Good Outcomes After a Severity Triad: Systemic Complications, Bacterial and Fungal Infections in 3 Patients With Major Burns
© 2024 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of ePlasty or HMP Global, their employees, and affiliates.
Abstract
Burn injuries resulting from domestic explosions involving liquefied petroleum gas present complex challenges in clinical management. We present 3 cases of patients with severe burn injuries, highlighting diverse presentations and complications encountered during their treatment. Despite significant morbidity, all patients demonstrated favorable outcomes, emphasizing the importance of comprehensive management strategies. Challenges included inhalation injury, microbial infections, thromboembolic complications, and acute kidney injury. Aggressive treatment modalities, including bronchoscopy-guided therapy, targeted antimicrobial therapy, and vigilant infection control, effectively addressed these complications. Multidisciplinary collaboration and adherence to evidence-based guidelines optimized outcomes. Continued research and innovation are needed to further enhance care and improve long-term outcomes for patients with severe burns.
Introduction
Burn injuries continue to pose significant challenges in clinical management due to their complex pathophysiology and potential for severe complications. The complexity of burn injuries lies not only in their immediate tissue damage but also in their potential to trigger a cascade of systemic complications and the potential for multiple organ dysfunction syndrome. Patients with extensive burn injuries often require multidisciplinary care and tailored treatment strategies to address not only the immediate consequences of thermal injury but also the systemic effects that can ensue.1-3
In this context, understanding the clinical course, complications, and therapeutic interventions in individual cases can provide valuable insights into the management of burn patients. We present the cases of 3 women with severe burns who developed bacterial and fungal complications. These cases highlight the diverse presentations and complications that may arise following burn injuries, including respiratory compromise, infectious complications, and renal dysfunction.4In addition to addressing primary burn injuries, effective management strategies were crucial in mitigating secondary complications, including microbial infections, thromboembolic events, and acute kidney injury. These complications, although common in burn patients, were successfully managed through early diagnosis, aggressive treatment modalities, targeted antimicrobial therapy, and infection control measures.
Case Presentations
Case 1
A 56-year-old female patient, with no known comorbidities, was transferred to our burn center from the regional hospital after the explosion of a liquefied petroleum gas (LPG) domestic cylinder in a closed space (her kitchen) 9 hours prior. She had second- and third-degree burns, with a total body surface area (TBSA) of 50%, including burns on the face, trunk, both upper limbs circumferential, the left thigh, both calves circumferential, and foot. Inhalation injury was suspected at admission. Escharotomies were performed in the regional hospital on both forearms and left calf (Figure 1). The Abbreviated Burn Severity Index (ABSI) score was 11 (probability of survival 20%-40%).

Figure 1. Burn wounds at admission.
After admission, she was intubated and mechanically ventilated and underwent surgery, consisting of performing fasciotomies of both forearms, bilateral carpal tunnel release, and escharotomies and fasciotomies on the dorsal side of both hands. On day 3 the incisions were sutured. Afterward, she underwent 2 excisions of the burn wounds on the upper limbs and grafting with split-thickness grafts from both thighs and abdomen. The rest of the burns healed spontaneously.
Fiberoptic bronchoscopy on day 1 showed airway edema and hyperemia. She underwent aggressive pulmonary toilet, chest physiotherapy, airway suctioning, bronchodilator treatment, and muscarinic receptor antagonist treatment. Bronchial aspirate collected by suctioning secretions from the lower airways during a bronchoscopy was sent for microbiological culture and Pseudomonas aeruginosa was identified (10,000 UFC/mL MDR); therefore, systemic treatment with colistin was initiated for 10 days. Aerosolized colistin inhalation (1 million IU q 8h) was associated with salbutamol/ipratropium aerosols. She was extubated on day 6. After extubation, the patient’s vital signs, including blood pressure, heart rate, and oxygen saturation, were monitored to ensure they were within normal limits. The patient showed no signs of respiratory distress, such as shortness of breath, coughing, or wheezing. She had persistent dysphonia due to her inhalation injury.
On day 30, blood cultures were collected and procalcitonin was measured (9.9 ng/mL). Burned wound cultures and blood cultures showed Pseudomonas aeruginosa, and colistin and piperacillin/tazobactam were started for 14 days. On day 38 another set of blood cultures was collected and results showed Candida parapsilosis, sensible to anidulafungin. In consequence, anidulafungin was added to colistin and piperacillin/tazobactam and was administered for 14 days.
On day 40, right iliac thrombosis was diagnosed through duplex ultrasound, left femoral central venous catheter. Computed tomography (CT) pulmonary angiography showed no signs of pulmonary embolism. The patient started treatment with a therapeutic dose of dalteparin and continued with apixaban after being discharged.
On day 47 blood cultures were collected again and results showed Pseudomonas aeruginosa, and another course of colistin was started, this one for 7 days. On day 54 blood cultures were negative. On day 60 the patient was discharged. She received a prescription for apixaban 5 mg bid for at least 3 months and an indication to be monitored by a cardiologist in her regional hospital. She returned to the ambulatory setting for follow-up (Figure 2).

Figure 2. Day 120 postburn (follow-up).
Case 2
A 31-year-old female patient with no known comorbidities was transferred from the regional hospital to our burn center with second- and third-degree burns having 55% TBSA burned after the explosion of a LPG domestic cylinder at her house 2 hours before. She had burns on her face, neck, upper limbs, gluteal region, and lower limbs. Her ABSI score was 10 (probability of survival 20%-40%).
On day 19, burned wound cultures showed Pseudomonas aeruginosa multidrug resistant (MDR), and treatment with colistin was initiated, to last for 14 days. On day 27, burned wound cultures showed both Pseudomonas aeruginosa and Aspergillus, while blood cultures were negative. Ceftazidime-avibactam was added for 14 days to the previous treatment with colistin. On day 37, burned wound cultures were negative.
On day 50, the patient showed an increase in serum creatinine to 1.76 mg/dL; eGFR = 40 mL/min/1.73 m2 – CKD-EPI; normal blood urea levels; and hypokalemia (3.09 mmol/L). The 24-hour urinalysis showed the following: creatinine: 32.1 mg/dL; glucose: 0.20 g/L; potassium: 29.1 mmol/L; proteins: 0.48 g/L; sodium: 107 mmol/L; urea: 246 mg/dL. Urine culture was negative. In the following days, creatinine levels gradually increased, and the nephrologist established the diagnosis of drug-related acute kidney injury (AKI), due to antibiotics and nonsteroidal anti-inflammatory drugs, and recommended that all nephrotoxic drugs must be stopped. On day 55 creatinine was 3.5 mg/dL, urea = 52.4 mg/dL, and creatinine clearance = 14.9 mL/min/1.73 m2. The patient was discharged on day 55 postburn injury against medical advice.
She returned to the ambulatory care department on day 59, when creatinine decreased to 2.3 mg/dL, and on day 66 (Figure 3), when creatinine was 1.1 mg/dL.

Figure 3. Day 66 postburn (follow-up).
Case 3
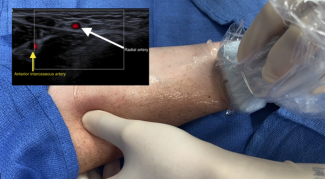
A 39-year-old female, with no known comorbidities, was referred to our burn center from the regional hospital. She suffered full- and partial-thickness burns on 45% TBSA due to the explosion of a LPG domestic cylinder in an enclosed space (her kitchen) 6 hours prior. She was intubated and mechanically ventilated before arrival. She had partial-thickness burns on the face and neck, with important face edema; full- and partial-thickness burns on the anterior and posterior thorax, abdomen, lumbar region, and both upper limbs with circumferential distribution on the forearms and hands, with burn-induced compartment syndrome; and full- and partial-thickness burns on the knees, calves, and legs. The patient’s ABSI score was 10 points (survival probability of 20%-40%). CT scan at admission showed aspiration bronchopneumonia in the left lower lobe (Figure 4).

Figure 4. Chest computed tomography showing the presence of consolidation in the left lower lobe.
Escarotomies and fasciotomies were performed on the anterior forearms, with decompression of the carpal tunnels, and on the dorsal side of both hands. On day 3 the incisions were sutured. Afterward, full-thickness burns on upper limbs and ankles were treated by tangential excision and covered with split-thickness autografts from the thighs.
Tracheal secretion cultures taken at admission showed Aspergillus spp. (with hyphae of the fungus) and Pseudomonas aeruginosa. The galactomannan antigen test in serum was negative, and in bronchoalveolar lavage fluid samples was positive. Treatment was initiated with piperacillin/tazobactam and fluconazole. Videolaryngoscopy on day 7 showed white deposits on the tongue and pharynx. An upper endoscopy on day 9 showed nonerosive gastritis and found no signs of fungal esophagitis. On day 10, a tracheostomy was performed. On day 18, mechanical ventilation was discontinued.
Burn wound cultures on day 13 showed Acinetobacter baumannii, and tracheal secretion cultures showed Acinetobacter baumannii and Pseudomonas aeruginosa. Treatment was continued with piperacillin/tazobactam and colistin. Burn wound cultures on day 24 were sterile.
On day 46, the patient developed deep vein thrombosis on the right subclavian vein, and treatment with apixaban was initiated. She was discharged on day 57.
Discussion
Even though 1 patient had an ABSI score of 11 and the other 2 patients had an ABSI score of 10, meaning a probability of survival of 20% to 40%, all 3 patients survived. During follow-up, they were in stable condition and no other complications appeared. Ultimately, the successful outcomes observed in these cases underscore the importance of a multidisciplinary framework and adherence to evidence-based protocols in optimizing patient care.
LPG is a flammable hydrocarbon gas commonly used for heating, cooking, and as fuel for vehicles. When mishandled or in the event of a leak, LPG can pose serious burn risks due to its highly combustible nature. LPG burns can result from explosions, fires, or direct contact with the skin when the gas is in its liquid form. The severity of LPG burns depends on factors such as the concentration of the gas, the duration of exposure, and the proximity to the source of ignition or explosion.5
Currently, people in Romania, especially in the rural setting, use liquefied petroleum gas for domestic purposes, especially cooking. All 3 patients were victims of domestic explosions of LPG cylinders, which are thin pressure vessels where gas is stored in liquid form under pressure.
Pre-hospital and early in-hospital management followed advanced trauma life support principles, promoting the primary survey sequence as airway, breathing, circulation, disability, and exposure. The secondary assessment involved further history when possible, a thorough head-to-toe exam, and diagnostic testing. In all patients, CT scans were performed to diagnose head, cervical spine, internal chest or abdomen, and pelvic injury. 6,7
The 3 patients included in this case series had a TBSA of 50%, 55%, and 45% (mean TBSA 50%). Two of the 3 patients had inhalation injury documented through bronchoscopy.
A previous study on the etiological and clinical spectrum of LPG-related burns identified that the mean TBSA was 36.6%, with a higher mean TBSA in females (41.1%). Inhalation injury was present/suspected in 46.1% of cases and accounted for a high mortality rate (31.5%). As anticipated, and in line with prior research, the 3 patients were in the productive age group, with a mean age of 42 years old. This can be explained by the fact that this age group is mostly involved in handling LPG stoves in the kitchen.8
In our patients, inhalation injuries were suspected in the presence of the following findings at the physical exam: facial burns, singed facial or nasal hair, or soot or carbonaceous material on the face or in the sputum. Inhalation injury was confirmed through bronchoscopy, as data from the literature recommend.9,10
The comprehensive approach to inhalation injuries involves bronchodilators, muscarinic receptor antagonists, and inhaled mucolytic agents and anticoagulants. These therapeutic interventions aim to alleviate airway complications, enhance oxygenation, and contribute to overall better outcomes for patients with inhalation injuries.11-14
Because of weakened immune defenses and extensive wound surfaces, individuals with burn injuries are prone to acquiring several pathogens that lead to invasive infections, Resistant organisms, including bacteria such as methicillin-resistant Staphylococcus aureus, vancomycin-resistant Enterococcus, Pseudomonas, Acinetobacter, or fungal organism such as Candida species and Aspergillus emerge as the leading cause of death from infection in burns. The widespread use of both topical and systemic antibiotics, whether used as a preventive measure or in the event of a confirmed bacterial infection, contributes to the increased likelihood of developing fungal infections.15-17In addition to invasive infection of the burn wounds, pathogens might lead to septic thrombophlebitis, especially in patients with intravenous and intra-arterial lines, urinary tract infections in patients with urinary catheters or hematogenous dissemination of bacteria and fungi, respiratory tract infections and ventilator-associated pneumonia in patients with direct contamination of the airway or hematogenous dissemination.18,19
Among the 3 patients, 2 patients had burn wound infection with Pseudomonas aeruginosa MDR and 1 patient had Acinetobacter baumanii MDR. Hematogenous dissemination of Pseudomonas aeruginosa was found in 1 patient. All 3 patients had infections with ESKAPE pathogens, an acronym for Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species, which are a group of bacteria notorious for their ability to "escape" the effects of common antibiotics and cause serious infections.20 All 3 patients received colistin (polymyxin E). In burn patients, particularly those with extensive burns or who have developed MDR infections, colistin may be considered when other antibiotics have failed or when there are limited treatment options available. Its potent activity against gram-negative bacteria, including strains resistant to other antibiotics, can make it a valuable option in such cases. However, the use of colistin in burn patients requires careful consideration due to its potential nephrotoxicity and neurotoxicity, which can be exacerbated in individuals with burn injuries. Close monitoring of renal function and neurological status is essential when using colistin in this patient population to mitigate the risk of adverse effects.21,22
All 3 patients had fungal infection: a blood culture positive for Candida parapsilosis on day 38, a burn wound culture positive for Aspergillus spp on day 27, and a tracheal secretion with Aspergillus from the admission. Previous studies identified risk factors for developing fungal infections in burn patients as age, >40% burned TBSA, full-thickness burns, inhalational injury, length of hospital stay, delayed surgical treatment, open dressings, use of artificial dermis, presence of central venous catheters, administration of antibiotics and steroids, prolonged mechanical ventilation, fungal wound colonization, hyperglycemic episodes, and other conditions leading to impaired immune defense such as neutropenia and uncontrolled diabetes.1,23,24 Mortality in burn patients with fungal infections is linked to the presence of fungemia, multiple positive cultures, and the invasion of healthy skin.24
Candida parapsilosis, typically a commensal of human skin with pathogenicity limited by intact integument, is reported to be the second most commonly isolated Candida species from blood cultures, after Candida albicans. Invasive disease is often spread from sources like contaminated medical devices, catheters, and the hands of health care workers. Immunocompromised patients and those with prior antibiotic therapy or immunosuppressive therapy are at high risk for infection.25-27Candida parapsilosis fungemia has a mortality rate ranging from 23% to 30%.28-29Although there is currently a lack of consensus on the management of invasive Candida parapsilosis diseases, treatment typically involves topical therapy or systemic antifungal medication. The choice of antifungal and the duration of systemic treatment depend on the severity and location of the infection, with common drugs being fluconazole, amphotericin B, and echinocandins (caspofungin, micafungin, and anidulafungin).25
Invasive aspergillosis is an opportunistic fungal infection that poses a significant and often fatal threat to immunocompromised patients, with reported mortality rates reaching as high as 92%. Detection of galactomannan, which is a heteropolysaccharide constituent of the Aspergillus cell wall, has proven valuable for early detection of invasive aspergillosis and serves as a key biomarker. Sample specimens such as serum and bronchoalveolar lavage fluid are commonly utilized. In patients with a high risk of developing aspergillosis, there is a higher sensitivity of detection of galactomannan by immunodiagnostics in bronchoalveolar lavage samples.30,31
We recorded thromboembolic complications in 2 out of the 3 patients: 1 deep vein thrombosis on the right iliac vein in 1 patient and 1 deep vein thrombosis on the right subclavian vein in another patient. In concordance with data from the literature, we identified multiple risk factors for thrombosis in these patients: the presence of burns on the affected limb, the presence of a central venous catheter, multiple surgeries, prolonged immobilization, and burns on over 40% TBSA.32-34
Effective infection control is paramount in mitigating the risk of thrombosis in burn patients. Early and targeted antimicrobial therapy, wound debridement, and rigorous infection surveillance are crucial components of a comprehensive strategy. Additionally, close monitoring of coagulation parameters and the judicious use of anticoagulant therapy may be warranted in high-risk patients to prevent thrombotic complications.33-35
Another complication we recorded in 1 patient was AKI due to nephrotoxic drugs (prolonged administration of nonsteroidal anti-inflammatory dugs and antibiotics). According to previous studies, AKI in burn patients is categorized into early AKI, occurring in the first 3 days after the burn, or late AKI. Early AKI is primarily attributed to factors such as hypovolemia and hemodynamic alterations, diminished renal perfusion, burn-induced systemic inflammation, hemolysis, rhabdomyolysis, and denatured protein deposition. Conversely, late-onset AKI is frequently linked to complications such as sepsis, multiple organ failure, and the administration of nephrotoxic medications.36-38
Conclusions
The cases presented in this series highlight the complex and challenging management of patients with severe burns, particularly those resulting from domestic explosions involving LPG. Despite the significant morbidity associated with these injuries, our patients demonstrated favorable outcomes, underscoring the importance of prompt and comprehensive management strategies.
Inhalation injury, microbial infections, thromboembolic complications, and AKI were among the significant challenges encountered by our patients. Through aggressive treatment modalities, including bronchoscopy-guided therapy for inhalation injury, targeted antimicrobial therapy, and vigilant infection control measures, we were able to effectively address these complications.
Furthermore, our cases underscore the importance of risk stratification and vigilant monitoring for complications such as thromboembolism and nephrotoxicity, particularly in patients with extensive burn injuries. Early recognition and intervention can significantly mitigate the risk of adverse outcomes in this patient population.
Overall, the successful management of these cases emphasizes the importance of a multidisciplinary approach, close collaboration between specialties, and adherence to evidence-based guidelines in optimizing outcomes for patients with severe burns. Continued research and clinical innovation are warranted to further enhance the care of these complex patients and improve long-term outcomes.
Acknowledgments
Authors: Eliza-Maria Bordeanu-Diaconescu, MD¹,²; Andreea Grosu-Bularda, MD, PhD¹,²; Adrian Frunza, MD, PhD¹,²; Sabina Grama, MD, PhD²; Mihaela-Cristina Andrei, MD, PhD¹; Tiberiu-Paul Neagu, MD, PhD¹,²; Ioan Lascar, MD, PhD ¹; Cristian-Sorin Hariga, MD, PhD¹
Affiliations: ¹Department of Plastic Surgery and Reconstructive Microsurgery, Carol Davila University of Medicine and Pharmacy Bucharest, Romania; ²Burn Centre, Emergency Clinical Hospital of Bucharest, Romania
Correspondence: Andreea Grosu-Bularda; andreea.grosu-bularda@umfcd.ro
The authors express their gratitude to the personnel of the Burn Centre of the Bucharest Emergency Clinical Hospital for taking part in these patients' medical care.
Ethics: This study was approved on 29 January 2024 by the Hospital Ethics Committee of Bucharest Emergency Clinical Hospital (approval number 793). Informed consent was obtained from all subjects.
Disclosures: The authors disclose no conflict of interest, and the work was not supported or funded by any drug company.
References
1. Wang Y, Beekman J, Hew J, et al. Burn injury: Challenges and advances in burn wound healing, infection, pain and scarring. Adv Drug Deliv Rev. 2018;123:3-17. doi:10.1016/j.addr.2017.09.018
2. Jeschke MG, van Baar ME, Choudhry MA, Chung KK, Gibran NS, Logsetty S. Burn injury. Nat Rev Dis Primers. 2020 Feb 13;6(1):11. doi:10.1038/s41572-020-0145-5
3. Datta PK, Roy Chowdhury S, Aravindan A, Saha S, Rapaka S. Medical and surgical care of critical burn patients: a comprehensive review of current evidence and practice. Cureus. 2022 Nov 15;14(11):e31550. doi:10.7759/cureus.31550
4. Norbury W, Herndon DN, Tanksley J, Jeschke MG, Finnerty CC. Infection in Burns. Surg Infect (Larchmt). 2016;17(2):250-255. doi:10.1089/sur.2013.134
5. Liang H, Wang T, Luo Z, Wang X, Kang X, Deng J. Risk assessment of liquefied petroleum gas explosion in a limited space. ACS Omega. 2021 Sep 13;6(38):24683-24692. doi:10.1021/acsomega.1c03430
6. Kostiuk M, Burns B. Trauma Assessment. In: StatPearls. StatPearls Publishing; 2023 Jan. https://www.ncbi.nlm.nih.gov/books/NBK555913/
7. Hussmann B, Lendemans S. Pre-hospital and early in-hospital management of severe injuries: changes and trends. Injury. 2014;45 Suppl 3:S39-S42. doi:10.1016/j.injury.2014.08.016
8. Baranwal S, Roy N, Chowdri A, Bhattacharya S. Etiological & clinical spectrum of liquefied petroleum gas (LPG) related burns: a three-year study from a tertiary care burn centre in New Delhi. Burns. 2022;48(6):1481-1487. doi:10.1016/j.burns.2021.07.020
9. Hassan Z, Wong JK, Bush J, Bayat A, Dunn KW. Assessing the severity of inhalation injuries in adults. Burns. 2010;36:212-216. doi:10.1016/j.burns.2009.06.205
10. Shubert J, Sharma S. Inhalation Injury. In: StatPearls. StatPearls Publishing; 2023 Jan. https://www.ncbi.nlm.nih.gov/books/NBK513261/
11. Dries DJ, Endorf FW. Inhalation injury: epidemiology, pathology, treatment strategies. Scand J Trauma Resusc Emerg Med. 2013;21:31.
12. Jonkam C, Zhu Y, Jacob S, et al. Muscarinic receptor antagonist therapy improves acute pulmonary dysfunction after smoke inhalation injury in sheep. Crit Care Med. 2010;38:2339-2344.
13. van der Poll T, Coyle SM, Barbosa K, Braxton CC, Lowry SF. Epinephrine inhibits tumor necrosis factor-alpha and potentiates interleukin 10 production during human endotoxemia. J Clin Invest. 1996;97(3):713-719. doi:10.1172/JCI118469
14. Suter PM, Domenighetti G, Schaller MD, Laverriere MC, Ritz R, Perret C. N-acetylcysteine enhances recovery from acute lung injury in man. A randomized, double-blind, placebo-controlled clinical study. Chest. 1994;105:190-194.
15. Struck MF. Infection control in burn patients: are fungal infections underestimated?. Scand J Trauma Resusc Emerg Med. 2009 Oct 9;17:51-56. doi:10.1186/1757-7241-17-51
16. Williams FN, Herndon DN, Hawkins HK, et al. The leading causes of death after burn injury in a single pediatric burn center. Crit Care. 2009;13(6):R183.
17. Norbury W, Herndon DN, Tanksley J, Jeschke MG, Finnerty CC. Infection in burns. Surg Infect (Larchmt). 2016;17(2):250-255. doi:10.1089/sur.2013.134
18. Franeschi D, Gerding RL, Phillips G, Fratianne RB. Risk factors associated with intravascular catheter infections in burned patients: a prospective, randomized study. J Trauma. 1989 Jun;29:811-815.
19. Gallagher JJ, Williams-Bouyer N, Villarreal C, et al. Treatment of infection in burns. In: Herndon DN, ed. Total Burn Care, 3rd ed. WB Saunders; 2007:136-176.
20. Hodea FV, Lazarescu AL, Grosu-Bularda AN, Cretu A, Teodoreanu RN, Lascar I, Hariga CS. Antimicrobial resistance of ESKAPE pathogens in major burns patients: One-year retrospective study. Farmacia. 2023;71:3.
21. Andrade FF, Silva D, Rodrigues A, Pina-Vaz C. Colistin update on its mechanism of action and resistance, present and future challenges. Microorganisms. 2020 Nov 2;8(11):1716. doi:10.3390/microorganisms8111716
22. Mariano F, Malvasio V, Risso D, et al. Colistin therapy, survival and renal replacement therapy in burn patients: a 10-year single-center cohort study. Int J Gen Med. 2022 May 25;15:5211-5221. doi:10.2147/IJGM.S357427
23. Horvath EE, Murray CK, Vaghan GM, et al. Fungal wound infection (not colonization) is independently associated with mortality in burn patients. Ann Surg. 2007;245:978-985.
24. Capoor MR, Sarabahi S, Tiwari VK, Narayanan RP. Fungal infections in burns: diagnosis and management. Indian J Plast Surg. 2010;43(Suppl):S37-S42. doi:10.4103/0970-0358.70718
25. Trofa D, Gácser A, Nosanchuk JD. Candida parapsilosis, an emerging fungal pathogen. Clin Microbiol Rev. 2008;21(4):606-625. doi:10.1128/CMR.00013-08
26. Clark TA, Slavinski SA, Morgan J, et al. Epidemiologic and molecular characterization of an outbreak of Candida parapsilosis bloodstream infections in a community hospital. J Clin Microbiol. 2004;42(10):4468-4472. doi:10.1128/JCM.42.10.4468-4472.2004
27. Almirante B, Rodriguez D, Cuenca-Estrella M, et al. Epidemiology, risk factors, and prognosis of Candida parapsilosis bloodstream infections: case-control population-based surveillance study of patients in Barcelona, Spain, from 2002 to 2003. J Clin Microbiol. 2006;44:1681-1685.
28. Chen CY, Sheng WH, Huang SY, et al. Clinical characteristics and treatment outcomes of patients with candidaemia due to Candida parapsilosis sensu lato species at a medical centre in Taiwan, 2000–12. J Antimicrob Chemother. 2015;70:1531-1538.
29. Barchiesi F, Orsetti E, Osimani P, Catassi C, Santelli F, Manso E. Factors related to outcome of bloodstream infections due to Candida parapsilosis complex. BMC Infect Dis. 2016 Aug 9;16:387. doi:10.1186/s12879-016-1704-y
30. Verdaguer V, Walsh TJ, Hope W, Cortez KJ. Galactomannan antigen detection in the diagnosis of invasive aspergillosis. Expert Rev Mol Diagn. 2007;7(1):21-32. doi:10.1586/14737159.7.1.21
31. Eigl S, Hoenigl M, Spiess B, et al. Galactomannan testing and aspergillus PCR in same-day bronchoalveolar lavage and blood samples for diagnosis of invasive aspergillosis. Med Mycol. 2017;55(5):528-534. doi:10.1093/mmy/myw102
32. Harrington DT, Mozingo DW, Cancio L, Bird P, Jordan B, Goodwin CW. Thermally injured patients are at significant risk for thromboembolic complications. J Trauma. 2001;50(3):495-499. doi:10.1097/00005373-200103000-00014
33. Ahuja RB, Bansal P, Pradhan GS, Subberwal M. An analysis of deep vein thrombosis in burn patients (part II): A randomized and controlled study of thrombo-prophylaxis with low molecular weight heparin. Burns. 2016;42(8):1693-1698. doi:10.1016/j.burns.2016.08.007
34. Bordeanu-Diaconescu EM, Grosu-Bularda A, Frunza A, Grama S, Andrei MC, Neagu TP, Hariga CS, Lascar I. Venous Thromboembolism in Burn Patients: A 5-Year Retrospective Study. Medicina (Kaunas). 2024 Feb 2;60(2):258. doi: 10.3390/medicina60020258. PMID: 38399545; PMCID: PMC10889946.
35. Coban YK. Infection control in severely burned patients. World J Crit Care Med. 2012 Aug 4;1(4):94-101. doi:10.5492/wjccm.v1.i4.94
36. Wu G, Xiao Y, Wang C, et al. Risk factors for acute kidney injury in patients with burn injury. J Burn Care Res. 2017;38(5):271-282. doi:10.1097/bcr.0000000000000438
37. Legrand M, Clark AT, Neyra JA, Ostermann M. Acute kidney injury in patients with burns. Nat Rev Nephrol. 2024;20(3):188-200. doi:10.1038/s41581-023-00769-y
38. Putra ON, Saputro ID, Diana D. Rifle criteria for acute kidney injury in burn patients: prevalence and risk factors. Ann Burns Fire Disasters. 2021 Sep 30;34(3):252-258.