One-stage Flexor Reconstruction With Anterolateral Thigh and Fascia Lata Rolls After High-Voltage Trauma: A Case Report
Abstract
Background. Electrical injuries from high-voltage power lines are unique forms of trauma that can create challenging wounds for reconstructive surgeons. Our patients, a man in his late thirties (Patient 1) and a man in his early twenties (Patient 2), both sustained upper extremity injuries after contact with a high-voltage line.
Methods. Despite minimal superficial damage, both patients required fasciotomies and debridement of the volar forearm, revealing segmental defects in most digital tendons as well as the distal median nerve. Free fasciocutaneous anterolateral thigh (ALT) flaps were harvested to ensure adequate wound coverage. Additionally, fascia lata grafts were taken from the free flap donor site and rolled into tubes to transfer available flexor digitorum superficialis proximal tendon stumps to the distal stumps of flexor digitorum profundus. The rolls were also used to bridge segmental tendon defects in flexor pollicis longus, while cadaveric nerve allografts were used to bridge the median nerve defects.
Results. Nine months postoperatively, Patient 1 had premorbid function with activities of daily living (ADLs), and Patient 2 required only minimal assistance with instrumental ADLs. Within a year following reconstruction, Patient 1 mostly regained range of motion in his digits with some rigidity, and Patient 2 regained full range of motion in his digits with minimal rigidity.
Conclusions. These cases have demonstrated that the use of an ALT free flap combined with rolled fascia lata graft tubes may be an effective choice for reconstruction and functional restoration in cases of severe high-voltage electrical trauma.
Introduction
High-voltage electrical injuries are rare cases of trauma that result in a unique and challenging spectrum of sequelae. As these injuries often result from accidental contact with high-voltage lines, the upper extremities are almost always involved.1 Since the electrical current preferentially travels through deep tissues, patients primarily sustain damage to deeper structures that are usually untouched by thermal burns.1 In cases where digits can be spared, repair of large, segmental defects in the flexor tendons of the hand is often necessary. Harvesting a flap (typically groin or anterolateral thigh) for coverage following high-voltage injuries makes it desirable to source a tendon graft from the same donor area. This would minimize the number of surgical sites, reduce recovery and rehabilitation time, and decrease potential complications.
In this report, we describe the cases of 2 patients treated from 2018 to 2021 with similar severe unilateral disruption of the contents of the carpal tunnel as sequelae of high-voltage electrical injury. Tendons of the flexor digitorum profundus (FDP) and superficialis (FDS) were reconstructed using a modified technique of transferring proximal FDS to distal FDP with fascia lata grafts following dissection of an anterolateral thigh flap. To the authors’ knowledge, flexor repair with the fascia lata in high-voltage injury has not been previously described in the literature. Furthermore, the fascia lata is not a commonly used graft for bridging flexor tendon defects,2-4 and its usage in this context has not been greatly explored.
Methods
The first patient, a linesman in his late thirties, stumbled and accidentally placed his hand on a high-voltage line, suffering severe unilateral injury to his upper extremity. The second patient was a male in his early twenties who came into contact with a high-voltage line while climbing a utility pole. On examination, both patients presented with total loss of digital flexion and total distal median nerve paresis. There was minimal superficial damage. However, they suffered considerable damage to deeper soft tissue, which required fasciotomy and substantial debridement of the volar forearm. After debridement, both patients were left with approximately 7-cm segmental defects in the flexor digitorum tendons and flexor pollicis longus (FPL) tendons. Proximal attachments of FDP tendons to the muscle belly were also lost. Patient 1 had lost continuity in the tendons of all but the fifth digit, whereas Patient 2 had segmental defects in all digits. Damage to the patients’ median nerves had also left an approximately 5 cm discontinuity just proximal to the thenar eminence. No digital amputation was required during debridement, and defects were left open. Following several subsequent debridements and negative pressure wound therapy, the patients underwent definitive repair of their volar forearms approximately 1 month after initial presentation.
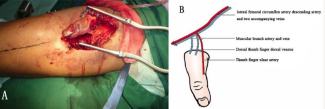
To achieve coverage of the volar forearm defects, a free fasciocutaneous anterolateral thigh flap (ALT) with perforators from the descending branch of the lateral circumflex femoral artery (DLCFA) and accompanying vein were harvested in both patients. Full-thickness fascia lata grafts were taken from the ALT donor site and were rolled into several tubes long enough to bridge the segmental defects. The rolls were secured via a longitudinal simple, absorbable running suture. A standard Pulvertaft distal-to-proximal tendon weave was then used to achieve continuity between the distal FDP tendon stumps and the grafts. As the tendons at the muscle belly of FDP were lost, available FDS tendon stumps at the muscle belly were transferred to the distal FDP tendons using the grafts. There was insufficient proximal FDS tendon for another tendon weave, so grafts were secured proximally via figure-of-eight suture (Figure 1). FPL defects were bridged directly. In both cases, a commercial processed cadaveric nerve allograft (Axogen, Alachua, FL) was used to bridge the defect in the median nerve. The fasciocutaneous portion of the ALT flap was then used to cover the superficial tissue defects. Patient 1 required a 13 × 25-cm flap for coverage, and Patient 2 required a 9 × 7-cm flap. The graft DLCFA was perfused by end-to-side anastomosis to the ulnar artery in Patient 1 and the radial artery in Patient 2. The accompanying vein underwent end-to-side anastomosis to the cephalic vein. Both patients underwent split-thickness skin grafting for coverage of other electrocution-related cutaneous burns.

Results
Both ALT flaps survived excellently. There were no postoperative complications in either patient, and the donor sites healed adequately without evidence of vastus lateralis instability. Repaired tendons were noted to be stable under passive range of motion 3 days postoperatively. A modified Duran program for flexor tendon repairwas used to facilitate healing and reduce graft adhesions. A dorsal blocking orthosis was employed during recuperation and physical therapy. Five months after definitive repair, Patient 1 underwent flap debulking and tenolysis. Patient 2 underwent flap debulking 7 months after repair but did not require tenolysis.
By their last occupational therapy visits (about 9 months post-operative), Patient 1 had overall function in activities of daily living (ADLs) return to premorbidity levels. Patient 2 required only minimal assistance (<25%) with instrumental ADLs. Both patients were able to partially recover range of motion of the digits and grip strength. The patients could flex all digits at both the proximal and distal interphalangeal joints, and strength recovery was the greatest challenge in physical therapy. As a result of the distal median nerve palsy, patients did not fully regain range of motion of the thenar eminence and had challenges opposing the thumb. Motion was recovered better than sensation as the segmental nerve defects were distal to the innervation of the digital flexors in the forearm; both patients experienced some persistent loss of sensation in the volar surfaces of digits 1 to 4 and in the thenar eminence in the affected hand.
Patient 1 went on to regain much of the range of motion with his digits and was able to make a fist with some rigidity in movement (Figure 2). Patient 2 eventually achieved practically full range of motion of all digits and could make a fist with minimal rigidity (Figure 3). While strength, sensation, and function were not fully regained, both patients reported satisfaction with the functional and aesthetic outcomes of the procedure. Within a year of reconstruction, Patient 1 was able to return to his job as a linesman and had further improvement in his ability to make a fist and oppose his thumb following tendon graft plication and flap debulking approximately 18 months after reconstruction. Patient 2 can now use his hand in his daily life without major difficulty.


Discussion
In such complex traumatic cases as those resulting from high-voltage injury, multiple procedures and surgical sites are often required for debridement of the burned tissue, amputation or reconstruction of tendons, wound coverage, nerve repair, and management of postoperative complications. In these 2 cases, usage of an ALT flap with concomitant fascia lata graft harvesting allowed for single-stage reconstruction and coverage with only 1 donor site. The use of a decellularized cadaveric nerve graft also eliminated the need for creation of another surgical site and allowed patients to regain some median nerve functionality despite a large segmental defect.
In the literature, fascia lata grafts are generally not discussed as a mainstay treatment for the repair of hand flexor or extensor tendons.2-4 Fascia lata grafts are most often used as reinforcement in other soft tissue reconstruction procedures5-6 and have sometimes been used for tendon transfer in nerve palsy.7 Palmaris longus and plantaris are the most used free tendon grafts for autologous hand tendon reconstruction overall,2 and they have been well documented for use in tendon repair for high-voltage injuries.8 While using these tendons as grafts results in negligible losses in functionality for most patients, they are often not present in the general population.9 Length of free tendon for grafting may also be insufficient to bridge multiple segmental defects, and these nearby tendons may be unavailable for grafting or transfer in severe traumatic cases such as these. While cadaveric tendon was considered for these cases, they were not available at the time of reconstruction, and acquiring approval for these cadaveric grafts would have significantly delayed repair. Harvesting the fascia lata in concert with the necessary ALT flap avoided the creation of a separate donor site and allowed for the bridging of multiple larger tendon defects with minimal additional risk of morbidity.
A few similar procedures10 -11 have been described in the literature. For example, one case of extensor compartment degloving utilized strips of fascia lata in a chimeric ALT flap to bridge segmental tendon loss and displayed comparable functional outcomes.10 In our cases, fascia lata was rolled into tubes. While this requires larger grafts, we anticipated this would better achieve geometric homogeneity and improve the distribution of mechanical stress on the graft and suture.
For both patients, the outcomes were encouraging despite the severity of initial injury and the necessary degree of reconstruction. Combined with the outcomes of similar applications of fascia lata grafts, these results suggest promise in our reconstructive methodology as an alternative to amputation or silicone rod grafting in large high-voltage electrical injuries of the upper extremities.
Acknowledgments
Affiliations: Division of Plastic Surgery, Department of Surgery, McGovern Medical School at the University of Texas Health Science Center at Houston, Houston, TX
Correspondence: Daniel J Freet, MD; daniel.j.freet@uth.tmc.edu
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosures: No authors disclose no financial or nonfinancial conflicts of interest.
References
1. Lee DH, Desai MJ, Gauger EM. Electrical injuries of the hand and upper extremity. J Am Acad Orthop Surg. 2019;27(1):e1-e8. doi:10.5435/JAAOS-D-17-00833
2. Moore T, Anderson B, Seiler JG. Flexor tendon reconstruction. J Hand Surg Am. 2010;35(6):1025-1030. doi:10.1016/j.jhsa.2010.03.042
3. Wong R, Alam N, McGrouther AD, Wong JK. Tendon grafts: their natural history, biology and future development. J Hand Surg Eur Vol. 2015;40(7):669-681. doi:10.1177/1753193415595176
4. Griffin M, Hindocha S, Jordan D, Saleh M, Khan W. An overview of the management of flexor tendon injuries. Open Orthop J. 2012;6(1):28-35. doi:10.2174/1874325001206010028
5. Andreu-Sola V, Aguilera-Sáez J, Rivas-Nicolls D, Bosacoma Roura P, Barret JP. Functional reconstruction of acutely burnt achilles tendon with composite anterolateral thigh flap with fascia lata: a case report. Ann Burns Fire Disasters. 2017;30(4):309-312.
6. Fankhauser G, Klomp A, Smith A, Rececca A, Casey W 3rd. Use of the pedicled tensor fascia lata myocutaneous flap in the salvage of upper extremity high-voltage electrical injuries. J Burn Care Res. 2010;31(4):670-673. doi:10.1097/BCR.0b013e3181e4c6d7
7. Goubier J-N, Teboul F. Restoration of active fingers flexion with tensor fascia lata transfer in total brachial plexus palsy. Tech Hand Up Extrem Surg. 2009;13(1):1-3. doi:10.1097/bth.0b013e3181818832
8. Suma P, Rao RVK, Srikanth R, Patil M. Single-stage reconstruction of high-voltage electric burns sequelae of Volar forearm using nerve grafts, short tendon grafts and microvascular flap. Indian J Burns. 2017;25(1):52. doi:10.4103/0971-653x.217041
9. Jakubietz MG, Jakubietz DF, Gruenert JG, Zahn R, Meffert RH, Jakubietz RG. Adequacy of palmaris longus and plantaris tendons for tendon grafting. J Hand Surg Am. 2011;36(4):695-698. doi:10.1016/j.jhsa.2011.01.007
10. Suondoh MS, Sulaiman WA, Ismail WF, Saad AZ. One stage microsurgical reconstruction with chimeric flap for salvaging complex hand injuries. Arch Hand Microsurg. 2020;25(2):156-160. doi:10.12790/ahm.20.0007
11. Bhat AK, Acharya AM, Soni N. Reconstruction of attritional rupture of flexor tendons with fascia lata graft following distal radius fracture malunion. J Hand Surg Asian Pac Vol. 2016;21(03):410-413. doi:10.1142/s2424835516720176