cannulation: a comprehensive review of recent anatomic and physiologic investigations. Anesth Analg. 2009;109(6):1763-1781. doi:10.1213/ANE.0b013e3181bbd416