Patients with psoriatic arthritis (PsA) now have more options for treatment. In September, ustekinumab (Stelara) from Janssen Biotech, Inc. received FDA approval alone or in combination with methotrexate for the treatment of adult patients (18 years or older) with active PsA, the chronic autoimmune disease characterized by both joint inflammation and psoriasis skin lesions. Then less than 2 weeks later the agency granted granted regulatory clearance to certolizumab pegol (Cimzia, UCB, Inc.) for the treatment of adult patients with active PsA.
The RAPID-PsA Study
“The FDA’s approval of certolizumab pegol for the treatment of active PsA provides an additional, effective treatment option for those living with the condition. PsA brings with it a heavy disease burden that often strikes during the prime years of life, impacting health-related quality of life and physical function,” explains Philip J. Mease, MD, director rheumatology research, Swedish Medical Center and clinical professor, University of Washington School of Medicine, Seattle, WA. “The RAPID-PsA study supporting the US approval is the first randomized, controlled study of an anti-TNF in PsA to include patients with and without prior anti-tumor necrosisi factor (anti-TNF) exposure. The American College of Rheumatology ACR20 results showed that certolizumab pegol rapidly improved the signs and symptoms of PsA for patients with response observed as early as the first week of treatment for some patients.”
The drug’s FDA approval for active PsA is based on data from the RAPID-PsA study, an ongoing, Phase III, multicenter, randomized, double-blind, placebo-controlled trial designed to evaluate the efficacy and safety of certolizumab pegol in 409 patients with active and progressive adult onset PsA. Patients received a loading dose of certolizumab pegol 400 mg at weeks 0, 2 and 4 or placebo, followed by either certolizumab pegol 200 mg every other week, Certolizumab pegol 400 mg every 4 weeks, or placebo every other week.
Patients were evaluated for signs and symptoms of PsA using the ACR20 response at week 12 and for structural damage using the modified Total Sharp Score at week 24.5 ACR20, 50 and 70 response rates at weeks 12 and 24 were higher for each certolizumab pegol dose group relative to placebo. Patients treated with certolizumab pegol 200 mg every other week demonstrated greater reduction in radiographic progression compared with placebo-treated patients at week 24, as measured by change from baseline in total mTSS. Patients treated with certolizumab pegol 400 mg every 4 weeks did not demonstrate greater inhibition of radiographic progression at week 24, compared with placebo-treated patients. Treatment with certolizumab pegol also resulted in improvement in skin manifestations in patients with PsA.
Adverse events occurred in 62% of patients in the certolizumab pegol group (combined dose) compared to 68% of patients in the placebo group. Serious adverse events occurred in 7% of patients in the certolizumab pegol group (combined dose) compared to 4% of patients in the placebo group.
In the US, certolizumab pegol is also approved for the treatment of adults with moderately to severely active rheumatoid arthritis. In addition, it is approved for reducing signs and symptoms of Crohn’s disease and maintaining clinical response in adult patients with moderately to severely active disease who have had an inadequate response to conventional therapy.
The FDA is also reviewing a filing for certolizumab pegol in the treatment of adults with active axial spondyloarthritis, including patients with ankylosing spondylitis.
PSUMMIT I and PSUMMIT II
For the treatment of PsA, ustekinumab is administered as a 45 mg subcutaneous injection at weeks 0 and 4, and then every 12 weeks, thereafter. For patients with co-existent moderate-to-severe plaque psoriasis weighing more than 220 lbs. (100 kg), the recommended dose is 90 mg subcutaneous injection at weeks 0 and 4, and then every 12 weeks, thereafter.
“It is critical for dermatologists and rheumatologists to be able to offer new and novel treatment options to our adult patients living with PsA, a disease where additional biologic options are very much needed,” explains investigator and Steering Committee member Alice B. Gottlieb, MD, PhD, chief and dermatologist-in-chief, department of dermatology, Tufts Medical Center.
“Therapy that targets the cytokines interleukin-12 (IL-12) and interleukin-23 (IL-23), 2 naturally occurring proteins believed to play a role in the development of this debilitating immune-mediated inflammatory disease, could improve patient care,” she says.
The approval of ustekinumab is supported by findings from 2 pivotal, Phase III multicenter, randomized, double-blind, placebo-controlled trials of ustekinumab, a fully human anti–IL-12/23p40 monoclonal antibody, administered subcutaneously, in subjects with active psoriatic arthritis (PSUMMIT I and PSUMMIT II), which evaluated the efficacy and safety of subcutaneously-administered ustekinumab 45 mg or 90 mg at weeks 0, 4, and then every 12 weeks.
The trials included 927 patients diagnosed with active PsA who had at least 5 tender and 5 swollen joints and C-reactive protein levels of at least 0.3 mg/dL in spite of previous treatment with conventional therapy. PSUMMIT II also included 180 patients with previous exposure to 1 to 5 TNF inhibitors.
Results from PSUMMIT 1 showed that at week 24, 42% and 50 % of patients receiving ustekinumab 45 mg and 90 mg, respectively, achieved at least 20% improvement in signs and symptoms according ACR 20, the primary endpoint for both studies.
In PSUMMIT II, 44% of patients receiving ustekinumab 45 mg and 44% of patients receiving ustekinumab 90 mg achieved ACR 20 at week 24.
Additionally, ustekinumab improved soft tissue components of the disease, including dactylitis (inflammation of the finger or toe), enthesitis (inflammation of the entheses, the sites where tendons or ligaments attach to bone) and skin component as measured by Psoriasis Area and Severity Index score 75.
The safety results of ustekinumab observed in the PSUMMIT studies were consistent with the known safety profile of ustekinumab in the labeled moderate-to-severe plaque psoriasis indication, which has 5 years of safety experience in clinical trials, according to the company.
Study Finds Dissatisfaction and Undertreatment Among Psoriasis and Psoriatic Arthritis Patients
Many patients with psoriasis and psoriatic arthritis (PsA) are not benefiting from the expanding array of treatments now available to fight these serious autoimmune disorders. A new study, published in JAMA Dermatology, shows that non-treatment and undertreatment of patients with these disorders remain a significant problem in the United States.
Psoriasis affects about 7.5 million Americans and is responsible for more 11,000 cardiovascular disease deaths each year in the United States. An estimated 10%-30% of those with psoriasis develop PsA.
The study’s aim was to determine the extent of non-treatment and undertreatment of psoriatic diseases, trends in treatment use, treatment satisfaction and reasons for medication discontinuation among patients with psoriasis and PsA.
"The high proportion of patients who are not being treated, or are being inadequately treated, is a concern because psoriasis is much more than a cosmetic skin condition,” says April W. Armstrong, MD, lead investigator and an associate professor of dermatology at UC Davis. “It’s a serious and chronic medical disease.”
For the study, the researchers analyzed the responses of 5,604 randomly selected patients from 13 biannual surveys, which were conducted by the National Psoriasis Foundation between 2003 and 2011. During the study period, patients who reported not receiving any therapy for their conditions ranged from 36.%-49.2% of patients with mild psoriasis, 23.6%-35.5% of patients with moderate psoriasis and 9.4%-29.7% of patients with severe psoriasis.
Patients with moderate-to-severe psoriasis often need systemic therapies as well as topical therapies to control their disease. However, according to the surveys, among those receiving treatment, 29.5% of patients with moderate psoriasis were on topical therapy alone, and 21.5% of patients with severe psoriasis were on topical treatments alone. Dr. Armstrong says that patients with moderate-to-severe psoriasis are often those who require more than just topical treatments to control their psoriasis. However, many patients have difficulty obtaining adequate systemic treatment due to health insurance constraints.
“Unfortunately, there are real barriers that prevent patients from being treated,” says Mark G. Lebwohl, MD, the study’s senior author and professor and chair of dermatology at Mount Sinai Medical Center in New York City. “Nearly every practicing dermatologist in the United States has written a prescription that has been denied by an insurance company.”
Dr. Lebwohl adds that even though phototherapy is a safe and effective therapy, it is no longer widely used because of the high copayments charged by insurance companies and their low reimbursement rates for the physician’s cost of providing the treatment. According to the American Academy of Dermatology, less than a third of practicing dermatologists now offer phototherapy as a treatment option for psoriasis.
The study also found that overall 52.3% of patients with psoriasis and 45.5% of patients with PsA were dissatisfied with their treatment. The researchers suggest that the high level of dissatisfaction may be due in part to ineffective therapies or patients not comprehending that psoriasis and PsA are chronic diseases, with symptoms that typically come and go even during clinical treatment.
To address the treatment challenges for psoriasis and PsA suffers, the researchers encourage more patient advocacy directed at payers. They also emphasize the need for more patient education and awareness about the risk of cardiovascular disease.
Armstrong AW, Robertson AD, Wu J, Schupp C, Lebwohl MG. Undertreatment, treatment trends, and treatment dissatisfaction among patients with psoriasis and psoriatic arthritis in the United States: Findings from the National Psoriasis Foundation Surveys, 2003-2011. JAMA Dermatol. Published online ahead of print August 14, 2013.
Psoriasis Linked with Other Serious Medical Conditions
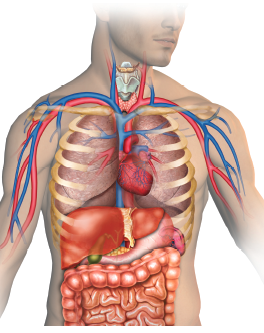 Although considered a disease limited to the skin and joints, increasing evidence suggests that psoriasis, a common, autoimmune disease affecting 2% - 3% of the population, has far-reaching systemic effects. A recent study by Yeung et al published in JAMA Dermatology demonstrates that psoriasis is linked to an increased presence of other diseases that affect the lungs, heart, kidneys, liver and pancreas.
Although considered a disease limited to the skin and joints, increasing evidence suggests that psoriasis, a common, autoimmune disease affecting 2% - 3% of the population, has far-reaching systemic effects. A recent study by Yeung et al published in JAMA Dermatology demonstrates that psoriasis is linked to an increased presence of other diseases that affect the lungs, heart, kidneys, liver and pancreas.
To determine the prevalence of major medical comorbidity in patients with psoriasis, researchers from the University of Pennsylvania conducted a population-based, cross-sectional study using data from The Health Improvement Network (THIN), an electronic medical records database in the United Kingdom. The version of THIN used in this study included longitudinal data on 7.5 million registered patients from 415 general practices. The researchers analyzed data from 9,035 psoriasis patients age 25 to 64 and 90,350 age- and practice-matched patients without psoriasis. The researchers then mailed questionnaires to each patient’s general practitioner to verify the presence of psoriasis and assess the extent of disease. The practitioners rated the severity of psoriasis for each patient as mild, moderate or severe based on the amount of body surface area affected. The primary endpoint was the prevalence of major medical comorbidity included in the Charlson comorbidity index.
Among the patients with psoriasis, 51.8%, 35.8% and 12.4%, respectively, had mild, moderate or severe disease. Systemic therapy and/or phototherapy use was recorded before assessment of disease severity in 137 of the patients with mild, 278 with moderate and 322 with severe psoriasis. The mean Charlson comorbidity index was increasingly higher in the psoriasis group versus the control group across all categories of psoriasis severity (mild, 0.375 vs 0.347; moderate, 0.398 vs 0.342 and severe, 0.450 vs 0.348, respectively; all P<.05). Trend analysis of Charlson index scores by disease severity also showed significant associations. After adjustment for age, sex and follow-up duration, patients with mild (odds ratio [OR, 1.11; 95% confidence interval [CI], 1.03-1.19), moderate (OR, 1.15; 95% CI, 1.05-1.25) or severe psoriasis (OR, 1.35; 95% CI, 1.16-1.56) had higher odds of having at least 1 major comorbid disease than patients without psoriasis.
Psoriasis overall was associated with a higher prevalence of chronic pulmonary disease (adjusted OR, 1.08; 95% CI, 1.02-1.15), diabetes (OR, 1.22; 95% CI, 1.11-1.35), diabetes with systemic complications (OR, 1.34; 95% CI, 1.11-1.62), mild liver disease (OR, 1.41; 95% CI, 1.12-1.76), myocardial infarction (OR, 1.34; 95% CI, 1.07-1.69), peptic ulcer disease (OR, 1.27; 95% CI, 1.03-1.58), peripheral vascular disease (OR, 1.38; 95% CI, 1.07-1.77), renal disease (OR, 1.28; 95% CI, 1.11-1.48) and rheumatic disease (OR, 2.04; 95% CI, 1.71-2.42). Significant associations were not observed between psoriasis or the prevalence of cancer, metastatic tumor or congestive heart failure.
“The burdens of overall medical comorbidity and of specific comorbid diseases increases with increasingly severity among patients with psoriasis,” the researchers conclude. “Physicians should be aware of these associations in providing comprehensive care to patients with psoriasis, especially those presenting with more severe disease.”
Yeung H, Takeshita J, Mehta NN, et al. Psoriasis severity and prevalence of major medical comorbidity: A population-based study. JAMA Dermatol. Published online ahead of print August 7, 2013.
Patients with psoriatic arthritis (PsA) now have more options for treatment. In September, ustekinumab (Stelara) from Janssen Biotech, Inc. received FDA approval alone or in combination with methotrexate for the treatment of adult patients (18 years or older) with active PsA, the chronic autoimmune disease characterized by both joint inflammation and psoriasis skin lesions. Then less than 2 weeks later the agency granted granted regulatory clearance to certolizumab pegol (Cimzia, UCB, Inc.) for the treatment of adult patients with active PsA.
The RAPID-PsA Study
“The FDA’s approval of certolizumab pegol for the treatment of active PsA provides an additional, effective treatment option for those living with the condition. PsA brings with it a heavy disease burden that often strikes during the prime years of life, impacting health-related quality of life and physical function,” explains Philip J. Mease, MD, director rheumatology research, Swedish Medical Center and clinical professor, University of Washington School of Medicine, Seattle, WA. “The RAPID-PsA study supporting the US approval is the first randomized, controlled study of an anti-TNF in PsA to include patients with and without prior anti-tumor necrosisi factor (anti-TNF) exposure. The American College of Rheumatology ACR20 results showed that certolizumab pegol rapidly improved the signs and symptoms of PsA for patients with response observed as early as the first week of treatment for some patients.”
The drug’s FDA approval for active PsA is based on data from the RAPID-PsA study, an ongoing, Phase III, multicenter, randomized, double-blind, placebo-controlled trial designed to evaluate the efficacy and safety of certolizumab pegol in 409 patients with active and progressive adult onset PsA. Patients received a loading dose of certolizumab pegol 400 mg at weeks 0, 2 and 4 or placebo, followed by either certolizumab pegol 200 mg every other week, Certolizumab pegol 400 mg every 4 weeks, or placebo every other week.
Patients were evaluated for signs and symptoms of PsA using the ACR20 response at week 12 and for structural damage using the modified Total Sharp Score at week 24.5 ACR20, 50 and 70 response rates at weeks 12 and 24 were higher for each certolizumab pegol dose group relative to placebo. Patients treated with certolizumab pegol 200 mg every other week demonstrated greater reduction in radiographic progression compared with placebo-treated patients at week 24, as measured by change from baseline in total mTSS. Patients treated with certolizumab pegol 400 mg every 4 weeks did not demonstrate greater inhibition of radiographic progression at week 24, compared with placebo-treated patients. Treatment with certolizumab pegol also resulted in improvement in skin manifestations in patients with PsA.
Adverse events occurred in 62% of patients in the certolizumab pegol group (combined dose) compared to 68% of patients in the placebo group. Serious adverse events occurred in 7% of patients in the certolizumab pegol group (combined dose) compared to 4% of patients in the placebo group.
In the US, certolizumab pegol is also approved for the treatment of adults with moderately to severely active rheumatoid arthritis. In addition, it is approved for reducing signs and symptoms of Crohn’s disease and maintaining clinical response in adult patients with moderately to severely active disease who have had an inadequate response to conventional therapy.
The FDA is also reviewing a filing for certolizumab pegol in the treatment of adults with active axial spondyloarthritis, including patients with ankylosing spondylitis.
PSUMMIT I and PSUMMIT II
For the treatment of PsA, ustekinumab is administered as a 45 mg subcutaneous injection at weeks 0 and 4, and then every 12 weeks, thereafter. For patients with co-existent moderate-to-severe plaque psoriasis weighing more than 220 lbs. (100 kg), the recommended dose is 90 mg subcutaneous injection at weeks 0 and 4, and then every 12 weeks, thereafter.
“It is critical for dermatologists and rheumatologists to be able to offer new and novel treatment options to our adult patients living with PsA, a disease where additional biologic options are very much needed,” explains investigator and Steering Committee member Alice B. Gottlieb, MD, PhD, chief and dermatologist-in-chief, department of dermatology, Tufts Medical Center.
“Therapy that targets the cytokines interleukin-12 (IL-12) and interleukin-23 (IL-23), 2 naturally occurring proteins believed to play a role in the development of this debilitating immune-mediated inflammatory disease, could improve patient care,” she says.
The approval of ustekinumab is supported by findings from 2 pivotal, Phase III multicenter, randomized, double-blind, placebo-controlled trials of ustekinumab, a fully human anti–IL-12/23p40 monoclonal antibody, administered subcutaneously, in subjects with active psoriatic arthritis (PSUMMIT I and PSUMMIT II), which evaluated the efficacy and safety of subcutaneously-administered ustekinumab 45 mg or 90 mg at weeks 0, 4, and then every 12 weeks.
The trials included 927 patients diagnosed with active PsA who had at least 5 tender and 5 swollen joints and C-reactive protein levels of at least 0.3 mg/dL in spite of previous treatment with conventional therapy. PSUMMIT II also included 180 patients with previous exposure to 1 to 5 TNF inhibitors.
Results from PSUMMIT 1 showed that at week 24, 42% and 50 % of patients receiving ustekinumab 45 mg and 90 mg, respectively, achieved at least 20% improvement in signs and symptoms according ACR 20, the primary endpoint for both studies.
In PSUMMIT II, 44% of patients receiving ustekinumab 45 mg and 44% of patients receiving ustekinumab 90 mg achieved ACR 20 at week 24.
Additionally, ustekinumab improved soft tissue components of the disease, including dactylitis (inflammation of the finger or toe), enthesitis (inflammation of the entheses, the sites where tendons or ligaments attach to bone) and skin component as measured by Psoriasis Area and Severity Index score 75.
The safety results of ustekinumab observed in the PSUMMIT studies were consistent with the known safety profile of ustekinumab in the labeled moderate-to-severe plaque psoriasis indication, which has 5 years of safety experience in clinical trials, according to the company.
Study Finds Dissatisfaction and Undertreatment Among Psoriasis and Psoriatic Arthritis Patients
Many patients with psoriasis and psoriatic arthritis (PsA) are not benefiting from the expanding array of treatments now available to fight these serious autoimmune disorders. A new study, published in JAMA Dermatology, shows that non-treatment and undertreatment of patients with these disorders remain a significant problem in the United States.
Psoriasis affects about 7.5 million Americans and is responsible for more 11,000 cardiovascular disease deaths each year in the United States. An estimated 10%-30% of those with psoriasis develop PsA.
The study’s aim was to determine the extent of non-treatment and undertreatment of psoriatic diseases, trends in treatment use, treatment satisfaction and reasons for medication discontinuation among patients with psoriasis and PsA.
"The high proportion of patients who are not being treated, or are being inadequately treated, is a concern because psoriasis is much more than a cosmetic skin condition,” says April W. Armstrong, MD, lead investigator and an associate professor of dermatology at UC Davis. “It’s a serious and chronic medical disease.”
For the study, the researchers analyzed the responses of 5,604 randomly selected patients from 13 biannual surveys, which were conducted by the National Psoriasis Foundation between 2003 and 2011. During the study period, patients who reported not receiving any therapy for their conditions ranged from 36.%-49.2% of patients with mild psoriasis, 23.6%-35.5% of patients with moderate psoriasis and 9.4%-29.7% of patients with severe psoriasis.
Patients with moderate-to-severe psoriasis often need systemic therapies as well as topical therapies to control their disease. However, according to the surveys, among those receiving treatment, 29.5% of patients with moderate psoriasis were on topical therapy alone, and 21.5% of patients with severe psoriasis were on topical treatments alone. Dr. Armstrong says that patients with moderate-to-severe psoriasis are often those who require more than just topical treatments to control their psoriasis. However, many patients have difficulty obtaining adequate systemic treatment due to health insurance constraints.
“Unfortunately, there are real barriers that prevent patients from being treated,” says Mark G. Lebwohl, MD, the study’s senior author and professor and chair of dermatology at Mount Sinai Medical Center in New York City. “Nearly every practicing dermatologist in the United States has written a prescription that has been denied by an insurance company.”
Dr. Lebwohl adds that even though phototherapy is a safe and effective therapy, it is no longer widely used because of the high copayments charged by insurance companies and their low reimbursement rates for the physician’s cost of providing the treatment. According to the American Academy of Dermatology, less than a third of practicing dermatologists now offer phototherapy as a treatment option for psoriasis.
The study also found that overall 52.3% of patients with psoriasis and 45.5% of patients with PsA were dissatisfied with their treatment. The researchers suggest that the high level of dissatisfaction may be due in part to ineffective therapies or patients not comprehending that psoriasis and PsA are chronic diseases, with symptoms that typically come and go even during clinical treatment.
To address the treatment challenges for psoriasis and PsA suffers, the researchers encourage more patient advocacy directed at payers. They also emphasize the need for more patient education and awareness about the risk of cardiovascular disease.
Armstrong AW, Robertson AD, Wu J, Schupp C, Lebwohl MG. Undertreatment, treatment trends, and treatment dissatisfaction among patients with psoriasis and psoriatic arthritis in the United States: Findings from the National Psoriasis Foundation Surveys, 2003-2011. JAMA Dermatol. Published online ahead of print August 14, 2013.
Psoriasis Linked with Other Serious Medical Conditions
 Although considered a disease limited to the skin and joints, increasing evidence suggests that psoriasis, a common, autoimmune disease affecting 2% - 3% of the population, has far-reaching systemic effects. A recent study by Yeung et al published in JAMA Dermatology demonstrates that psoriasis is linked to an increased presence of other diseases that affect the lungs, heart, kidneys, liver and pancreas.
Although considered a disease limited to the skin and joints, increasing evidence suggests that psoriasis, a common, autoimmune disease affecting 2% - 3% of the population, has far-reaching systemic effects. A recent study by Yeung et al published in JAMA Dermatology demonstrates that psoriasis is linked to an increased presence of other diseases that affect the lungs, heart, kidneys, liver and pancreas.
To determine the prevalence of major medical comorbidity in patients with psoriasis, researchers from the University of Pennsylvania conducted a population-based, cross-sectional study using data from The Health Improvement Network (THIN), an electronic medical records database in the United Kingdom. The version of THIN used in this study included longitudinal data on 7.5 million registered patients from 415 general practices. The researchers analyzed data from 9,035 psoriasis patients age 25 to 64 and 90,350 age- and practice-matched patients without psoriasis. The researchers then mailed questionnaires to each patient’s general practitioner to verify the presence of psoriasis and assess the extent of disease. The practitioners rated the severity of psoriasis for each patient as mild, moderate or severe based on the amount of body surface area affected. The primary endpoint was the prevalence of major medical comorbidity included in the Charlson comorbidity index.
Among the patients with psoriasis, 51.8%, 35.8% and 12.4%, respectively, had mild, moderate or severe disease. Systemic therapy and/or phototherapy use was recorded before assessment of disease severity in 137 of the patients with mild, 278 with moderate and 322 with severe psoriasis. The mean Charlson comorbidity index was increasingly higher in the psoriasis group versus the control group across all categories of psoriasis severity (mild, 0.375 vs 0.347; moderate, 0.398 vs 0.342 and severe, 0.450 vs 0.348, respectively; all P<.05). Trend analysis of Charlson index scores by disease severity also showed significant associations. After adjustment for age, sex and follow-up duration, patients with mild (odds ratio [OR, 1.11; 95% confidence interval [CI], 1.03-1.19), moderate (OR, 1.15; 95% CI, 1.05-1.25) or severe psoriasis (OR, 1.35; 95% CI, 1.16-1.56) had higher odds of having at least 1 major comorbid disease than patients without psoriasis.
Psoriasis overall was associated with a higher prevalence of chronic pulmonary disease (adjusted OR, 1.08; 95% CI, 1.02-1.15), diabetes (OR, 1.22; 95% CI, 1.11-1.35), diabetes with systemic complications (OR, 1.34; 95% CI, 1.11-1.62), mild liver disease (OR, 1.41; 95% CI, 1.12-1.76), myocardial infarction (OR, 1.34; 95% CI, 1.07-1.69), peptic ulcer disease (OR, 1.27; 95% CI, 1.03-1.58), peripheral vascular disease (OR, 1.38; 95% CI, 1.07-1.77), renal disease (OR, 1.28; 95% CI, 1.11-1.48) and rheumatic disease (OR, 2.04; 95% CI, 1.71-2.42). Significant associations were not observed between psoriasis or the prevalence of cancer, metastatic tumor or congestive heart failure.
“The burdens of overall medical comorbidity and of specific comorbid diseases increases with increasingly severity among patients with psoriasis,” the researchers conclude. “Physicians should be aware of these associations in providing comprehensive care to patients with psoriasis, especially those presenting with more severe disease.”
Yeung H, Takeshita J, Mehta NN, et al. Psoriasis severity and prevalence of major medical comorbidity: A population-based study. JAMA Dermatol. Published online ahead of print August 7, 2013.
Patients with psoriatic arthritis (PsA) now have more options for treatment. In September, ustekinumab (Stelara) from Janssen Biotech, Inc. received FDA approval alone or in combination with methotrexate for the treatment of adult patients (18 years or older) with active PsA, the chronic autoimmune disease characterized by both joint inflammation and psoriasis skin lesions. Then less than 2 weeks later the agency granted granted regulatory clearance to certolizumab pegol (Cimzia, UCB, Inc.) for the treatment of adult patients with active PsA.
The RAPID-PsA Study
“The FDA’s approval of certolizumab pegol for the treatment of active PsA provides an additional, effective treatment option for those living with the condition. PsA brings with it a heavy disease burden that often strikes during the prime years of life, impacting health-related quality of life and physical function,” explains Philip J. Mease, MD, director rheumatology research, Swedish Medical Center and clinical professor, University of Washington School of Medicine, Seattle, WA. “The RAPID-PsA study supporting the US approval is the first randomized, controlled study of an anti-TNF in PsA to include patients with and without prior anti-tumor necrosisi factor (anti-TNF) exposure. The American College of Rheumatology ACR20 results showed that certolizumab pegol rapidly improved the signs and symptoms of PsA for patients with response observed as early as the first week of treatment for some patients.”
The drug’s FDA approval for active PsA is based on data from the RAPID-PsA study, an ongoing, Phase III, multicenter, randomized, double-blind, placebo-controlled trial designed to evaluate the efficacy and safety of certolizumab pegol in 409 patients with active and progressive adult onset PsA. Patients received a loading dose of certolizumab pegol 400 mg at weeks 0, 2 and 4 or placebo, followed by either certolizumab pegol 200 mg every other week, Certolizumab pegol 400 mg every 4 weeks, or placebo every other week.
Patients were evaluated for signs and symptoms of PsA using the ACR20 response at week 12 and for structural damage using the modified Total Sharp Score at week 24.5 ACR20, 50 and 70 response rates at weeks 12 and 24 were higher for each certolizumab pegol dose group relative to placebo. Patients treated with certolizumab pegol 200 mg every other week demonstrated greater reduction in radiographic progression compared with placebo-treated patients at week 24, as measured by change from baseline in total mTSS. Patients treated with certolizumab pegol 400 mg every 4 weeks did not demonstrate greater inhibition of radiographic progression at week 24, compared with placebo-treated patients. Treatment with certolizumab pegol also resulted in improvement in skin manifestations in patients with PsA.
Adverse events occurred in 62% of patients in the certolizumab pegol group (combined dose) compared to 68% of patients in the placebo group. Serious adverse events occurred in 7% of patients in the certolizumab pegol group (combined dose) compared to 4% of patients in the placebo group.
In the US, certolizumab pegol is also approved for the treatment of adults with moderately to severely active rheumatoid arthritis. In addition, it is approved for reducing signs and symptoms of Crohn’s disease and maintaining clinical response in adult patients with moderately to severely active disease who have had an inadequate response to conventional therapy.
The FDA is also reviewing a filing for certolizumab pegol in the treatment of adults with active axial spondyloarthritis, including patients with ankylosing spondylitis.
PSUMMIT I and PSUMMIT II
For the treatment of PsA, ustekinumab is administered as a 45 mg subcutaneous injection at weeks 0 and 4, and then every 12 weeks, thereafter. For patients with co-existent moderate-to-severe plaque psoriasis weighing more than 220 lbs. (100 kg), the recommended dose is 90 mg subcutaneous injection at weeks 0 and 4, and then every 12 weeks, thereafter.
“It is critical for dermatologists and rheumatologists to be able to offer new and novel treatment options to our adult patients living with PsA, a disease where additional biologic options are very much needed,” explains investigator and Steering Committee member Alice B. Gottlieb, MD, PhD, chief and dermatologist-in-chief, department of dermatology, Tufts Medical Center.
“Therapy that targets the cytokines interleukin-12 (IL-12) and interleukin-23 (IL-23), 2 naturally occurring proteins believed to play a role in the development of this debilitating immune-mediated inflammatory disease, could improve patient care,” she says.
The approval of ustekinumab is supported by findings from 2 pivotal, Phase III multicenter, randomized, double-blind, placebo-controlled trials of ustekinumab, a fully human anti–IL-12/23p40 monoclonal antibody, administered subcutaneously, in subjects with active psoriatic arthritis (PSUMMIT I and PSUMMIT II), which evaluated the efficacy and safety of subcutaneously-administered ustekinumab 45 mg or 90 mg at weeks 0, 4, and then every 12 weeks.
The trials included 927 patients diagnosed with active PsA who had at least 5 tender and 5 swollen joints and C-reactive protein levels of at least 0.3 mg/dL in spite of previous treatment with conventional therapy. PSUMMIT II also included 180 patients with previous exposure to 1 to 5 TNF inhibitors.
Results from PSUMMIT 1 showed that at week 24, 42% and 50 % of patients receiving ustekinumab 45 mg and 90 mg, respectively, achieved at least 20% improvement in signs and symptoms according ACR 20, the primary endpoint for both studies.
In PSUMMIT II, 44% of patients receiving ustekinumab 45 mg and 44% of patients receiving ustekinumab 90 mg achieved ACR 20 at week 24.
Additionally, ustekinumab improved soft tissue components of the disease, including dactylitis (inflammation of the finger or toe), enthesitis (inflammation of the entheses, the sites where tendons or ligaments attach to bone) and skin component as measured by Psoriasis Area and Severity Index score 75.
The safety results of ustekinumab observed in the PSUMMIT studies were consistent with the known safety profile of ustekinumab in the labeled moderate-to-severe plaque psoriasis indication, which has 5 years of safety experience in clinical trials, according to the company.
Study Finds Dissatisfaction and Undertreatment Among Psoriasis and Psoriatic Arthritis Patients
Many patients with psoriasis and psoriatic arthritis (PsA) are not benefiting from the expanding array of treatments now available to fight these serious autoimmune disorders. A new study, published in JAMA Dermatology, shows that non-treatment and undertreatment of patients with these disorders remain a significant problem in the United States.
Psoriasis affects about 7.5 million Americans and is responsible for more 11,000 cardiovascular disease deaths each year in the United States. An estimated 10%-30% of those with psoriasis develop PsA.
The study’s aim was to determine the extent of non-treatment and undertreatment of psoriatic diseases, trends in treatment use, treatment satisfaction and reasons for medication discontinuation among patients with psoriasis and PsA.
"The high proportion of patients who are not being treated, or are being inadequately treated, is a concern because psoriasis is much more than a cosmetic skin condition,” says April W. Armstrong, MD, lead investigator and an associate professor of dermatology at UC Davis. “It’s a serious and chronic medical disease.”
For the study, the researchers analyzed the responses of 5,604 randomly selected patients from 13 biannual surveys, which were conducted by the National Psoriasis Foundation between 2003 and 2011. During the study period, patients who reported not receiving any therapy for their conditions ranged from 36.%-49.2% of patients with mild psoriasis, 23.6%-35.5% of patients with moderate psoriasis and 9.4%-29.7% of patients with severe psoriasis.
Patients with moderate-to-severe psoriasis often need systemic therapies as well as topical therapies to control their disease. However, according to the surveys, among those receiving treatment, 29.5% of patients with moderate psoriasis were on topical therapy alone, and 21.5% of patients with severe psoriasis were on topical treatments alone. Dr. Armstrong says that patients with moderate-to-severe psoriasis are often those who require more than just topical treatments to control their psoriasis. However, many patients have difficulty obtaining adequate systemic treatment due to health insurance constraints.
“Unfortunately, there are real barriers that prevent patients from being treated,” says Mark G. Lebwohl, MD, the study’s senior author and professor and chair of dermatology at Mount Sinai Medical Center in New York City. “Nearly every practicing dermatologist in the United States has written a prescription that has been denied by an insurance company.”
Dr. Lebwohl adds that even though phototherapy is a safe and effective therapy, it is no longer widely used because of the high copayments charged by insurance companies and their low reimbursement rates for the physician’s cost of providing the treatment. According to the American Academy of Dermatology, less than a third of practicing dermatologists now offer phototherapy as a treatment option for psoriasis.
The study also found that overall 52.3% of patients with psoriasis and 45.5% of patients with PsA were dissatisfied with their treatment. The researchers suggest that the high level of dissatisfaction may be due in part to ineffective therapies or patients not comprehending that psoriasis and PsA are chronic diseases, with symptoms that typically come and go even during clinical treatment.
To address the treatment challenges for psoriasis and PsA suffers, the researchers encourage more patient advocacy directed at payers. They also emphasize the need for more patient education and awareness about the risk of cardiovascular disease.
Armstrong AW, Robertson AD, Wu J, Schupp C, Lebwohl MG. Undertreatment, treatment trends, and treatment dissatisfaction among patients with psoriasis and psoriatic arthritis in the United States: Findings from the National Psoriasis Foundation Surveys, 2003-2011. JAMA Dermatol. Published online ahead of print August 14, 2013.
Psoriasis Linked with Other Serious Medical Conditions
 Although considered a disease limited to the skin and joints, increasing evidence suggests that psoriasis, a common, autoimmune disease affecting 2% - 3% of the population, has far-reaching systemic effects. A recent study by Yeung et al published in JAMA Dermatology demonstrates that psoriasis is linked to an increased presence of other diseases that affect the lungs, heart, kidneys, liver and pancreas.
Although considered a disease limited to the skin and joints, increasing evidence suggests that psoriasis, a common, autoimmune disease affecting 2% - 3% of the population, has far-reaching systemic effects. A recent study by Yeung et al published in JAMA Dermatology demonstrates that psoriasis is linked to an increased presence of other diseases that affect the lungs, heart, kidneys, liver and pancreas.
To determine the prevalence of major medical comorbidity in patients with psoriasis, researchers from the University of Pennsylvania conducted a population-based, cross-sectional study using data from The Health Improvement Network (THIN), an electronic medical records database in the United Kingdom. The version of THIN used in this study included longitudinal data on 7.5 million registered patients from 415 general practices. The researchers analyzed data from 9,035 psoriasis patients age 25 to 64 and 90,350 age- and practice-matched patients without psoriasis. The researchers then mailed questionnaires to each patient’s general practitioner to verify the presence of psoriasis and assess the extent of disease. The practitioners rated the severity of psoriasis for each patient as mild, moderate or severe based on the amount of body surface area affected. The primary endpoint was the prevalence of major medical comorbidity included in the Charlson comorbidity index.
Among the patients with psoriasis, 51.8%, 35.8% and 12.4%, respectively, had mild, moderate or severe disease. Systemic therapy and/or phototherapy use was recorded before assessment of disease severity in 137 of the patients with mild, 278 with moderate and 322 with severe psoriasis. The mean Charlson comorbidity index was increasingly higher in the psoriasis group versus the control group across all categories of psoriasis severity (mild, 0.375 vs 0.347; moderate, 0.398 vs 0.342 and severe, 0.450 vs 0.348, respectively; all P<.05). Trend analysis of Charlson index scores by disease severity also showed significant associations. After adjustment for age, sex and follow-up duration, patients with mild (odds ratio [OR, 1.11; 95% confidence interval [CI], 1.03-1.19), moderate (OR, 1.15; 95% CI, 1.05-1.25) or severe psoriasis (OR, 1.35; 95% CI, 1.16-1.56) had higher odds of having at least 1 major comorbid disease than patients without psoriasis.
Psoriasis overall was associated with a higher prevalence of chronic pulmonary disease (adjusted OR, 1.08; 95% CI, 1.02-1.15), diabetes (OR, 1.22; 95% CI, 1.11-1.35), diabetes with systemic complications (OR, 1.34; 95% CI, 1.11-1.62), mild liver disease (OR, 1.41; 95% CI, 1.12-1.76), myocardial infarction (OR, 1.34; 95% CI, 1.07-1.69), peptic ulcer disease (OR, 1.27; 95% CI, 1.03-1.58), peripheral vascular disease (OR, 1.38; 95% CI, 1.07-1.77), renal disease (OR, 1.28; 95% CI, 1.11-1.48) and rheumatic disease (OR, 2.04; 95% CI, 1.71-2.42). Significant associations were not observed between psoriasis or the prevalence of cancer, metastatic tumor or congestive heart failure.
“The burdens of overall medical comorbidity and of specific comorbid diseases increases with increasingly severity among patients with psoriasis,” the researchers conclude. “Physicians should be aware of these associations in providing comprehensive care to patients with psoriasis, especially those presenting with more severe disease.”
Yeung H, Takeshita J, Mehta NN, et al. Psoriasis severity and prevalence of major medical comorbidity: A population-based study. JAMA Dermatol. Published online ahead of print August 7, 2013.
 Although considered a disease limited to the skin and joints, increasing evidence suggests that psoriasis, a common, autoimmune disease affecting 2% - 3% of the population, has far-reaching systemic effects. A recent study by Yeung et al published in JAMA Dermatology demonstrates that psoriasis is linked to an increased presence of other diseases that affect the lungs, heart, kidneys, liver and pancreas.
Although considered a disease limited to the skin and joints, increasing evidence suggests that psoriasis, a common, autoimmune disease affecting 2% - 3% of the population, has far-reaching systemic effects. A recent study by Yeung et al published in JAMA Dermatology demonstrates that psoriasis is linked to an increased presence of other diseases that affect the lungs, heart, kidneys, liver and pancreas.





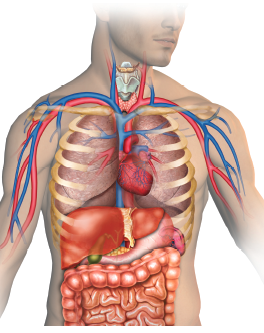 Although considered a disease limited to the skin and joints, increasing evidence suggests that psoriasis, a common, autoimmune disease affecting 2% - 3% of the population, has far-reaching systemic effects. A recent study by Yeung et al published in JAMA Dermatology demonstrates that psoriasis is linked to an increased presence of other diseases that affect the lungs, heart, kidneys, liver and pancreas.
Although considered a disease limited to the skin and joints, increasing evidence suggests that psoriasis, a common, autoimmune disease affecting 2% - 3% of the population, has far-reaching systemic effects. A recent study by Yeung et al published in JAMA Dermatology demonstrates that psoriasis is linked to an increased presence of other diseases that affect the lungs, heart, kidneys, liver and pancreas.



















