Fluid Resuscitation of Severely Burned Children
© 2024 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of ePlasty or HMP Global, their employees, and affiliates.
Questions
1. What is the optimal composition of hydrating solutions used to resuscitate children following a burn?
2. How much fluid is necessary for optimal resuscitation in the first 24 hours?
3. Why does burn shock resuscitation fail?
4. What end points should be monitored during the initial period of fluid resuscitation?
Case Description
A 2-year-old girl weighing 12.3 kg and measuring 82 cm in height accidentally tipped a pan of hot oil over herself (Figure 1). She sustained mixed second- and third-degree burns to 37% of her body. Peripheral intravenous access was established through unburned skin in the right upper limb, with prompt initiation of fluid resuscitation to restore tissue perfusion, electrolytes, and protein; maintain normal hydration in all body fluid compartments; correct acid-base imbalance; and preserve organ function. The fluid requirements were calculated using the Shriners Burns Hospital-Galveston pediatric formula.

Figure 1. Appearance on admission to the burn unit.
Q1. What is the optimal composition of hydrating solutions used to resuscitate children following a burn?
Following a burn, the wound sequesters isotonic fluid. Correcting hypovolemia requires the replacement of sodium, as water alone lowers the osmolarity of extracellular fluid, potentially causing intracellular overhydration and water intoxication. Recommended formulas suggest replacement of 0.5 to 0.6 mEq sodium per kg/% total body surface area (%TBSA) burn.1 The optimal tonicity and the use of colloids remain controversial. Mildly hypotonic lactated Ringer solution (LRS) is commonly used for the first 24 hours (Table 1)2 to avoid hyperchloremic metabolic acidosis associated with large volumes of isotonic saline.

Table 1. Lactated Ringer solution (LRS) is a mildly hypotonic balanced salt solution that approximates the composition and pH of the extracellular fluid. In addition, the lactate is metabolized to bicarbonate by the liver, which can partially correct the lactic acidosis of burn shock. No free water is needed in the first 24 hours since the sodium concentration in LRS is 130 mEq/L, which furnishes 80 to 100 ml of free water per liter. Despite a pH of 5.1, LRS has little effect on blood pH even when given in large quantities.
Colloids, such as plasma and albumin, are more effective in restoring oncotic pressure and intravascular volume than crystalloids. However, concern exists regarding protein extravasation and the development of systemic and pulmonary edema.3 Nevertheless, the microvasculature retains protein 8 to 12 hours after a burn,4 supporting the practice of infusing 5% albumin in normal saline for patients with burns over 40% TBSA and for those with low serum albumin levels or poor response to crystalloid resuscitation. Fresh frozen plasma is usually reserved for correcting clotting abnormalities since it carries the risk of disease transmission and transfusion-related acute lung injury (TRALI). Non-protein colloids, such as Hetastarch and dextran, are avoided in children due to complications observed in adult trauma patients, such as impaired renal function, bleeding, and pruritis.5
Mildly hypertonic saline solutions (HS) with sodium concentrations of 205 to 310 mEq/L preserve plasma volume while curtailing overhydration by shifting water from the intracellular to the extracellular compartments. A meta-analysis of 10 published studies of 2% to 3% NaCl with control groups that included a total of 536 patients reported a one-third reduction in 24-hour volume requirements with sustained effects for 48 hours. However, caution is necessary to prevent serum sodium levels exceeding 160 mEq/l due to the risks of hypernatremia, including hyperosmolarity, cerebral hemorrhage, hyperosmolar coma, and renal failure.6
Q2. How much fluid is necessary for optimal resuscitation in the first 24 hours?
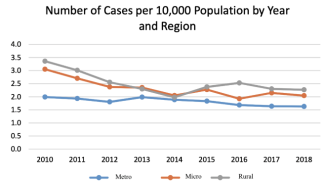
Intravenous fluid resuscitation is required for children with second- and third-degree burns exceeding 10% TBSA. Formulas have been proposed to estimate fluid requirements, recommending 2 to 4 mL/kg/% of salt-containing fluid to compensate for burn edema and achieve a urine output of 0.5 to 1.0 mL/kg/hour. The Modified Brooke and Parkland adult formulas prescribe 2 and 4 mL/kg/%TBSA burned of LRS, respectively, with half administered over the first 8 hours and the remainder over the next 16 hours.7However, children require approximately 6 mL/kg/%TBSA burned.8 Single-figure adult formulas may fail to consider maintenance and underestimate needs in small children and overhydrate large children (Figure 2).9 Accordingly, thePediatric Brooke formula recommends LRS at 3 mL/kg/%TBSA for the first day, with additional maintenance fluids using 5% dextrose in half normal saline based on weight (Table 2).

Figure 2. Fluid calculations for children of varying weights, comparing the Parkland and SBI Galveston formulas and maintenance requirements for the first 24 hours. (A) Represents a 20% TBSA burn. In the first 24 hours, a 1-year-old child weighing 9 kg with a 20% burn will be prescribed 720 mL by the Parkland formula and 1800 mL by the SBI Galveston formula, respectively. Since daily maintenance requirement is 900 mL, as determined by the Holliday-Segar formula, reliance on the Parkland alone in small children with small burns results in inadequate fluid resuscitation. (B) Represents an 80% TBSA burn. Large children with large burns may be over-resuscitated using the Parkland formula. TBSA has been calculated using the Mosteller formula with average height for weights for ages 1 to 12 years obtained from World Health Organization growth charts (https://www.cdc.gov/growthcharts/clinical_charts.htm).

Table 2. Holliday-Segar method for calculation of pediatric maintenance fluids based on weight.
Because burn edema and evaporative fluid losses bear a closer relationship to the extent of the burn rather than weight, the pediatric formula used by the Shriners Burns Hospital in Galveston is based on surface area calculations, derived from height/weight nomograms or formulas.10 It provides 5000 mL/m2TBSA burned for burn-related losses, plus 2000 mL/m2 TBSA for maintenance fluids in the initial 24-hour period. The amount is also given as half in the first 8 hours and the rest over 16 hours. Although no randomized trials have established the benefit of colloids, burn surgeons commonly use crystalloid solutions and supplement with albumin after 8 hours (Table 3). Infants require glucose monitoring and maintenance with 5% dextrose to prevent hypoglycemia resulting from depletion of glycogen stores. For children weighing over 40 kg, Warden suggested the use of HS containing LRS plus 50 mEq of sodium bicarbonate per liter (180 mEq Na for the first 8 hours post burn), initiated at a rate calculated by the Parkland formula. This offers the benefits of HS without complications.11

Table 3. Estimation of 24-hour requirements for the child in Figure 1 by the Galveston Shriners Burns Institute formula. The TBSA was estimated from the patient's height and weight using the Mosteller formula.
Q3. Why does burn shock resuscitation fail?
Inadequate hydration can lead to burn shock, renal failure, and death. This may occur due to delayed therapy, underestimation of burn size, miscalculated formulas, and higher fluid requirements in specific cases, such as high-voltage electrical injuries and inhalation injury. Accurate assessment of the TBSA% burned requires careful mapping of the burn on appropriate body proportion charts and exclusion of first-degree injuries. Estimates of burn size based solely on weight can be incorrect unless height and weight align with the 50th percentile.
Delayed or under-hydration is managed by providing additional fluid to expand the contracted intravascular volume, restore cardiovascular and renal hemodynamics, and correct acidosis. Conversely, caution should be exercised in compensating for excessive fluid intake as patients may already have developed significant edema fluid that is not accessible to the circulation.
Children are prone to “fluid creep,” a term that describes the insidious trend of infusing volumes larger than predicted by conventional formulas, particularly the Parkland formula. Recent studies have reported crystalloid fluid resuscitation volumes ranging from 4.8 to 6.7 mL/kg/%TBSA for the initial 24 hours post-burn.12 Excessive resuscitation promotes fluid extravasation into burned and unburned tissue that can result in massive facial and airway swelling requiring intubation, decreased chest wall compliance, pulmonary edema and congestive heart failure, burn wound conversion, cerebral edema (Figure 3), anterior ischemic optic atrophy and blindness, and extremity and abdominal compartment syndromes.

Figure 3. (A) Computed tomography scan of a child obtunded from a house fire; the ventricular system is compressed. (B) Same child 1 month later, lucid and restored to an edema-free brain. (Courtesy of Dr BA Pruitt)
Strategies to prevent fluid creep involve precise estimation of burn size, downward titration of fluid restriction based on renal output, and corrective measures if the prediction exceeds 6 mL/kg/%TBSA. Colloids should be routinely considered after 8 hours or as a rescue treatment. Other strategies include the use of hypertonic saline and high-dose ascorbic acid (vitamin C) infusion.13
Q4. What endpoints should be monitored during the initial period of fluid resuscitation?
While formulas can be used to initiate therapy, optimal outcomes require that burn resuscitation be tailored to the patient's physiological response to fluid therapy. Guides to adequate hydration rely on indirect measurement of oxygen delivery and tissue perfusion since direct invasive measurement carries significant morbidity. Hourly measurement of urine output (UO) is a vital parameter for gauging effective hydration, with targets of 0.5 mL/kg/hour for children weighing over 30 kg,5 0.5 to 1.0 mL/kg/hour for those less than 30 kg, and 1.0 to 2.0 mL/kg/hour for infants.14 However, assessment of UO may be misleading with oliguria from inappropriate antidiuretic hormone secretion or decreased renal perfusion in abdominal hypertension. The prerenal and renal causes of oliguria can be distinguished by measurement of the fractional excretion of sodium (Table 4).15

Table 4. The formula for fractional excretion of sodium (FeNa) used to differentiate a prerenal state from acute kidney injury. A normal functioning nephron in burn shock is associated with increased absorption of sodium, due to activation of the renin-angiotensin II-aldosterone system in response to decreased arterial pressure. A FeNa of less than 1% suggests a prerenal cause, whereas a FeNa greater than 1% suggests acute kidney injury.
Clinical signs such as alertness, warm skin, and strong peripheral pulses with good capillary refill indicate adequate resuscitation, while signs of dehydration include, lethargy, thirst, anxiety, cold dry mottled skin, and a rapid thready pulse. Mean arterial blood pressure may not change until the blood volume deficit exceeds 11%, so reduced pulse pressure is a more reliable indicator of volume contraction. The initial elevated hematocrit declines as blood volume is restored, and normal arterial lactate and base excess levels suggest adequate perfusion and tissue oxygenation. Transthoracic or transesophageal echocardiography can assess cardiac function in patients who fail to respond to conventional therapy. However, invasive cardiac monitoring, such as transpulmonary thermodilution, aimed at optimizing cardiac index and oxygen delivery through goal-directed therapy, has not demonstrated improved outcomes and may contribute to over-resuscitation.
Acknowledgments
Author: Stephen M. Milner, MBBS, BDS, DSc (Hon), FRCSE, FACS
Affiliation: Professor of Plastic and Reconstructive Surgery, Johns Hopkins University School of Medicine, Baltimore, MD (Ret.)
Correspondence: Stephen M. Milner, MBBS, BDS, DSc (Hon), FRCSE, FACS; stephenmilner123@gmail.com
Disclosures: The author discloses no relevant conflict of interest or financial disclosures for this manuscript.
References
1. Settle J. Principles of replacement fluid therapy. In: Settle JA, ed. Principles and Practice of Burns Management. Churchill Livingstone; 1996:217-222.
2. Marino P. The Little ICU Book. 2nd ed. Wolters Kluwer; 2017.
3. Greenhalgh DG. Management of burns. N Engl J Medicine. 2019;380(24):2349-2359. doi:10.1056/NEJMra1807442
4. Demling RH. The burn edema process: current concepts. J Burn Care Rehabil. 2005;26(3):207-227. doi:10.1097/01.BCR.0000162151.71482.B3
5. Romanowski KS, Palmieri TL. Pediatric burn resuscitation: past, present, and future. Burns Trauma. 2017;5:26. doi:10.1186/s41038-017-0091-y
6. Milner SM, Thomas JA, Grady JJ, Herndon DN. The clinical record of hypertonic saline in burn resuscitation: a meta-analysis of controlled clinical studies. J Burn Care Rehab 18:S88, 1997.
7. Baxter CR, Shires T. Physiological response to crystalloid resuscitation of severe burns. Ann N Y Acad Sci. 1968;150(3):874-894. doi:10.1111/j.1749-6632.1968.tb14738.x
8. Graves TA, Cioffi WG, McManus WF, Mason AD Jr, Pruitt BA Jr. Fluid resuscitation of infants and children with massive thermal Injury. J Trauma. 1988;28(12):1656-1659. doi:10.1097/00005373-198812000-00007
9. Carvajal H. Fluid resuscitation of pediatric burn victims: a critical appraisal. Pediatr Nephrol. 1994;8(3):357-366. doi:doi.org/10.1007/BF00866366
10. Akkawi El Edelbi R, Lindemalm S, Nydert P, Eksborg S. Estimation of body surface area in neonates, infants, and children using body weight alone. Int J Pediatr Adolesc Med. 2021;8(4):221-228. doi:10.1016/j.ijpam.2020.09.003
11. Warden GD. Burn shock resuscitation. World J Surg. 1992;16(1):16-23. doi:10.1007/BF02067109
12. Cancio LC, Chávez S, Alvarado-Ortega M, et al. Predicting increased fluid requirements during the resuscitation of thermally injured patients. J Trauma. 2004;56(2):404-414. doi:10.1097/01.TA.0000075341.43956.E4
13. Nakajima M, Kojiro M, Aso S, et al. Effect of high-dose vitamin C therapy on severe burn patients: a nationwide cohort study. Crit Care. 2019;23(1):407. doi:10.1186/s13054-019-2693-1
14. Sheridan R, Remensnyder J, Prelack K, Petras L, Lydon M. Treatment of the seriously burned infant. J Burn Care Rehabil. 1998;19(2):115-118. doi:10.1097/00004630-199803000-00005
15. Steiner RW. Interpreting the fractional excretion of sodium. Am J Med. 1984;77(4):699-702. doi:10.1016/0002-9343(84)90368-1