Use of an Autologous Heterogenous Skin Construct in the Treatment of Intractable Late-Effect Radiation Wounds: Case Series
Abstract
Background. Late-effect radiation–induced wounds represent a particularly difficult category of wounds to manage and treat. Fibrosis, impaired cellular activity, ischemia, and wound chronicity all work to impair healing, and this becomes more pronounced when defects are large or when avascular structures such as bone are exposed. Effective treatment options for this type of wound are limited. Thorough excision of irradiated tissue followed by distal pedicled or free flap closure is the most successful; however, this often requires multiple-stage surgeries and prolonged hospitalization and is associated with significant donor site morbidity. This is complicated further when wounds are large or in difficult locations, when surgery is not appropriate, or when there is limited access to surgeons with the appropriate experience/skill to perform such procedures.
Methods.This case series describes the use of an autologous heterogenous skin construct (AHSC) made from a small full-thickness sample of the patient’s healthy skin. Three patients with intractable late-effect radiation wounds were treated with AHSC. Case 1 describes an abdominal wound with tunneling of 7.5 cm to the pubic symphysis, which had been treated for known osteomyelitis, and a shallower full-thickness groin wound. Case 2 describes a right scapular wound with exposed bone, which had failed flap closure. Case 3 describes a right thigh wound in a patient who had been treated for sarcoma with extensive radiation therapy. This eventually resulted in an above-the-knee amputation, which failed to heal, and full exposure of the distal end of the resected femur. All wounds had been present for greater than 10 months.
Results. Mean percent volume reduction was 83% (±2.7) at 3 weeks and 92.9% (±4.7) at 4 weeks. The tunneled abdominal wound decreased in depth from 7.5 cm to 1.2 cm in 3 weeks. Complete closure was achieved at 11 weeks for the abdominal and groin wounds (patient 1) and at 16 weeks for the thigh wound (patient 3). The scapular wound volume of patient 2 had decreased by 91.8% at week 4 but was not fully restored until week 21. Mean time to closure was 16.1 (±4.7) weeks.
Conclusions. AHSC was effective in covering exposed bone, improving wound bed vascularity, filling in significant wound depth, and achieving complete wound closure with one application in patients with intractable late-effect radiation wounds.
Introduction
Late-effect radiation–induced wounds represent a particularly difficult category of wounds to manage and treat. Approximately 7 million patients are treated with radiotherapy worldwide each year,1 and the number of radiation-treated survivors in the US is projected to be over 4 million by 2030.2 Complications occur in 50% to 60%, with up to 25% of those treated experiencing significant skin fibrosis or ulceration.1,3,4 Radiotherapy effects on tissue are complex and enduring. The pathophysiology of radiation skin damage can generally be divided into the direct effects of ionizing radiation on the cells and the body’s immune response to insult, which result in unregulated inflammation, oxidative stress and loss, or molecular damage to skin regenerative and reparative cells.
Radiation affects the ability of cells to replicate and migrate and can cause cell death (apoptosis).5 As ionizing radiation passes through the cells, it reacts with water and other cellular molecules to produce reactive oxygen species (ROS).4 ROS interact with cellular components, causing intracellular and molecular damage, particularly to cellular DNA.5,6 This is especially harmful to vessel and skin stem cell and progenitor populations, which lose their ability reproduce, differentiate, and repair damaged tissue.7
Secondarily, radiation damage triggers a highly amplified immune response, initiating a cascade of proinflammatory mediators, which escalate and perpetuate the inflammatory response for prolonged periods of time. A persistent inflammatory environment, along with direct cellular damage to regenerative and reparative cells, interferes with and alters tissue repair processes.7-9 Profibrotic mediators remain elevated in fibroblasts, endothelial cells, and keratinocytes.6 Angiogenic activity is severely inhibited; larger vessel walls fibrose, thicken, and narrow; and small vessels become completely occluded (obliterative endarteritis), resulting in ischemia and tissue hypoxia. Lymphatics are destroyed or become blocked by fibrous tissue, resulting in edema, which further decreases local perfusion and perpetuates the inflammatory response.3,6,7,9 The dermis becomes hypovascular, thickened, and inelastic, often without hair follicles and sebaceous glands.6,10 Atypical fibroblasts replace subcutaneous tissue with an overproduction of thickened, unorganized extracellular matrix.4,10 The epidermis becomes atrophied and hypovascular without the normal interlocking architecture of the dermal-epidermal junction, making it fragile and painful.3
In late-effect radiation wounds, fibrosis, impaired cellular activity, ischemia, and wound chronicity all work to impair healing and become more pronounced when avascular structures such as bone and tendon are exposed.5 Effective treatment options for this type of wound are limited.5,10 Thorough excision of irradiated tissue followed by distal pedicled or free flap closure is the most successful; however, this often requires multiple-stage surgeries and prolonged hospitalization and is associated with high complication rates and significant donor site morbidity.11 This is complicated further when defects are large or in difficult locations, when surgery is not appropriate, or when there is limited access to surgeons with the appropriate experience/skill to perform such procedures. There is urgent need for alternatives that are less technically complex, less invasive, and have lower associated morbidity.
This case series describes the use of an autologous heterogenous skin construct (AHSC) (SkinTE,PolarityTE, MD, Inc), an autograft made from a small full-thickness sample of the patient’s healthy skin. Three patients with intractable, late-effect radiation wounds, present for greater than 10 months, were treated with AHSC.
Methods
Data were collected retrospectively via chart review. Institutional review board (IRB) approval (IRB 1735372-2) was obtained for this retrospective cohort study, which meets the waiver criteria as described in the 45 Code of Federal Regulations (CFR) 164.512 (i) (2) (ii). Mean percent volume reduction was calculated from measurements within the same week but may be up to 4 days different in time since AHSC application.

Treatment Description
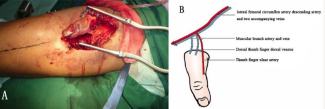
For each patient, a small ellipse of full-thickness skin was harvested from an area of healthy skin, typically the abdomen, and the donor site was closed primarily. Donor skin was sent to the manufacturer for processing, and the AHSC was returned for application within 3 days. All surfaces of the wound bed were debrided, removing all chronic or nonviable tissue and wound debris. In the case of the tunneled abdominal wound, endoscopic instruments were used for visualization and to ensure adequate debridement (Figure 1). All surfaces of the wounds were coated with AHSC. A fenestrated silicone sheet was applied to protect the graft and negative pressure wound therapy (NPWT) was applied over this( Figure 2). For the deep abdominal and thigh wounds, NPWT was only applied to the outer portion of the wound, allowing fluid egress and facilitating approximation of deeper tissues (similar to an incisional NPWT dressing). Strips of hydrocolloid wafer were used around wound edges to ensure a good seal and protect peri-wound skin. NPWT was set at 125 mm Hg, continuous, and changed weekly. Bordered foam dressings were used once wound volume was restored. Dressings were changed weekly and as needed.

Results
Patient Description
Patient 1 was a 73-year-old female who developed malignant melanoma of the vulva 27 years prior, which was treated with excision and radiation. She had recurrent, draining wounds in the radiated tissue since that time. She presented with a nonhealing hysterectomy surgical incision and a left groin ulcer, both within irradiated tissue. The abdominal wound tracked 7.5 cm to the posterior aspect of the pubic symphysis, which had been treated for recurrent osteomyelitis and had been present for 4.5 months.
Patient 2 was a 60-year-old female with a history of squamous cell cancer that was treated with wide excision, radiation, and chemotherapy. Local tissue rearrangement was attempted to cover the deficit, but this failed to heal for greater than 1 year. During this time, she was treated for osteomyelitis of the exposed bone. Additional prior treatments included hyperbaric therapy (HBO), multiple types of cellular and tissue products, and split-thickness skin grafting.
Patient 3 was a 73-year-old-male with history of sarcoma of the thigh, treated with wide excision and radiation. His total knee prosthesis became infected, eventually leading to an above-the-knee amputation. The radiated tissue failed to heal for over 1 year despite HBO treatment. He developed a seroma around the distal half of the resected femur, which had to be surgically opened and debrided, leaving the entire distal end of the resected femur exposed. Plastic surgery offered hip disarticulation with local tissue rearrangement to achieve closure; however, this would have prevented or significantly limited the possibility of future ambulation with a prosthesis.


Outcomes
Outcomes can be seen in Table 1. Mean percent volume reduction was 83% (±2.7) at 3 weeks and 92.9% (±4.7) at 4 weeks. The tunneled abdominal wound decreased in depth from 7.5 cm to 1.2 cm in 3 weeks. Complete closure was achieved at 11 weeks for the abdominal and groin wounds (patient 1) and at 16 weeks for the thigh wound (patient 3). The scapular wound volume of patient 2 had decreased by 91.8% at week 4 but was not fully restored until week 21. Mean time to closure was 16.1 (±4.7) weeks. Mean percent volume reduction can be seen in Figure 3. Wound progressions can be seen in Figures 4-7.

Discussion
Outside of tissue rearrangement, few treatments exist that can restore large volume defects in a timely manner. NPWT is often used to stimulate granulation tissue formation and decrease wound volume, but its use in radiation wounds is problematic due to fragility of the peri-wound skin. In addition, results are prolonged and leave already immunocompromised tissue at higher risk for infection. Partial and full-thickness skin grafts have exceedingly low success rates due to the poor vascularity of radiated tissue and are not able to restore volume in deep wounds.11 In recent years, modulation of cytokines, use of exomes, and introduction of healthy fibroblasts and keratinocytes into the wound bed have all been studied, exhibiting varying degrees of success.7,12 Some of the most promising results have been seen with the use of stem and progenitor cells.13-15 Mesenchymal stem cells (MSC), in particular, have been shown to replace damaged or destroyed cells through differentiation, decrease inflammation and oxidative stress, modulate the immune response, and promote revascularization; however, much of this research is still in the animal model and preliminary clinical stages.16,17



Healthy full-thickness skin contains a family of stem cells that collectively maintain homeostasis in all layers and structures of skin. As cells age and die, new cells are produced, which can differentiate and replace lost cells. With skin injury, regenerative cells work to replace damaged tissue, rather than just maintaining homeostasis. The manufacture of AHSC preserves and activates the skin’s endogenous regenerative and supportive cell populations, upregulating the extracellular matrix and stem cell gene expression pathways associated with native wound healing.18 It also optimizes surface-to-volume ratio, allowing better survival and take of cell aggregates within the wound bed. When applied, they interact with the wound environment and begin to carry out their normal functions of tissue repair, which include but are not limited to, modulation of inflammation, promotion of angiogenesis and proliferation, and differentiation to replace missing skin architecture and structures.19-21 This is similar to some of the described actions of MSCs; however, skin stem cells are much more specialized in their ability to regenerate and repair skin because, in complex interaction with one another, they are fulfilling their specific, intended biological function and can, therefore, do it more efficiently and efficaciously.

In this cohort, a marked improvement in the vascularity of the wound bed and growth of new vascular tissue was visualized within the first week after AHSC application. This was surprising in such chronic, radiated tissue and is suggestive of 1) effective graft survival and take, 2) transition of the wounds from an inflammatory to a proliferative state, and 3) improvement of the impaired angiogenic activity seen in radiation fibrosis. The 83% mean reduction in wound volume by week 3 further supports this and is particularly remarkable in the tunneled abdominal wound of patient 1. Tunneling wounds are difficult to heal in nonirradiated tissue, often requiring surgical unroofing or widening of the superficial aspect of the wound to prevent abscess formation and allow healing from the inside out. In a tunneled wound with significant radiation fibrosis and exposed bone at the base, the likelihood of achieving wound closure is poor at best. In this case, the tunnel depth decreased by over 6 cm in 3 weeks and the wound was completely closed at week 11. Of note, patient 1 returned to the wound center 2 years after AHSC application due to a flair of vulvar inflammation and a new groin wound. The areas that had been treated with AHSC were completely free of inflammation, while the surrounding untreated tissue was significantly inflamed (Figure 8). In the scapular wound (patient 2), tissue rearrangement, split-thickness skin grafts, and multiple advanced tissue products had all failed prior to AHSC. Pressure and shear forces, due to location of the wound over a scapular bony prominence, and impaired sensation, related to previous surgeries, likely contributed to this. New areas of bruising over peri-wound bony prominences, in conjunction with fluctuations in wound size, would suggest that mechanical trauma continued to be a factor after AHSC application. Despite this, the wound bed appeared significantly more vascular within a week of AHSC application. At 4 weeks, there was epithelial island formation within the wound bed, indicative of full-thickness skin regeneration, and it had decreased in size by 92%. In the thigh wound of patient 3, deep wound tissues, approximated by NPWT, knitted together, decreasing the amount of tissue necessary to restore wound volume. This is a remarkable response in irradiated tissue, only possible through a marked improvement it wound bed vascularity. By week 4, the wound depth had decreased from 5 cm to 3 mm. Complete wound closure was slowed by persistent edema due to the patient’s inconsistency with wearing his residual limb shrinker, but it was achieved by week 14. The patient, formerly wheelchair dependent, walked into a follow up visit at week 20 wearing his new above-the-knee prosthesis (Figure 9).

Limitations
This was a limited case series of only 3 patients, with limited follow up. While results were promising in this extremely challenging wound etiology, further prospective trials are needed to fully elucidate efficacy and best practice for the use of AHSC in late-effect radiation wounds.
Conclusions
While this case series represents a small sample size, the effectiveness of AHSC in decreasing inflammation, facilitating angiogenesis, and normalizing dysregulated tissue repair was dramatic and well exceeded the efficacy of advanced therapies previously utilized in this group. AHSC was effective in covering exposed bone, restoring significant wound depth, and achieving wound closure with one application in 3 patients with intractable late-effect radiation wounds.
Acknowledgments
The authors would like to thank James Mayo, MD, and Deborah Tedesco, DNP, APRN, ANP-BC, CBCN, AP-PMN, CWS, CWCN-AP, CPHQ, who participated significantly in the care of one of the patients.
Affiliations: 1Lakeland Regional Health, Lakeland, Florida; 2Orlando Regional Medical Center, Orlando, Florida; 3PolarityTE, MD, Inc, Salt Lake City, Utah
Correspondence: Diana Burgueño-Vega, MD; diana.burgueno-vega@mylrh.org
During the study period, AHSC technology was registered with the US Food and Drug Administration (FDA) as a human cell, tissue, and cellular and tissue-based product (HCT/P), regulated solely under Section 361 of the Public Health Service Act. It is now being studied as an investigational new drug for the treatment of chronic cutaneous ulcers and is currently available for investigational use only.
Data Access Statement: Institutional review board (IRB) approval (IRB 1731663-1) was obtained for this retrospective study, which meets the waiver criteria as described in the 45 Code of Federal Regulations (CFR) 164.512 (i) (2) (ii). Research data supporting this publication are available upon request of the corresponding author.
Disclosures: MB is a former employee of PolarityTE. DB, DS, and WC have no conflicts of interest to declare.
References
1. Majeed H, Gupta V. Adverse Effects Of Radiation Therapy. StatPearls. Published online 2022. Accessed March 28, 2022. https://pubmed.ncbi.nlm.nih.gov/33085406/
2. Bryant AK, Banegas MP, Martinez ME, Mell LK, Murphy JD. Trends in Radiation Therapy among Cancer Survivors in the United States, 2000–2030. Cancer Epidemiology, Biomarkers & Prevention. 2017;26(6):963-970. doi:10.1158/1055-9965.EPI-16-1023
3. DiCarlo AL, Bandremer AC, Hollingsworth BA, et al. Cutaneous Radiation Injuries: Models, Assessment and Treatments. Radiat Res. 2020;194(3):315. doi:10.1667/RADE-20-00120.1
4. Devalia HL, Mansfield L. Radiotherapy and wound healing. Int Wound J. 2008;5(1):40-44. doi:10.1111/J.1742-481X.2007.00351.X
5. Dormand EL, Banwell PE, Goodacre TEE. Radiotherapy and wound healing. Int Wound J. 2005;2(2):112-127. doi:10.1111/J.1742-4801.2005.00079.X
6. Olascoaga A, Vilar-Compte D, Poitevin-Chacón A, Contreras-Ruiz J. Wound healing in radiated skin: Pathophysiology and treatment options. Int Wound J. 2008;5(2):246-257. doi:10.1111/J.1742-481X.2008.00436.X
7. Yang X, Ren H, Guo X, Hu C, Fu J. Radiation-induced skin injury: pathogenesis, treatment, and management. Aging. Published online November 16, 2020. doi:10.18632/aging.103932
8. Kim JH, Kolozsvary AJJ, Jenrow KA, Brown SL. Mechanisms of radiation-induced skin injury and implications for future clinical trials. Int J Radiat Biol. 2013;89(5):311-318. doi:10.3109/09553002.2013.765055
9. Borrelli MR, Shen AH, Lee GK, Momeni A, Longaker MT, Wan DC. Radiation-Induced Skin Fibrosis. Ann Plast Surg. 2019;83(4S):S59-S64. doi:10.1097/SAP.0000000000002098
10. Haubner F, Ohmann E, Pohl F, Strutz J, Gassner HG. Wound healing after radiation therapy: Review of the literature. Radiation Oncology. 2012;7(1):162. doi:10.1186/1748-717X-7-162
11. Fujioka M. Surgical Reconstruction of Radiation Injuries. Adv Wound Care (New Rochelle). 2014;3(1):25-37. doi:10.1089/wound.2012.0405
12. Kim JH, Jenrow KA, Brown SL. Mechanisms of radiation-induced normal tissue toxicity and implications for future clinical trials. Radiat Oncol J. 2014;32(3):103-115. doi:10.3857/roj.2014.32.3.103
13. Rodgers K, Jadhav SS. The application of mesenchymal stem cells to treat thermal and radiation burns. Adv Drug Deliv Rev. 2018;123:75-81. doi:10.1016/j.addr.2017.10.003
14. Straub JM, New J, Hamilton CD, Lominska C, Shnayder Y, Thomas SM. Radiation-induced fibrosis: mechanisms and implications for therapy HHS Public Access. J Cancer Res Clin Oncol. 2015;141(11):1985-1994. doi:10.1007/s00432-015-1974-6
15. Ryu JS, Jeong EJ, Kim JY, et al. Application of mesenchymal stem cells in inflammatory and fibrotic diseases. Int J Mol Sci. 2020;21(21):1-26. doi:10.3390/ijms21218366
16. Fang Z, Chen P, Tang S, et al. Will mesenchymal stem cells be future directions for treating radiation-induced skin injury? Stem Cell Res Ther. 2021;12(1):179. doi:10.1186/s13287-021-02261-5
17. Kiang JG. ADULT MESENCHYMAL STEM CELLS AND RADIATION INJURY. Health Phys. 2016;111(2):198. doi:10.1097/HP.0000000000000459
18. Sopko N, Milner S, Mathis R, et al. Neogenesis of Full-thickness Skin and Concomitant Dermal Appendages in Acute Wounds Using Novel Autologous Homologous Skin Construct Therapy in Preclinical and Clinical Settings. Symposium on Advanced Wound Care. Published online May 8, 2019. Accessed April 26, 2022. https://www.hmpgloballearningnetwork.com/site/woundcare/poster/neogenesis-full-thickness-skin-and-concomitant-dermal-appendages-acute-wounds-using-novel
19. Mundinger GS, Mundinger GS, Armstrong DG, et al. Autologous Homologous Skin Constructs Allow Safe Closure of Wounds: A Retrospective, Noncontrolled, Multicentered Case Series. Plast Reconstr Surg Glob Open. Published online 2020. doi:10.1097/GOX.0000000000002840
20. Granick MS, Baetz NW, Labroo P, Milner S, Li WW, Sopko NA. In vivo expansion and regeneration of full‐thickness functional skin with an autologous homologous skin construct: Clinical proof of concept for chronic wound healing. Int Wound J. 2019;16(3):841-846. doi:10.1111/iwj.13109
21. Isbester K, Wee C, Boas S, Sopko N, Kumar A. Regeneration of Functional, Full-Thickness Skin With Minimal Donor Site Contribution Using Autologous Homologous Skin Construct. Plastic Surgery Case Studies. 2020;6:2513826X1989881. doi:10.1177/2513826x19898810
References
1. Majeed H, Gupta V. Adverse Effects Of Radiation Therapy. StatPearls. Published online 2022. Accessed March 28, 2022. https://pubmed.ncbi.nlm.nih.gov/33085406/
2. Bryant AK, Banegas MP, Martinez ME, Mell LK, Murphy JD. Trends in radiation rherapy among cancer survivors in the United States, 2000–2030. Cancer Epidemiol Biomarkers Prev. 2017;26(6):963-970. doi:10.1158/1055-9965.EPI-16-1023
3. DiCarlo AL, Bandremer AC, Hollingsworth BA, et al. Cutaneous radiation injuries: models, assessment and treatments. Radiat Res. 2020;194(3):315. doi:10.1667/RADE-20-00120.1
4. Devalia HL, Mansfield L. Radiotherapy and wound healing. Int Wound J. 2008;5(1):40-44. doi:10.1111/J.1742-481X.2007.00351.X
5. Dormand EL, Banwell PE, Goodacre TEE. Radiotherapy and wound healing. Int Wound J. 2005;2(2):112-127. doi:10.1111/J.1742-4801.2005.00079.X
6. Olascoaga A, Vilar-Compte D, Poitevin-Chacón A, Contreras-Ruiz J. Wound healing in radiated skin: Pathophysiology and treatment options. Int Wound J. 2008;5(2):246-257. doi:10.1111/J.1742-481X.2008.00436.X
7. Yang X, Ren H, Guo X, Hu C, Fu J. Radiation-induced skin injury: pathogenesis, treatment, and management. Aging. Published online November 16, 2020. doi:10.18632/aging.103932
8. Kim JH, Kolozsvary AJJ, Jenrow KA, Brown SL. Mechanisms of radiation-induced skin injury and implications for future clinical trials. Int J Radiat Biol. 2013;89(5):311-318. doi:10.3109/09553002.2013.765055
9. Borrelli MR, Shen AH, Lee GK, Momeni A, Longaker MT, Wan DC. Radiation-induced skin fibrosis. Ann Plast Surg. 2019;83(4S):S59-S64. doi:10.1097/SAP.0000000000002098
10. Haubner F, Ohmann E, Pohl F, Strutz J, Gassner HG. Wound healing after radiation therapy: Review of the literature. Radiation Oncology. 2012;7(1):162. doi:10.1186/1748-717X-7-162
11. Fujioka M. Surgical Reconstruction of radiation injuries. Adv Wound Care (New Rochelle). 2014;3(1):25-37. doi:10.1089/wound.2012.0405
12. Kim JH, Jenrow KA, Brown SL. Mechanisms of radiation-induced normal tissue toxicity and implications for future clinical trials. Radiat Oncol J. 2014;32(3):103-115. doi:10.3857/roj.2014.32.3.103
13. Rodgers K, Jadhav SS. The application of mesenchymal stem cells to treat thermal and radiation burns. Adv Drug Deliv Rev. 2018;123:75-81. doi:10.1016/j.addr.2017.10.003
14. Straub JM, New J, Hamilton CD, Lominska C, Shnayder Y, Thomas SM. Radiation-induced fibrosis: mechanisms and implications for therapy HHS Public Access. J Cancer Res Clin Oncol. 2015;141(11):1985-1994. doi:10.1007/s00432-015-1974-6
15. Ryu JS, Jeong EJ, Kim JY, et al. Application of mesenchymal stem cells in inflammatory and fibrotic diseases. Int J Mol Sci. 2020;21(21):1-26. doi:10.3390/ijms21218366
16. Fang Z, Chen P, Tang S, et al. Will mesenchymal stem cells be future directions for treating radiation-induced skin injury? Stem Cell Res Ther. 2021;12(1):179. doi:10.1186/s13287-021-02261-5
17. Kiang JG. Adult mesenchymal stem cells and radiation injury. Health Phys. 2016;111(2):198. doi:10.1097/HP.0000000000000459
18. Sopko N, Milner S, Mathis R, et al. Neogenesis of full-thickness skin and concomitant dermal appendages in acute wounds using novel autologous homologous skin construct therapy in preclinical and clinical settings. Symposium on Advanced Wound Care. Published online May 8, 2019. Accessed April 26, 2022. https://www.hmpgloballearningnetwork.com/site/woundcare/poster/neogenesis-full-thickness-skin-and-concomitant-dermal-appendages-acute-wounds-using-novel
19. Mundinger GS, Mundinger GS, Armstrong DG, et al. Autologous homologous skin constructs allow safe closure of wounds: a retrospective, noncontrolled, multicentered case series. Plast Reconstr Surg Glob Open. Published online 2020. doi:10.1097/GOX.0000000000002840
20. Granick MS, Baetz NW, Labroo P, Milner S, Li WW, Sopko NA. In vivo expansion and regeneration of full‐thickness functional skin with an autologous homologous skin construct: Clinical proof of concept for chronic wound healing. Int Wound J. 2019;16(3):841-846. doi:10.1111/iwj.13109
21. Isbester K, Wee C, Boas S, Sopko N, Kumar A. Regeneration of functional, full-thickness skin with minimal donor site contribution using autologous homologous skin construct. Plast Surg Case Stud. 2020;6:2513826X1989881. doi:10.1177/2513826x19898810