Our Experience With Glabrous Skin Grafts for Hand Injuries
Abstract
Background. Hand injuries requiring skin cover may utilize skin harvested from the instep of the foot. We present a series of such cases with a follow-up period of 6 months following glabrous skin grafting.
Objectives. To evaluate the aesthetic and functional outcome of using glabrous skin to cover skin defects in the hand.
Methods. All patients with raw areas of the hand who presented to our institution’s department of plastic surgery between August 2021 and August 2022 were included in the study. The Patient and Observer Scar Assessment Scale (POSAS) was used to serially assess the quality of scar over a period of 6 months. The instep of either foot was chosen as the donor site. POSAS scores for the resulting scar were collected at 1 month, 3 months, and 6 months postoperatively. Outcomes were analyzed using SPSS software
Results. A total of 15 cases were included in the study. Average preoperative POSAS score by patients was found to be 52/60, whereas the average score given by the observer (physician) was 51/60. At 1 month after glabrous skin grafting, patients scored an average of 33/60, whereas the average observer score was 31/60. At 3 months, there was marked improvement in quality of the scars, with an average patient score of 20/60 and observer score of 19/60. At the final follow-up of 6 months, most patients had minimum symptoms and reported an average score of 7/60 and observer score of 6.2/60.
Conclusions. In our study, we found excellent graft uptake, good functional outcome, adequate color match, improved scar quality, and minimal donor site scarring.
Introduction
Glabrous skin is the non–hair-bearing skin of the palm and sole that is thicker than the skin over the rest of the body. The epidermis of the skin has 4 layers: the stratum basale, stratum spinosum, stratum granulosum, and stratum corneum. The glabrous skin is specialized as it has an additional layer, stratum lucidum.1 Hand injuries often result in a loss of skin cover in addition to other components, such as soft tissue, tendons, ligaments, and bone. It is important to provide an early cover to ensure good functional and aesthetic outcome. These injuries may result from a multitude of causes, including burns, road traffic accidents, industrial and machine injuries, infections, or ring avulsion injuries.2
We present a series of cases in which glabrous grafts from the instep of foot were used to cover defects over the palmar aspect of hand.
OBJECTIVE
To evaluate aesthetic and functional outcomes in patients for whom glabrous skin was used to cover skin defects in the hand.
Materials and Methods
Inclusion and Exclusion Criteria
Patients of any age group, including children, were deemed eligible for inclusion. We reviewed all cases of burn-related contracture of the hand, posttraumatic ulcer of the hand, and ulcers of hand secondary to cellulitis that were evaluated in patients presenting to the department of plastic surgery for surgical management. Patients unwilling to consent to participate in the study were not included.
Statistical Methods
Data collected are presented in the form of tables and charts created using Microsoft Excel and analyzed with the help of SPSS (IBM Corp) software. Result was considered as statistically significant if P value was <0.5

Tools Used
The Patient and Observer Scar Assessment Scale (POSAS) Version 2.0 (Figure 1) was used to determine observer (physician) and patient assessment of 6 items: vascularity, pigmentation, thickness, relief, pliability, and surface area. All items were scored on a scale of 1 to 10. It is a standardized scale for scar assessment from patient and clinician perspective.
Detailed Description of Procedure and Processes
After obtaining Institutional Ethical Committee clearance, patients presenting to plastic surgery department were recruited into this study. This is a prospective study that included all patients who fit the inclusion criteria and who presented to our department between August 2021-2022. After obtaining written and informed consent, data pertaining to basic patient demographics, causal event (eg, history of burns), prior treatment details (if any), and comorbid conditions that may affect wound healing were collected in a questionnaire format by the investigators. Factors that might have caused delayed or suboptimal wound healing were noted, such as connective tissue disorders, skin diseases that cause delayed or poor wound healing, previous surgeries in the potential donor sites, smoking history, and steroid usage.
For each patient, an intermediate-thickness (0.3-0.6 mm) glabrous graft was harvested from the instep of the foot and used to cover the raw areas after debridement. On follow-up visits at 1 month, 3 months, and 6 months, the subjects underwent clinical examination, colorimeter assessment, scar assessment using the POSAS tool, and functional assessment of both the grafted and donor sites. We conducted functional assessments by evaluating range of motion of 2 joints: one above and one below the graft site. Postoperative complications were noted, including graft loss, postoperative surgical site infections, and donor site pain. Contracture reformation and other subjective complications were also noted. After a subject completed 6 months of follow-up assessments, their data were analyzed.
Results
A total of 15 patients were included in the study. Of these, 12 patients had raw areas over the fingers, and 3 had raw areas mostly over the palmar area. The average preoperative POSAS score of patients was found to be 52/60 whereas the average observer score was 51. This suggests a commonality in opinion between the patients and observer regarding the scar quality.
At 1 month after glabrous skin grafting, patients reported an average POSAS score of 33/60 and the average observer score was 31/60. These reductions suggest marked improvement in symptoms and appearance of the scar after grafting. At 3 months, there was marked improvement in scar quality as reflected in the average patient score of 20/60 and observer score of 19/60.

At the final follow-up examination at 6 months, most patients had minimum symptoms and reported an average POSAS score of 7/60 and observer score of 6/60. One patient of the 15 participants reported re-contracture along the longitudinal margin of the graft over the proximal interphalangeal joint of the second digit. Overall functional and aesthetic outcome was satisfactory at the end of 6 months. Donor sites healed well with good scar outcomes and no functional deficits. The results are summarized in Table 1.
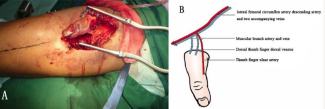
Figures 2, 3, 4, and 5 are clinical photographs of glabrous grafts performed for various indications.




Discussion
In one of the largest studies to explore glabrous skin grafts, Sohail et al examined outcomes for intermediate-thickness glabrous skin grafts in 74 patients with palmar contractures after burn injuries.3 The authors reported observations regarding intraoperative methods, postoperative complications with respect to the donor site, and long-term follow up results. They concluded that donor site healing was rapid, and weight-bearing capacity was not affected by the selection of donor site.3 The long-term follow-up results with respect to color and texture match was akin to our study.
In a study of 48 cases of hand contractures after burn injuries, Sridhar et al evaluated the outcomes of full-thickness grafts on raw areas over skin defects following contracture release.4 The authors concluded that, in a pediatric population, full-thickness grafts tended to grow with age and hence provided a good outcome. In our study, which did not include pediatric patients, we found only 1 instance of re-contracture after glabrous graft placement.
In a comparative analysis of full-thickness grafts and glabrous grafts in pediatric hand defects by Elrod et al, the authors found superior colorimetric results with glabrous grafts.5 They used the Vancouver Scar Scale and POSAS to analyze their patients’ perception of healing and found better results in the glabrous group. Our study used POSAS scores to serially evaluate patient and observer analysis of the scar outcome. At the end of 6 months, we found remarkable patient satisfaction as evidenced by an average patient POSAS score of 7. The color match was comparable to surrounding skin, and symptoms like itching, erythema, and scar thickening were minimal. In the Elrod et al study, donor site coverage was accomplished through the “Zurich move,” a technique in which the glabrous donor site was covered with a split-thickness skin graft.5 We, however, allowed our donor sites to heal through use of dressings and wound care similar to that employed for other graft donor sites. For all of our included patients, donor sites healed well with negligible scarring at the end of 6 months.
After reviewing the literature on glabrous grafts, most studies have been conducted in pediatric populations. We attribute this to reduced availability of glabrous grafts large enough to cover such areas as the entire palmar aspect of an adult patient. Friel et al conducted a retrospective review of palmar skin burns in a pediatric burn center and identified 17 patients who underwent glabrous grafts over a period of 2 and a half years.6 They found excellent long-term functional and aesthetic outcomes in all cases, much like our study.6
Limitations
Lack of a control group may be considered as a limitation of this study. A larger case-control study may be designed to compare the outcomes of glabrous grafts with other types of skin grafts.
Conclusions
Using glabrous skin harvested from the instep of the sole of the foot to cover raw areas of the hand is an approach that adheres to the important plastic surgery principle of replacing “like with like.” In our study, we found excellent graft uptake, good functional outcome, adequate color match, improved scar quality, and minimal donor site scarring.
Acknowledgments
Affiliation: 1Department of Plastic Surgery, Kasturba Medical College, Manipal Academy of Higher Education, Karnataka, India
Correspondence: Divya Syam, MCh; divyasyam92@gmail.com
Ethics: Institutional Review Board approval was obtained for this study, and written and informed consent was obtained from all study participants. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Disclosures: The authors disclose no relevant conflict of interest or financial disclosures for this manuscript.
References
1. Bonifant H, Holloway S. A review of the effects of ageing on skin integrity and wound healing. Br J Community Nurs. 2019 Mar 1;24(Sup3):S28-S33. doi:10.12968/bjcn.2019.24.Sup3.S28
2. Krishnamoorthy R, Karthikeyan G. Degloving injuries of the hand. Indian J Plast Surg. 2011;44:227-236. doi:10.4103/0970-0358.85344
3. Sohail M, Hussain M, Mustehsan Bashir M, et al. Outcome of coverage of post burn palmar hand contractures with glabrous intermediate-thickness plantar (ITP) skin graft. Ann King Edward Med Univ. 2017;23(3):274-278. doi:10.21649/akemu.v23i3.2008
4. Sridhar R, Hariharan NC. Reconstruction of post-burn contracture of fingers. Int J Sci Study. 2017;55(2):55-58. doi:10.17354/ijss/2017/215
5. Elrod J, Moellmeier D, Schiestl C, Mohr C, Neuhaus K. Comparative analysis of functional and aesthetic outcomes of retroauricular full thickness versus plantar glabrous split thickness skin grafts in pediatric palmar hand burns. Burns. 2020 May 1;46(3):639-646. doi:10.1016/j.burns.2019.09.004
6. Friel MT, Duquette SP, Ranganath B, Burkey BA, Glat PM, Davis WJ. The use of glabrous skins grafts in the treatment of pediatric palmar hand burns. Ann Plast Surg. 2015 Aug 25;75(2):153-157. doi:10.1097/SAP.0000000000000558