Figure 1.
A 32-year-old man presented with a lesion on the dorsum of the left index finger that appeared 2 weeks prior to his presentation to the clinic. The lesion grew in size from a pinpoint papule to its current size. On physical examination, there was a weeping yellowish nodule overlying an erythematous base on the inner dorsal aspect of the left index finger at the metacarpal-phalangeal joint level. Overlying this nodule was a 2.2 cm x 2.1 cm ulcer (Figure).
What is Your Diagnosis?
To learn the answer, go to page 2
{{pagebreak}}
Diagnosis: ORF Virus
Orf virus (OrfV), also known as ecthyma contagiosum, is a double-stranded DNA virus that belongs to the Parapoxvirus genus.1 In regards to epidemiology, antibodies against OrfV were reported in 3 flocks from Hokkaido and Iwate prefectures in Japan (2.57% of all sheep tested in northern Japan). The 6 positive animals were all Suffolk ewes of 5 to 7 years of age.2
Clinical Presentation
OrfV usually infects sheep and goat hosts, resulting in a zoonotic infection characterized by acute, highly vascularized cutaneous pustular lesions.
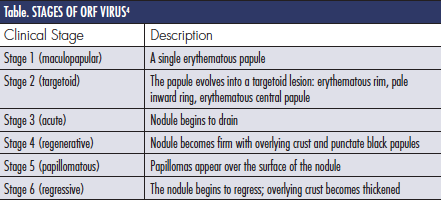
In humans, the disease usually presents as a painful nodule on the dorsal side of the fingers or hands (Figure). This regresses spontaneously without scar formation within 2 months. It has been reported in children after visiting petting zoos and livestock fairs.3 Human infection is rare. OrfV infection usually goes through 6 stages. Each stage usually lasts about 1 week. The stages are summarized in the Table.4
OrfV is often transmitted to humans by direct contact with infected animals. One hunter developed an OrfV lesion on the finger, which he acquired 3 weeks previously while he was handling a chamois carcass.5 A 42-year-old man presented with multiple nodular lesions on his right wrist after incurring an injury during ovine slaughter.6 There was also a reported outbreak among handlers of black goats in China.7 One article described a mother and son in the Gansu province of China who were infected with OrfV.1
Some cases of OrfV have been reported during religious practices. A 34-year-old Muslim man from Tunisia acquired OrfV infection on his left hand after he handled lamb meat during the Feast of Sacrifice. A 57-year-old Jewish man acquired OrfV on his left finger after the ritual of declaring lamb meat kosher.8 This virus also occurred in 5 individuals in France during the Eid-al-Adha practice.9
The transmission of OrfV from human to human is extremely rare. Only 4 cases have been described in the literature: a nurse who had changed the dressings of an infected patient, 2 cases of a child from an infected mother and a woman who contracted lesions on her cheek from her husband, a farmer.10 The first reported outbreak of a nosocomial OrfV infection occurred from October to December 2012 in a hospital burn unit in Gaziantep, Turkey; 13 patients became infected.11
Another report described an outbreak in Brazil in which a co-infection with Orf and vaccinia virus occurred in cows. The cows exhibited painful erythematous papules and vesicles in the teats for up to 3 weeks. Two people milking the affected cows developed the same painful lesions in 4 to 7 days; these later ulcerated and scabbed.12 The same co-infection occurred in goats in Brazil.13
Pathology
Histological analysis demonstrates balloon degeneration in the epidermis. Lymphocytes, neutrophils and abundant eosinophils are signs of most cutaneous viral infection. Indirect immunofluorescence may show anti-orf immunoglobulin (Ig) G earlier in the course, followed by both anti-orf IgG and IgM during convalescence.14
Diagnosis is made by Parapoxvirus RNA polymerase gene sequences, which can specifically detect Orf and other species in this genus.15 One group found that diagnosis from scabs of sheep and goats via counterimmunoelectrophoresis, conventional PCR, and rt-PCR was positive in 21.4%, 51.4% and 92.9%, respectively. This means that rt-PCR is the most sensitive tool in the diagnosis of OrfV. Furthermore, the rt-PCR is simpler and quicker compared to conventional PCR, which requires 2 rounds of PCR amplification.16
A novel technique known as flexible loop-mediated isothermal amplification (LAMP) can rapidly detect OrfV with high specificity and sensitivity. In contrast to PCR, in which the reaction is carried out with a series of alternating temperature steps, isothermal amplification is carried out at a single temperature, and does not require a thermal cycler. As a result, LAMP is a simple screening assay that can be used at the point of care. This has overcome some of the deficiencies of nucleic acid-based diagnostic tests and has made on-site diagnosis possible.17
Differential Diagnosis
The differential diagnosis for OrfV includes acute febrile neutrophilic dermatosis, erysipeloid and milker’s nodules.4 Acute febrile neutrophilic dermatosis, also known as Sweet disease, is a reactive process characterized by sudden onset tender, erythematous to violaceous papules that coalesce to form plaques. Erysipeloid is a sudden-onset bacterial infection of traumatized skin caused by Erysipelothrix rhusiopathiae. Milker’s nodules are another zoonotic infection caused by Parapoxvirus. They present similarly as localized, cutaneous nodules. OrfV also may mimic malignant neoplasms.
Pathogenesis
The OrfV confers infectivity through interferon resistance genes as well as Bcl-2 protein and cell cycle inhibitor genes. OrfV also exploits signal transduction pathways of the ubiquitin-proteasome system, which bypasses the intracellular signal transduction and CD8+ T-cell activation, thus shielding virus particles as they are matured and released from host cells.18
One study analyzed the genomic DNA of OrfV strains from the lips of 3- to 4-month-old goats in farms near Shihezi, Xinjiang, between June 2012 and August 2013. The authors found that the antigenic genes B2L and F1L were relatively conservative previously described isolates in the literature. At amino acid level, the identity was 88.6% to 97.9% and 86.7% to 97.4%, respectively.19
Currently, the main virulence genes found on the OrfV genome are VIR, vIL-10, GIF and VEGF. They are located at inverted repeats of genome terminals and play important roles in OrfV infection and pathogenesis. The virulence genes VIR and GIF also showed homology at the nucleotide and the amino acid level. However, the VEGF gene showed large variations, particularly at amino acid sequence level. As a result, this locus confers the most virulence for the OrfV.19
One group investigated an Orf outbreak in a flock of sheep at the Central Institute for Research on Goats in Makhdoom, India. On comparison of nucleotide and amino acid sequences, a unique 126S residue was observed in the Indian sheep, indicating that completely new strain exists in India.20
Management
At present, there are no effective antiviral treatments available for OrfV, and rapid diagnosis is therefore critical for effective control of the disease. Infections with OrfV (as with all Parapoxvirus) do not confer lifelong immunity. However, vaccines for primary prevention do exist. The DNA vaccine pcDNA3.1-ORFV011/ORFV059 expressing ORFV011 and ORFV059 chemeric-proteins were found effective in some goats in China.21
Vaccination with attenuated OrfV is the most common method to prevent and control the disease. It reduces the infection rate to a certain extent. However, there are recent reports showing that the vaccination with the attenuated virus cannot provide effective protection, suggesting that the OrfV epidemic strains might have been changed genetically under the current immune pressure.
One study revealed that RNA interference (RNAi) targeting of the OrfV DNA polymerase gene is potentially useful for therapeutic applications. Three small interfering RNA (siRNA) — siRNA704, siRNA1017 and siRNA1388 — prepared by in vitro transcription had reduced virus titers by 59- to 199-fold and reduced the level of viral replication by 73% to 89%.22 One group reported resolution with doxycycline.
Patient Management
Upon further questioning, the patient admitted to having been in contact with a sheep a few days prior to the development of the lesion. He was informed of the diagnosis and wound care with silver nitrate and fucidic acid cream (topical antibacterial) was started. At the 3-week follow-up, the lesion was healing with regression of the swelling and erythema.
Conclusion
OrfV is a double-stranded DNA virus that belongs to the Parapoxvirus genus. In humans, the disease usually presents as a painful nodule on the dorsal side of the fingers or hands that regresses, sometimes appearing like a bacterial infection or neoplasm. Histological analysis demonstrates balloon degeneration in the epidermis, lymphocytes, neutrophils and abundant eosinophils. At present, there are no effective antiviral treatments available for OrfV. Vaccination with attenuated OrfV is the most common method to prevent and control the disease.
Dr. Kallini is with Saint Louis University in St. Louis, MO.
Dr. Ehrsam is in private practice dermatology in Lille, France.
Dr. Khachemoune, the Section Editor of Derm DX, is with the Department of Dermatology at the State University of New York Downstate and Veterans Affairs Medical Center, both in Brooklyn, NY.
Disclosure: The authors report no relevant financial relationships.
References
1. Zhang K, Liu Y, Kong H, Shang Y, Liu X. Human infection with Orf virus from goats in China, 2012. Vector Borne Zoonotic Dis. 2014;14(5):365-367.
2. Giangaspero M, Bonfini B, Orusa R, Savini G, Osawa T, Harasawa R. Epidemiological survey for Toxoplasma gondii, Chlamydia psittaci var. ovis, Mycobacterium paratuberculosis, Coxiella burnetii, Brucella spp., leptospirosis and Orf virus among sheep from northern districts of Japan.
J Vet Med Sci. 2013;75(5):679-684.
3. Centers for Disease Control and Prevention. Human Orf virus infection from household exposures - United States, 2009-2011. MMWR Morb Mortal Wkly Rep. 2012;61(14):245-248.
4. Hawayek LH, Rubeiz N. Orf. Medscape. May 28, 2013. https://emedicine.medscape.com/article/1133450-overview. Accessed February 19, 2015.
5. Kitchen M, Müller H, Zobl A, Windisch A, Romani N, Huemer H. ORF virus infection in a hunter in Western Austria, presumably transmitted by game. Acta Derm Venereol. 2014;94(2):212-214.
6. Turan E, Yesilova Y, Ucmak D. A case of orf (ecthyma contagiosum) with multiple lesions. J Pak Med Assoc. 2013;63(6):786-787.
7. Gao F, Yuan H, Ling H, et al. An outbreak of human orf disease caused by introduced black goats. Zhonghua Liu Xing Bing Xue Za Zhi. 2011;32(9):905-907.
8. Veraldi S, Nazzaro G, Vaira F, Cuka E. Presentation of orf (ecthyma contagiosum) after sheep slaughtering for religious feasts. Infection. 2014;42(4):767-769.
9. Nougairede A, Fossati C, Salez N, et al. Sheep-to-human transmission of Orf virus during Eid al-Adha religious practices, France. Emerg Infect Dis. 2013;19(1):102-105.
10. Turk BG, Senturk B, Dereli T, Yaman B. A rare human-to-human transmission of orf. Int J Dermatol. 2014;53(1):e63-65.
11. Midilli K, Erkiliç A, Kuskucu M, et al. Nosocomial outbreak of disseminated orf infection in a burn unit, Gaziantep, Turkey, October to December 2012. Euro Surveill. 2013;18(11):20425.
12. de Sant’Ana FJ, Leal FA, Rabelo RE, et al. Coinfection by Vaccinia virus and an Orf virus-like parapoxvirus in an outbreak of vesicular disease in dairy cows in midwestern Brazil. J Vet Diagn Invest. 2013;25(2):267-272.
13. de Oliveira CH, Assis FL, Neto JD, et al. Multifocal cutaneous ORF virus infection in goats in the Amazon region, Brazil. Vector Borne Zoonotic Dis. 2012;12(4):336-340.
14. Lieu TJ, Park AN, Ahmed AM, Blanco GM, Luby JP. PHOTO QUIZ. A generalized eruption in a rancher. Clin Infect Dis. 2013;56(11):1613, 1675-1676.
15. Zhao H, Wilkins K, Damon IK, Li Y. Specific qPCR assays for the detection of orf virus, pseudocowpox virus and bovine papular stomatitis virus. J Virol Methods. 2013;194(1-2):229-234.
16. Venkatesan G, Bhanuprakash V, Balamurugan V, et al. Rapid detection and quantification of Orf virus from infected scab materials of sheep and goats. Acta Virol. 2012;56(1):81-83.
17. Li J, Song D, He W, et al. Rapid detection of orf virus by loop-mediated isothermal amplification based on the DNA polymerase gene. Arch Virol. 2013;158(4):793-798.
18. Yu YZ, Tong CY, Song BF, et al. Molecular mechanism of ORFV intervention strategies based on the UPS of host cell: a review. Bing Du Xue Bao. 2013;29(6):662-666.
19. Yang H, Meng Q, Qiao J, et al. Detection of genetic variations in Orf virus isolates epidemic in Xinjiang China. J Basic Microbiol. 2014;54(11):1273-1278.
20. Kumar N, Wadhwa A, Chaubey KK, et al. Isolation and phylogenetic analysis of an orf virus from sheep in Makhdoom, India. Virus Genes. 2014;48(2):312-319.
21. Zhao K, He W, Gao W, et al. Orf virus DNA vaccines expressing ORFV 011 and ORFV 059 chimeric protein enhances immunogenicity.
Virol J. 2011;8:562.
22. Wang G, He W, Song D, et al. In vitro RNA interference targeting the DNA polymerase gene inhibits orf virus replication in primary ovine fetal turbinate cells. Arch Virol. 2014;159(5):915-920.

Figure 1.
A 32-year-old man presented with a lesion on the dorsum of the left index finger that appeared 2 weeks prior to his presentation to the clinic. The lesion grew in size from a pinpoint papule to its current size. On physical examination, there was a weeping yellowish nodule overlying an erythematous base on the inner dorsal aspect of the left index finger at the metacarpal-phalangeal joint level. Overlying this nodule was a 2.2 cm x 2.1 cm ulcer (Figure).
What is Your Diagnosis?
Diagnosis: ORF Virus
Orf virus (OrfV), also known as ecthyma contagiosum, is a double-stranded DNA virus that belongs to the Parapoxvirus genus.1 In regards to epidemiology, antibodies against OrfV were reported in 3 flocks from Hokkaido and Iwate prefectures in Japan (2.57% of all sheep tested in northern Japan). The 6 positive animals were all Suffolk ewes of 5 to 7 years of age.2
Clinical Presentation
OrfV usually infects sheep and goat hosts, resulting in a zoonotic infection characterized by acute, highly vascularized cutaneous pustular lesions.
In humans, the disease usually presents as a painful nodule on the dorsal side of the fingers or hands (Figure). This regresses spontaneously without scar formation within 2 months. It has been reported in children after visiting petting zoos and livestock fairs.3 Human infection is rare. OrfV infection usually goes through 6 stages. Each stage usually lasts about 1 week. The stages are summarized in the Table.4

OrfV is often transmitted to humans by direct contact with infected animals. One hunter developed an OrfV lesion on the finger, which he acquired 3 weeks previously while he was handling a chamois carcass.5 A 42-year-old man presented with multiple nodular lesions on his right wrist after incurring an injury during ovine slaughter.6 There was also a reported outbreak among handlers of black goats in China.7 One article described a mother and son in the Gansu province of China who were infected with OrfV.1
Some cases of OrfV have been reported during religious practices. A 34-year-old Muslim man from Tunisia acquired OrfV infection on his left hand after he handled lamb meat during the Feast of Sacrifice. A 57-year-old Jewish man acquired OrfV on his left finger after the ritual of declaring lamb meat kosher.8 This virus also occurred in 5 individuals in France during the Eid-al-Adha practice.9
The transmission of OrfV from human to human is extremely rare. Only 4 cases have been described in the literature: a nurse who had changed the dressings of an infected patient, 2 cases of a child from an infected mother and a woman who contracted lesions on her cheek from her husband, a farmer.10 The first reported outbreak of a nosocomial OrfV infection occurred from October to December 2012 in a hospital burn unit in Gaziantep, Turkey; 13 patients became infected.11
Another report described an outbreak in Brazil in which a co-infection with Orf and vaccinia virus occurred in cows. The cows exhibited painful erythematous papules and vesicles in the teats for up to 3 weeks. Two people milking the affected cows developed the same painful lesions in 4 to 7 days; these later ulcerated and scabbed.12 The same co-infection occurred in goats in Brazil.13
Pathology
Histological analysis demonstrates balloon degeneration in the epidermis. Lymphocytes, neutrophils and abundant eosinophils are signs of most cutaneous viral infection. Indirect immunofluorescence may show anti-orf immunoglobulin (Ig) G earlier in the course, followed by both anti-orf IgG and IgM during convalescence.14
Diagnosis is made by Parapoxvirus RNA polymerase gene sequences, which can specifically detect Orf and other species in this genus.15 One group found that diagnosis from scabs of sheep and goats via counterimmunoelectrophoresis, conventional PCR, and rt-PCR was positive in 21.4%, 51.4% and 92.9%, respectively. This means that rt-PCR is the most sensitive tool in the diagnosis of OrfV. Furthermore, the rt-PCR is simpler and quicker compared to conventional PCR, which requires 2 rounds of PCR amplification.16
A novel technique known as flexible loop-mediated isothermal amplification (LAMP) can rapidly detect OrfV with high specificity and sensitivity. In contrast to PCR, in which the reaction is carried out with a series of alternating temperature steps, isothermal amplification is carried out at a single temperature, and does not require a thermal cycler. As a result, LAMP is a simple screening assay that can be used at the point of care. This has overcome some of the deficiencies of nucleic acid-based diagnostic tests and has made on-site diagnosis possible.17
Differential Diagnosis
The differential diagnosis for OrfV includes acute febrile neutrophilic dermatosis, erysipeloid and milker’s nodules.4 Acute febrile neutrophilic dermatosis, also known as Sweet disease, is a reactive process characterized by sudden onset tender, erythematous to violaceous papules that coalesce to form plaques. Erysipeloid is a sudden-onset bacterial infection of traumatized skin caused by Erysipelothrix rhusiopathiae. Milker’s nodules are another zoonotic infection caused by Parapoxvirus. They present similarly as localized, cutaneous nodules. OrfV also may mimic malignant neoplasms.
Pathogenesis
The OrfV confers infectivity through interferon resistance genes as well as Bcl-2 protein and cell cycle inhibitor genes. OrfV also exploits signal transduction pathways of the ubiquitin-proteasome system, which bypasses the intracellular signal transduction and CD8+ T-cell activation, thus shielding virus particles as they are matured and released from host cells.18
One study analyzed the genomic DNA of OrfV strains from the lips of 3- to 4-month-old goats in farms near Shihezi, Xinjiang, between June 2012 and August 2013. The authors found that the antigenic genes B2L and F1L were relatively conservative previously described isolates in the literature. At amino acid level, the identity was 88.6% to 97.9% and 86.7% to 97.4%, respectively.19
Currently, the main virulence genes found on the OrfV genome are VIR, vIL-10, GIF and VEGF. They are located at inverted repeats of genome terminals and play important roles in OrfV infection and pathogenesis. The virulence genes VIR and GIF also showed homology at the nucleotide and the amino acid level. However, the VEGF gene showed large variations, particularly at amino acid sequence level. As a result, this locus confers the most virulence for the OrfV.19
One group investigated an Orf outbreak in a flock of sheep at the Central Institute for Research on Goats in Makhdoom, India. On comparison of nucleotide and amino acid sequences, a unique 126S residue was observed in the Indian sheep, indicating that completely new strain exists in India.20
Management
At present, there are no effective antiviral treatments available for OrfV, and rapid diagnosis is therefore critical for effective control of the disease. Infections with OrfV (as with all Parapoxvirus) do not confer lifelong immunity. However, vaccines for primary prevention do exist. The DNA vaccine pcDNA3.1-ORFV011/ORFV059 expressing ORFV011 and ORFV059 chemeric-proteins were found effective in some goats in China.21
Vaccination with attenuated OrfV is the most common method to prevent and control the disease. It reduces the infection rate to a certain extent. However, there are recent reports showing that the vaccination with the attenuated virus cannot provide effective protection, suggesting that the OrfV epidemic strains might have been changed genetically under the current immune pressure.
One study revealed that RNA interference (RNAi) targeting of the OrfV DNA polymerase gene is potentially useful for therapeutic applications. Three small interfering RNA (siRNA) — siRNA704, siRNA1017 and siRNA1388 — prepared by in vitro transcription had reduced virus titers by 59- to 199-fold and reduced the level of viral replication by 73% to 89%.22 One group reported resolution with doxycycline.
Patient Management
Upon further questioning, the patient admitted to having been in contact with a sheep a few days prior to the development of the lesion. He was informed of the diagnosis and wound care with silver nitrate and fucidic acid cream (topical antibacterial) was started. At the 3-week follow-up, the lesion was healing with regression of the swelling and erythema.
Conclusion
OrfV is a double-stranded DNA virus that belongs to the Parapoxvirus genus. In humans, the disease usually presents as a painful nodule on the dorsal side of the fingers or hands that regresses, sometimes appearing like a bacterial infection or neoplasm. Histological analysis demonstrates balloon degeneration in the epidermis, lymphocytes, neutrophils and abundant eosinophils. At present, there are no effective antiviral treatments available for OrfV. Vaccination with attenuated OrfV is the most common method to prevent and control the disease.
Dr. Kallini is with Saint Louis University in St. Louis, MO.
Dr. Ehrsam is in private practice dermatology in Lille, France.
Dr. Khachemoune, the Section Editor of Derm DX, is with the Department of Dermatology at the State University of New York Downstate and Veterans Affairs Medical Center, both in Brooklyn, NY.
Disclosure: The authors report no relevant financial relationships.
References
1. Zhang K, Liu Y, Kong H, Shang Y, Liu X. Human infection with Orf virus from goats in China, 2012. Vector Borne Zoonotic Dis. 2014;14(5):365-367.
2. Giangaspero M, Bonfini B, Orusa R, Savini G, Osawa T, Harasawa R. Epidemiological survey for Toxoplasma gondii, Chlamydia psittaci var. ovis, Mycobacterium paratuberculosis, Coxiella burnetii, Brucella spp., leptospirosis and Orf virus among sheep from northern districts of Japan.
J Vet Med Sci. 2013;75(5):679-684.
3. Centers for Disease Control and Prevention. Human Orf virus infection from household exposures - United States, 2009-2011. MMWR Morb Mortal Wkly Rep. 2012;61(14):245-248.
4. Hawayek LH, Rubeiz N. Orf. Medscape. May 28, 2013. https://emedicine.medscape.com/article/1133450-overview. Accessed February 19, 2015.
5. Kitchen M, Müller H, Zobl A, Windisch A, Romani N, Huemer H. ORF virus infection in a hunter in Western Austria, presumably transmitted by game. Acta Derm Venereol. 2014;94(2):212-214.
6. Turan E, Yesilova Y, Ucmak D. A case of orf (ecthyma contagiosum) with multiple lesions. J Pak Med Assoc. 2013;63(6):786-787.
7. Gao F, Yuan H, Ling H, et al. An outbreak of human orf disease caused by introduced black goats. Zhonghua Liu Xing Bing Xue Za Zhi. 2011;32(9):905-907.
8. Veraldi S, Nazzaro G, Vaira F, Cuka E. Presentation of orf (ecthyma contagiosum) after sheep slaughtering for religious feasts. Infection. 2014;42(4):767-769.
9. Nougairede A, Fossati C, Salez N, et al. Sheep-to-human transmission of Orf virus during Eid al-Adha religious practices, France. Emerg Infect Dis. 2013;19(1):102-105.
10. Turk BG, Senturk B, Dereli T, Yaman B. A rare human-to-human transmission of orf. Int J Dermatol. 2014;53(1):e63-65.
11. Midilli K, Erkiliç A, Kuskucu M, et al. Nosocomial outbreak of disseminated orf infection in a burn unit, Gaziantep, Turkey, October to December 2012. Euro Surveill. 2013;18(11):20425.
12. de Sant’Ana FJ, Leal FA, Rabelo RE, et al. Coinfection by Vaccinia virus and an Orf virus-like parapoxvirus in an outbreak of vesicular disease in dairy cows in midwestern Brazil. J Vet Diagn Invest. 2013;25(2):267-272.
13. de Oliveira CH, Assis FL, Neto JD, et al. Multifocal cutaneous ORF virus infection in goats in the Amazon region, Brazil. Vector Borne Zoonotic Dis. 2012;12(4):336-340.
14. Lieu TJ, Park AN, Ahmed AM, Blanco GM, Luby JP. PHOTO QUIZ. A generalized eruption in a rancher. Clin Infect Dis. 2013;56(11):1613, 1675-1676.
15. Zhao H, Wilkins K, Damon IK, Li Y. Specific qPCR assays for the detection of orf virus, pseudocowpox virus and bovine papular stomatitis virus. J Virol Methods. 2013;194(1-2):229-234.
16. Venkatesan G, Bhanuprakash V, Balamurugan V, et al. Rapid detection and quantification of Orf virus from infected scab materials of sheep and goats. Acta Virol. 2012;56(1):81-83.
17. Li J, Song D, He W, et al. Rapid detection of orf virus by loop-mediated isothermal amplification based on the DNA polymerase gene. Arch Virol. 2013;158(4):793-798.
18. Yu YZ, Tong CY, Song BF, et al. Molecular mechanism of ORFV intervention strategies based on the UPS of host cell: a review. Bing Du Xue Bao. 2013;29(6):662-666.
19. Yang H, Meng Q, Qiao J, et al. Detection of genetic variations in Orf virus isolates epidemic in Xinjiang China. J Basic Microbiol. 2014;54(11):1273-1278.
20. Kumar N, Wadhwa A, Chaubey KK, et al. Isolation and phylogenetic analysis of an orf virus from sheep in Makhdoom, India. Virus Genes. 2014;48(2):312-319.
21. Zhao K, He W, Gao W, et al. Orf virus DNA vaccines expressing ORFV 011 and ORFV 059 chimeric protein enhances immunogenicity.
Virol J. 2011;8:562.
22. Wang G, He W, Song D, et al. In vitro RNA interference targeting the DNA polymerase gene inhibits orf virus replication in primary ovine fetal turbinate cells. Arch Virol. 2014;159(5):915-920.

Figure 1.
A 32-year-old man presented with a lesion on the dorsum of the left index finger that appeared 2 weeks prior to his presentation to the clinic. The lesion grew in size from a pinpoint papule to its current size. On physical examination, there was a weeping yellowish nodule overlying an erythematous base on the inner dorsal aspect of the left index finger at the metacarpal-phalangeal joint level. Overlying this nodule was a 2.2 cm x 2.1 cm ulcer (Figure).
What is Your Diagnosis?
,

Figure 1.
A 32-year-old man presented with a lesion on the dorsum of the left index finger that appeared 2 weeks prior to his presentation to the clinic. The lesion grew in size from a pinpoint papule to its current size. On physical examination, there was a weeping yellowish nodule overlying an erythematous base on the inner dorsal aspect of the left index finger at the metacarpal-phalangeal joint level. Overlying this nodule was a 2.2 cm x 2.1 cm ulcer (Figure).
What is Your Diagnosis?
To learn the answer, go to page 2
{{pagebreak}}
Diagnosis: ORF Virus
Orf virus (OrfV), also known as ecthyma contagiosum, is a double-stranded DNA virus that belongs to the Parapoxvirus genus.1 In regards to epidemiology, antibodies against OrfV were reported in 3 flocks from Hokkaido and Iwate prefectures in Japan (2.57% of all sheep tested in northern Japan). The 6 positive animals were all Suffolk ewes of 5 to 7 years of age.2
Clinical Presentation
OrfV usually infects sheep and goat hosts, resulting in a zoonotic infection characterized by acute, highly vascularized cutaneous pustular lesions.
In humans, the disease usually presents as a painful nodule on the dorsal side of the fingers or hands (Figure). This regresses spontaneously without scar formation within 2 months. It has been reported in children after visiting petting zoos and livestock fairs.3 Human infection is rare. OrfV infection usually goes through 6 stages. Each stage usually lasts about 1 week. The stages are summarized in the Table.4
OrfV is often transmitted to humans by direct contact with infected animals. One hunter developed an OrfV lesion on the finger, which he acquired 3 weeks previously while he was handling a chamois carcass.5 A 42-year-old man presented with multiple nodular lesions on his right wrist after incurring an injury during ovine slaughter.6 There was also a reported outbreak among handlers of black goats in China.7 One article described a mother and son in the Gansu province of China who were infected with OrfV.1
Some cases of OrfV have been reported during religious practices. A 34-year-old Muslim man from Tunisia acquired OrfV infection on his left hand after he handled lamb meat during the Feast of Sacrifice. A 57-year-old Jewish man acquired OrfV on his left finger after the ritual of declaring lamb meat kosher.8 This virus also occurred in 5 individuals in France during the Eid-al-Adha practice.9
The transmission of OrfV from human to human is extremely rare. Only 4 cases have been described in the literature: a nurse who had changed the dressings of an infected patient, 2 cases of a child from an infected mother and a woman who contracted lesions on her cheek from her husband, a farmer.10 The first reported outbreak of a nosocomial OrfV infection occurred from October to December 2012 in a hospital burn unit in Gaziantep, Turkey; 13 patients became infected.11
Another report described an outbreak in Brazil in which a co-infection with Orf and vaccinia virus occurred in cows. The cows exhibited painful erythematous papules and vesicles in the teats for up to 3 weeks. Two people milking the affected cows developed the same painful lesions in 4 to 7 days; these later ulcerated and scabbed.12 The same co-infection occurred in goats in Brazil.13
Pathology
Histological analysis demonstrates balloon degeneration in the epidermis. Lymphocytes, neutrophils and abundant eosinophils are signs of most cutaneous viral infection. Indirect immunofluorescence may show anti-orf immunoglobulin (Ig) G earlier in the course, followed by both anti-orf IgG and IgM during convalescence.14
Diagnosis is made by Parapoxvirus RNA polymerase gene sequences, which can specifically detect Orf and other species in this genus.15 One group found that diagnosis from scabs of sheep and goats via counterimmunoelectrophoresis, conventional PCR, and rt-PCR was positive in 21.4%, 51.4% and 92.9%, respectively. This means that rt-PCR is the most sensitive tool in the diagnosis of OrfV. Furthermore, the rt-PCR is simpler and quicker compared to conventional PCR, which requires 2 rounds of PCR amplification.16
A novel technique known as flexible loop-mediated isothermal amplification (LAMP) can rapidly detect OrfV with high specificity and sensitivity. In contrast to PCR, in which the reaction is carried out with a series of alternating temperature steps, isothermal amplification is carried out at a single temperature, and does not require a thermal cycler. As a result, LAMP is a simple screening assay that can be used at the point of care. This has overcome some of the deficiencies of nucleic acid-based diagnostic tests and has made on-site diagnosis possible.17
Differential Diagnosis
The differential diagnosis for OrfV includes acute febrile neutrophilic dermatosis, erysipeloid and milker’s nodules.4 Acute febrile neutrophilic dermatosis, also known as Sweet disease, is a reactive process characterized by sudden onset tender, erythematous to violaceous papules that coalesce to form plaques. Erysipeloid is a sudden-onset bacterial infection of traumatized skin caused by Erysipelothrix rhusiopathiae. Milker’s nodules are another zoonotic infection caused by Parapoxvirus. They present similarly as localized, cutaneous nodules. OrfV also may mimic malignant neoplasms.
Pathogenesis
The OrfV confers infectivity through interferon resistance genes as well as Bcl-2 protein and cell cycle inhibitor genes. OrfV also exploits signal transduction pathways of the ubiquitin-proteasome system, which bypasses the intracellular signal transduction and CD8+ T-cell activation, thus shielding virus particles as they are matured and released from host cells.18
One study analyzed the genomic DNA of OrfV strains from the lips of 3- to 4-month-old goats in farms near Shihezi, Xinjiang, between June 2012 and August 2013. The authors found that the antigenic genes B2L and F1L were relatively conservative previously described isolates in the literature. At amino acid level, the identity was 88.6% to 97.9% and 86.7% to 97.4%, respectively.19
Currently, the main virulence genes found on the OrfV genome are VIR, vIL-10, GIF and VEGF. They are located at inverted repeats of genome terminals and play important roles in OrfV infection and pathogenesis. The virulence genes VIR and GIF also showed homology at the nucleotide and the amino acid level. However, the VEGF gene showed large variations, particularly at amino acid sequence level. As a result, this locus confers the most virulence for the OrfV.19
One group investigated an Orf outbreak in a flock of sheep at the Central Institute for Research on Goats in Makhdoom, India. On comparison of nucleotide and amino acid sequences, a unique 126S residue was observed in the Indian sheep, indicating that completely new strain exists in India.20
Management
At present, there are no effective antiviral treatments available for OrfV, and rapid diagnosis is therefore critical for effective control of the disease. Infections with OrfV (as with all Parapoxvirus) do not confer lifelong immunity. However, vaccines for primary prevention do exist. The DNA vaccine pcDNA3.1-ORFV011/ORFV059 expressing ORFV011 and ORFV059 chemeric-proteins were found effective in some goats in China.21
Vaccination with attenuated OrfV is the most common method to prevent and control the disease. It reduces the infection rate to a certain extent. However, there are recent reports showing that the vaccination with the attenuated virus cannot provide effective protection, suggesting that the OrfV epidemic strains might have been changed genetically under the current immune pressure.
One study revealed that RNA interference (RNAi) targeting of the OrfV DNA polymerase gene is potentially useful for therapeutic applications. Three small interfering RNA (siRNA) — siRNA704, siRNA1017 and siRNA1388 — prepared by in vitro transcription had reduced virus titers by 59- to 199-fold and reduced the level of viral replication by 73% to 89%.22 One group reported resolution with doxycycline.
Patient Management
Upon further questioning, the patient admitted to having been in contact with a sheep a few days prior to the development of the lesion. He was informed of the diagnosis and wound care with silver nitrate and fucidic acid cream (topical antibacterial) was started. At the 3-week follow-up, the lesion was healing with regression of the swelling and erythema.
Conclusion
OrfV is a double-stranded DNA virus that belongs to the Parapoxvirus genus. In humans, the disease usually presents as a painful nodule on the dorsal side of the fingers or hands that regresses, sometimes appearing like a bacterial infection or neoplasm. Histological analysis demonstrates balloon degeneration in the epidermis, lymphocytes, neutrophils and abundant eosinophils. At present, there are no effective antiviral treatments available for OrfV. Vaccination with attenuated OrfV is the most common method to prevent and control the disease.
Dr. Kallini is with Saint Louis University in St. Louis, MO.
Dr. Ehrsam is in private practice dermatology in Lille, France.
Dr. Khachemoune, the Section Editor of Derm DX, is with the Department of Dermatology at the State University of New York Downstate and Veterans Affairs Medical Center, both in Brooklyn, NY.
Disclosure: The authors report no relevant financial relationships.
References
1. Zhang K, Liu Y, Kong H, Shang Y, Liu X. Human infection with Orf virus from goats in China, 2012. Vector Borne Zoonotic Dis. 2014;14(5):365-367.
2. Giangaspero M, Bonfini B, Orusa R, Savini G, Osawa T, Harasawa R. Epidemiological survey for Toxoplasma gondii, Chlamydia psittaci var. ovis, Mycobacterium paratuberculosis, Coxiella burnetii, Brucella spp., leptospirosis and Orf virus among sheep from northern districts of Japan.
J Vet Med Sci. 2013;75(5):679-684.
3. Centers for Disease Control and Prevention. Human Orf virus infection from household exposures - United States, 2009-2011. MMWR Morb Mortal Wkly Rep. 2012;61(14):245-248.
4. Hawayek LH, Rubeiz N. Orf. Medscape. May 28, 2013. https://emedicine.medscape.com/article/1133450-overview. Accessed February 19, 2015.
5. Kitchen M, Müller H, Zobl A, Windisch A, Romani N, Huemer H. ORF virus infection in a hunter in Western Austria, presumably transmitted by game. Acta Derm Venereol. 2014;94(2):212-214.
6. Turan E, Yesilova Y, Ucmak D. A case of orf (ecthyma contagiosum) with multiple lesions. J Pak Med Assoc. 2013;63(6):786-787.
7. Gao F, Yuan H, Ling H, et al. An outbreak of human orf disease caused by introduced black goats. Zhonghua Liu Xing Bing Xue Za Zhi. 2011;32(9):905-907.
8. Veraldi S, Nazzaro G, Vaira F, Cuka E. Presentation of orf (ecthyma contagiosum) after sheep slaughtering for religious feasts. Infection. 2014;42(4):767-769.
9. Nougairede A, Fossati C, Salez N, et al. Sheep-to-human transmission of Orf virus during Eid al-Adha religious practices, France. Emerg Infect Dis. 2013;19(1):102-105.
10. Turk BG, Senturk B, Dereli T, Yaman B. A rare human-to-human transmission of orf. Int J Dermatol. 2014;53(1):e63-65.
11. Midilli K, Erkiliç A, Kuskucu M, et al. Nosocomial outbreak of disseminated orf infection in a burn unit, Gaziantep, Turkey, October to December 2012. Euro Surveill. 2013;18(11):20425.
12. de Sant’Ana FJ, Leal FA, Rabelo RE, et al. Coinfection by Vaccinia virus and an Orf virus-like parapoxvirus in an outbreak of vesicular disease in dairy cows in midwestern Brazil. J Vet Diagn Invest. 2013;25(2):267-272.
13. de Oliveira CH, Assis FL, Neto JD, et al. Multifocal cutaneous ORF virus infection in goats in the Amazon region, Brazil. Vector Borne Zoonotic Dis. 2012;12(4):336-340.
14. Lieu TJ, Park AN, Ahmed AM, Blanco GM, Luby JP. PHOTO QUIZ. A generalized eruption in a rancher. Clin Infect Dis. 2013;56(11):1613, 1675-1676.
15. Zhao H, Wilkins K, Damon IK, Li Y. Specific qPCR assays for the detection of orf virus, pseudocowpox virus and bovine papular stomatitis virus. J Virol Methods. 2013;194(1-2):229-234.
16. Venkatesan G, Bhanuprakash V, Balamurugan V, et al. Rapid detection and quantification of Orf virus from infected scab materials of sheep and goats. Acta Virol. 2012;56(1):81-83.
17. Li J, Song D, He W, et al. Rapid detection of orf virus by loop-mediated isothermal amplification based on the DNA polymerase gene. Arch Virol. 2013;158(4):793-798.
18. Yu YZ, Tong CY, Song BF, et al. Molecular mechanism of ORFV intervention strategies based on the UPS of host cell: a review. Bing Du Xue Bao. 2013;29(6):662-666.
19. Yang H, Meng Q, Qiao J, et al. Detection of genetic variations in Orf virus isolates epidemic in Xinjiang China. J Basic Microbiol. 2014;54(11):1273-1278.
20. Kumar N, Wadhwa A, Chaubey KK, et al. Isolation and phylogenetic analysis of an orf virus from sheep in Makhdoom, India. Virus Genes. 2014;48(2):312-319.
21. Zhao K, He W, Gao W, et al. Orf virus DNA vaccines expressing ORFV 011 and ORFV 059 chimeric protein enhances immunogenicity.
Virol J. 2011;8:562.
22. Wang G, He W, Song D, et al. In vitro RNA interference targeting the DNA polymerase gene inhibits orf virus replication in primary ovine fetal turbinate cells. Arch Virol. 2014;159(5):915-920.

Figure 1.
A 32-year-old man presented with a lesion on the dorsum of the left index finger that appeared 2 weeks prior to his presentation to the clinic. The lesion grew in size from a pinpoint papule to its current size. On physical examination, there was a weeping yellowish nodule overlying an erythematous base on the inner dorsal aspect of the left index finger at the metacarpal-phalangeal joint level. Overlying this nodule was a 2.2 cm x 2.1 cm ulcer (Figure).
What is Your Diagnosis?
Diagnosis: ORF Virus
Orf virus (OrfV), also known as ecthyma contagiosum, is a double-stranded DNA virus that belongs to the Parapoxvirus genus.1 In regards to epidemiology, antibodies against OrfV were reported in 3 flocks from Hokkaido and Iwate prefectures in Japan (2.57% of all sheep tested in northern Japan). The 6 positive animals were all Suffolk ewes of 5 to 7 years of age.2
Clinical Presentation
OrfV usually infects sheep and goat hosts, resulting in a zoonotic infection characterized by acute, highly vascularized cutaneous pustular lesions.
In humans, the disease usually presents as a painful nodule on the dorsal side of the fingers or hands (Figure). This regresses spontaneously without scar formation within 2 months. It has been reported in children after visiting petting zoos and livestock fairs.3 Human infection is rare. OrfV infection usually goes through 6 stages. Each stage usually lasts about 1 week. The stages are summarized in the Table.4

OrfV is often transmitted to humans by direct contact with infected animals. One hunter developed an OrfV lesion on the finger, which he acquired 3 weeks previously while he was handling a chamois carcass.5 A 42-year-old man presented with multiple nodular lesions on his right wrist after incurring an injury during ovine slaughter.6 There was also a reported outbreak among handlers of black goats in China.7 One article described a mother and son in the Gansu province of China who were infected with OrfV.1
Some cases of OrfV have been reported during religious practices. A 34-year-old Muslim man from Tunisia acquired OrfV infection on his left hand after he handled lamb meat during the Feast of Sacrifice. A 57-year-old Jewish man acquired OrfV on his left finger after the ritual of declaring lamb meat kosher.8 This virus also occurred in 5 individuals in France during the Eid-al-Adha practice.9
The transmission of OrfV from human to human is extremely rare. Only 4 cases have been described in the literature: a nurse who had changed the dressings of an infected patient, 2 cases of a child from an infected mother and a woman who contracted lesions on her cheek from her husband, a farmer.10 The first reported outbreak of a nosocomial OrfV infection occurred from October to December 2012 in a hospital burn unit in Gaziantep, Turkey; 13 patients became infected.11
Another report described an outbreak in Brazil in which a co-infection with Orf and vaccinia virus occurred in cows. The cows exhibited painful erythematous papules and vesicles in the teats for up to 3 weeks. Two people milking the affected cows developed the same painful lesions in 4 to 7 days; these later ulcerated and scabbed.12 The same co-infection occurred in goats in Brazil.13
Pathology
Histological analysis demonstrates balloon degeneration in the epidermis. Lymphocytes, neutrophils and abundant eosinophils are signs of most cutaneous viral infection. Indirect immunofluorescence may show anti-orf immunoglobulin (Ig) G earlier in the course, followed by both anti-orf IgG and IgM during convalescence.14
Diagnosis is made by Parapoxvirus RNA polymerase gene sequences, which can specifically detect Orf and other species in this genus.15 One group found that diagnosis from scabs of sheep and goats via counterimmunoelectrophoresis, conventional PCR, and rt-PCR was positive in 21.4%, 51.4% and 92.9%, respectively. This means that rt-PCR is the most sensitive tool in the diagnosis of OrfV. Furthermore, the rt-PCR is simpler and quicker compared to conventional PCR, which requires 2 rounds of PCR amplification.16
A novel technique known as flexible loop-mediated isothermal amplification (LAMP) can rapidly detect OrfV with high specificity and sensitivity. In contrast to PCR, in which the reaction is carried out with a series of alternating temperature steps, isothermal amplification is carried out at a single temperature, and does not require a thermal cycler. As a result, LAMP is a simple screening assay that can be used at the point of care. This has overcome some of the deficiencies of nucleic acid-based diagnostic tests and has made on-site diagnosis possible.17
Differential Diagnosis
The differential diagnosis for OrfV includes acute febrile neutrophilic dermatosis, erysipeloid and milker’s nodules.4 Acute febrile neutrophilic dermatosis, also known as Sweet disease, is a reactive process characterized by sudden onset tender, erythematous to violaceous papules that coalesce to form plaques. Erysipeloid is a sudden-onset bacterial infection of traumatized skin caused by Erysipelothrix rhusiopathiae. Milker’s nodules are another zoonotic infection caused by Parapoxvirus. They present similarly as localized, cutaneous nodules. OrfV also may mimic malignant neoplasms.
Pathogenesis
The OrfV confers infectivity through interferon resistance genes as well as Bcl-2 protein and cell cycle inhibitor genes. OrfV also exploits signal transduction pathways of the ubiquitin-proteasome system, which bypasses the intracellular signal transduction and CD8+ T-cell activation, thus shielding virus particles as they are matured and released from host cells.18
One study analyzed the genomic DNA of OrfV strains from the lips of 3- to 4-month-old goats in farms near Shihezi, Xinjiang, between June 2012 and August 2013. The authors found that the antigenic genes B2L and F1L were relatively conservative previously described isolates in the literature. At amino acid level, the identity was 88.6% to 97.9% and 86.7% to 97.4%, respectively.19
Currently, the main virulence genes found on the OrfV genome are VIR, vIL-10, GIF and VEGF. They are located at inverted repeats of genome terminals and play important roles in OrfV infection and pathogenesis. The virulence genes VIR and GIF also showed homology at the nucleotide and the amino acid level. However, the VEGF gene showed large variations, particularly at amino acid sequence level. As a result, this locus confers the most virulence for the OrfV.19
One group investigated an Orf outbreak in a flock of sheep at the Central Institute for Research on Goats in Makhdoom, India. On comparison of nucleotide and amino acid sequences, a unique 126S residue was observed in the Indian sheep, indicating that completely new strain exists in India.20
Management
At present, there are no effective antiviral treatments available for OrfV, and rapid diagnosis is therefore critical for effective control of the disease. Infections with OrfV (as with all Parapoxvirus) do not confer lifelong immunity. However, vaccines for primary prevention do exist. The DNA vaccine pcDNA3.1-ORFV011/ORFV059 expressing ORFV011 and ORFV059 chemeric-proteins were found effective in some goats in China.21
Vaccination with attenuated OrfV is the most common method to prevent and control the disease. It reduces the infection rate to a certain extent. However, there are recent reports showing that the vaccination with the attenuated virus cannot provide effective protection, suggesting that the OrfV epidemic strains might have been changed genetically under the current immune pressure.
One study revealed that RNA interference (RNAi) targeting of the OrfV DNA polymerase gene is potentially useful for therapeutic applications. Three small interfering RNA (siRNA) — siRNA704, siRNA1017 and siRNA1388 — prepared by in vitro transcription had reduced virus titers by 59- to 199-fold and reduced the level of viral replication by 73% to 89%.22 One group reported resolution with doxycycline.
Patient Management
Upon further questioning, the patient admitted to having been in contact with a sheep a few days prior to the development of the lesion. He was informed of the diagnosis and wound care with silver nitrate and fucidic acid cream (topical antibacterial) was started. At the 3-week follow-up, the lesion was healing with regression of the swelling and erythema.
Conclusion
OrfV is a double-stranded DNA virus that belongs to the Parapoxvirus genus. In humans, the disease usually presents as a painful nodule on the dorsal side of the fingers or hands that regresses, sometimes appearing like a bacterial infection or neoplasm. Histological analysis demonstrates balloon degeneration in the epidermis, lymphocytes, neutrophils and abundant eosinophils. At present, there are no effective antiviral treatments available for OrfV. Vaccination with attenuated OrfV is the most common method to prevent and control the disease.
Dr. Kallini is with Saint Louis University in St. Louis, MO.
Dr. Ehrsam is in private practice dermatology in Lille, France.
Dr. Khachemoune, the Section Editor of Derm DX, is with the Department of Dermatology at the State University of New York Downstate and Veterans Affairs Medical Center, both in Brooklyn, NY.
Disclosure: The authors report no relevant financial relationships.
References
1. Zhang K, Liu Y, Kong H, Shang Y, Liu X. Human infection with Orf virus from goats in China, 2012. Vector Borne Zoonotic Dis. 2014;14(5):365-367.
2. Giangaspero M, Bonfini B, Orusa R, Savini G, Osawa T, Harasawa R. Epidemiological survey for Toxoplasma gondii, Chlamydia psittaci var. ovis, Mycobacterium paratuberculosis, Coxiella burnetii, Brucella spp., leptospirosis and Orf virus among sheep from northern districts of Japan.
J Vet Med Sci. 2013;75(5):679-684.
3. Centers for Disease Control and Prevention. Human Orf virus infection from household exposures - United States, 2009-2011. MMWR Morb Mortal Wkly Rep. 2012;61(14):245-248.
4. Hawayek LH, Rubeiz N. Orf. Medscape. May 28, 2013. https://emedicine.medscape.com/article/1133450-overview. Accessed February 19, 2015.
5. Kitchen M, Müller H, Zobl A, Windisch A, Romani N, Huemer H. ORF virus infection in a hunter in Western Austria, presumably transmitted by game. Acta Derm Venereol. 2014;94(2):212-214.
6. Turan E, Yesilova Y, Ucmak D. A case of orf (ecthyma contagiosum) with multiple lesions. J Pak Med Assoc. 2013;63(6):786-787.
7. Gao F, Yuan H, Ling H, et al. An outbreak of human orf disease caused by introduced black goats. Zhonghua Liu Xing Bing Xue Za Zhi. 2011;32(9):905-907.
8. Veraldi S, Nazzaro G, Vaira F, Cuka E. Presentation of orf (ecthyma contagiosum) after sheep slaughtering for religious feasts. Infection. 2014;42(4):767-769.
9. Nougairede A, Fossati C, Salez N, et al. Sheep-to-human transmission of Orf virus during Eid al-Adha religious practices, France. Emerg Infect Dis. 2013;19(1):102-105.
10. Turk BG, Senturk B, Dereli T, Yaman B. A rare human-to-human transmission of orf. Int J Dermatol. 2014;53(1):e63-65.
11. Midilli K, Erkiliç A, Kuskucu M, et al. Nosocomial outbreak of disseminated orf infection in a burn unit, Gaziantep, Turkey, October to December 2012. Euro Surveill. 2013;18(11):20425.
12. de Sant’Ana FJ, Leal FA, Rabelo RE, et al. Coinfection by Vaccinia virus and an Orf virus-like parapoxvirus in an outbreak of vesicular disease in dairy cows in midwestern Brazil. J Vet Diagn Invest. 2013;25(2):267-272.
13. de Oliveira CH, Assis FL, Neto JD, et al. Multifocal cutaneous ORF virus infection in goats in the Amazon region, Brazil. Vector Borne Zoonotic Dis. 2012;12(4):336-340.
14. Lieu TJ, Park AN, Ahmed AM, Blanco GM, Luby JP. PHOTO QUIZ. A generalized eruption in a rancher. Clin Infect Dis. 2013;56(11):1613, 1675-1676.
15. Zhao H, Wilkins K, Damon IK, Li Y. Specific qPCR assays for the detection of orf virus, pseudocowpox virus and bovine papular stomatitis virus. J Virol Methods. 2013;194(1-2):229-234.
16. Venkatesan G, Bhanuprakash V, Balamurugan V, et al. Rapid detection and quantification of Orf virus from infected scab materials of sheep and goats. Acta Virol. 2012;56(1):81-83.
17. Li J, Song D, He W, et al. Rapid detection of orf virus by loop-mediated isothermal amplification based on the DNA polymerase gene. Arch Virol. 2013;158(4):793-798.
18. Yu YZ, Tong CY, Song BF, et al. Molecular mechanism of ORFV intervention strategies based on the UPS of host cell: a review. Bing Du Xue Bao. 2013;29(6):662-666.
19. Yang H, Meng Q, Qiao J, et al. Detection of genetic variations in Orf virus isolates epidemic in Xinjiang China. J Basic Microbiol. 2014;54(11):1273-1278.
20. Kumar N, Wadhwa A, Chaubey KK, et al. Isolation and phylogenetic analysis of an orf virus from sheep in Makhdoom, India. Virus Genes. 2014;48(2):312-319.
21. Zhao K, He W, Gao W, et al. Orf virus DNA vaccines expressing ORFV 011 and ORFV 059 chimeric protein enhances immunogenicity.
Virol J. 2011;8:562.
22. Wang G, He W, Song D, et al. In vitro RNA interference targeting the DNA polymerase gene inhibits orf virus replication in primary ovine fetal turbinate cells. Arch Virol. 2014;159(5):915-920.
Diagnosis: ORF Virus
Orf virus (OrfV), also known as ecthyma contagiosum, is a double-stranded DNA virus that belongs to the Parapoxvirus genus.1 In regards to epidemiology, antibodies against OrfV were reported in 3 flocks from Hokkaido and Iwate prefectures in Japan (2.57% of all sheep tested in northern Japan). The 6 positive animals were all Suffolk ewes of 5 to 7 years of age.2
Clinical Presentation
OrfV usually infects sheep and goat hosts, resulting in a zoonotic infection characterized by acute, highly vascularized cutaneous pustular lesions.
In humans, the disease usually presents as a painful nodule on the dorsal side of the fingers or hands (Figure). This regresses spontaneously without scar formation within 2 months. It has been reported in children after visiting petting zoos and livestock fairs.3 Human infection is rare. OrfV infection usually goes through 6 stages. Each stage usually lasts about 1 week. The stages are summarized in the Table.4

OrfV is often transmitted to humans by direct contact with infected animals. One hunter developed an OrfV lesion on the finger, which he acquired 3 weeks previously while he was handling a chamois carcass.5 A 42-year-old man presented with multiple nodular lesions on his right wrist after incurring an injury during ovine slaughter.6 There was also a reported outbreak among handlers of black goats in China.7 One article described a mother and son in the Gansu province of China who were infected with OrfV.1
Some cases of OrfV have been reported during religious practices. A 34-year-old Muslim man from Tunisia acquired OrfV infection on his left hand after he handled lamb meat during the Feast of Sacrifice. A 57-year-old Jewish man acquired OrfV on his left finger after the ritual of declaring lamb meat kosher.8 This virus also occurred in 5 individuals in France during the Eid-al-Adha practice.9
The transmission of OrfV from human to human is extremely rare. Only 4 cases have been described in the literature: a nurse who had changed the dressings of an infected patient, 2 cases of a child from an infected mother and a woman who contracted lesions on her cheek from her husband, a farmer.10 The first reported outbreak of a nosocomial OrfV infection occurred from October to December 2012 in a hospital burn unit in Gaziantep, Turkey; 13 patients became infected.11
Another report described an outbreak in Brazil in which a co-infection with Orf and vaccinia virus occurred in cows. The cows exhibited painful erythematous papules and vesicles in the teats for up to 3 weeks. Two people milking the affected cows developed the same painful lesions in 4 to 7 days; these later ulcerated and scabbed.12 The same co-infection occurred in goats in Brazil.13
Pathology
Histological analysis demonstrates balloon degeneration in the epidermis. Lymphocytes, neutrophils and abundant eosinophils are signs of most cutaneous viral infection. Indirect immunofluorescence may show anti-orf immunoglobulin (Ig) G earlier in the course, followed by both anti-orf IgG and IgM during convalescence.14
Diagnosis is made by Parapoxvirus RNA polymerase gene sequences, which can specifically detect Orf and other species in this genus.15 One group found that diagnosis from scabs of sheep and goats via counterimmunoelectrophoresis, conventional PCR, and rt-PCR was positive in 21.4%, 51.4% and 92.9%, respectively. This means that rt-PCR is the most sensitive tool in the diagnosis of OrfV. Furthermore, the rt-PCR is simpler and quicker compared to conventional PCR, which requires 2 rounds of PCR amplification.16
A novel technique known as flexible loop-mediated isothermal amplification (LAMP) can rapidly detect OrfV with high specificity and sensitivity. In contrast to PCR, in which the reaction is carried out with a series of alternating temperature steps, isothermal amplification is carried out at a single temperature, and does not require a thermal cycler. As a result, LAMP is a simple screening assay that can be used at the point of care. This has overcome some of the deficiencies of nucleic acid-based diagnostic tests and has made on-site diagnosis possible.17
Differential Diagnosis
The differential diagnosis for OrfV includes acute febrile neutrophilic dermatosis, erysipeloid and milker’s nodules.4 Acute febrile neutrophilic dermatosis, also known as Sweet disease, is a reactive process characterized by sudden onset tender, erythematous to violaceous papules that coalesce to form plaques. Erysipeloid is a sudden-onset bacterial infection of traumatized skin caused by Erysipelothrix rhusiopathiae. Milker’s nodules are another zoonotic infection caused by Parapoxvirus. They present similarly as localized, cutaneous nodules. OrfV also may mimic malignant neoplasms.
Pathogenesis
The OrfV confers infectivity through interferon resistance genes as well as Bcl-2 protein and cell cycle inhibitor genes. OrfV also exploits signal transduction pathways of the ubiquitin-proteasome system, which bypasses the intracellular signal transduction and CD8+ T-cell activation, thus shielding virus particles as they are matured and released from host cells.18
One study analyzed the genomic DNA of OrfV strains from the lips of 3- to 4-month-old goats in farms near Shihezi, Xinjiang, between June 2012 and August 2013. The authors found that the antigenic genes B2L and F1L were relatively conservative previously described isolates in the literature. At amino acid level, the identity was 88.6% to 97.9% and 86.7% to 97.4%, respectively.19
Currently, the main virulence genes found on the OrfV genome are VIR, vIL-10, GIF and VEGF. They are located at inverted repeats of genome terminals and play important roles in OrfV infection and pathogenesis. The virulence genes VIR and GIF also showed homology at the nucleotide and the amino acid level. However, the VEGF gene showed large variations, particularly at amino acid sequence level. As a result, this locus confers the most virulence for the OrfV.19
One group investigated an Orf outbreak in a flock of sheep at the Central Institute for Research on Goats in Makhdoom, India. On comparison of nucleotide and amino acid sequences, a unique 126S residue was observed in the Indian sheep, indicating that completely new strain exists in India.20
Management
At present, there are no effective antiviral treatments available for OrfV, and rapid diagnosis is therefore critical for effective control of the disease. Infections with OrfV (as with all Parapoxvirus) do not confer lifelong immunity. However, vaccines for primary prevention do exist. The DNA vaccine pcDNA3.1-ORFV011/ORFV059 expressing ORFV011 and ORFV059 chemeric-proteins were found effective in some goats in China.21
Vaccination with attenuated OrfV is the most common method to prevent and control the disease. It reduces the infection rate to a certain extent. However, there are recent reports showing that the vaccination with the attenuated virus cannot provide effective protection, suggesting that the OrfV epidemic strains might have been changed genetically under the current immune pressure.
One study revealed that RNA interference (RNAi) targeting of the OrfV DNA polymerase gene is potentially useful for therapeutic applications. Three small interfering RNA (siRNA) — siRNA704, siRNA1017 and siRNA1388 — prepared by in vitro transcription had reduced virus titers by 59- to 199-fold and reduced the level of viral replication by 73% to 89%.22 One group reported resolution with doxycycline.
Patient Management
Upon further questioning, the patient admitted to having been in contact with a sheep a few days prior to the development of the lesion. He was informed of the diagnosis and wound care with silver nitrate and fucidic acid cream (topical antibacterial) was started. At the 3-week follow-up, the lesion was healing with regression of the swelling and erythema.
Conclusion
OrfV is a double-stranded DNA virus that belongs to the Parapoxvirus genus. In humans, the disease usually presents as a painful nodule on the dorsal side of the fingers or hands that regresses, sometimes appearing like a bacterial infection or neoplasm. Histological analysis demonstrates balloon degeneration in the epidermis, lymphocytes, neutrophils and abundant eosinophils. At present, there are no effective antiviral treatments available for OrfV. Vaccination with attenuated OrfV is the most common method to prevent and control the disease.
Dr. Kallini is with Saint Louis University in St. Louis, MO.
Dr. Ehrsam is in private practice dermatology in Lille, France.
Dr. Khachemoune, the Section Editor of Derm DX, is with the Department of Dermatology at the State University of New York Downstate and Veterans Affairs Medical Center, both in Brooklyn, NY.
Disclosure: The authors report no relevant financial relationships.
References
1. Zhang K, Liu Y, Kong H, Shang Y, Liu X. Human infection with Orf virus from goats in China, 2012. Vector Borne Zoonotic Dis. 2014;14(5):365-367.
2. Giangaspero M, Bonfini B, Orusa R, Savini G, Osawa T, Harasawa R. Epidemiological survey for Toxoplasma gondii, Chlamydia psittaci var. ovis, Mycobacterium paratuberculosis, Coxiella burnetii, Brucella spp., leptospirosis and Orf virus among sheep from northern districts of Japan.
J Vet Med Sci. 2013;75(5):679-684.
3. Centers for Disease Control and Prevention. Human Orf virus infection from household exposures - United States, 2009-2011. MMWR Morb Mortal Wkly Rep. 2012;61(14):245-248.
4. Hawayek LH, Rubeiz N. Orf. Medscape. May 28, 2013. https://emedicine.medscape.com/article/1133450-overview. Accessed February 19, 2015.
5. Kitchen M, Müller H, Zobl A, Windisch A, Romani N, Huemer H. ORF virus infection in a hunter in Western Austria, presumably transmitted by game. Acta Derm Venereol. 2014;94(2):212-214.
6. Turan E, Yesilova Y, Ucmak D. A case of orf (ecthyma contagiosum) with multiple lesions. J Pak Med Assoc. 2013;63(6):786-787.
7. Gao F, Yuan H, Ling H, et al. An outbreak of human orf disease caused by introduced black goats. Zhonghua Liu Xing Bing Xue Za Zhi. 2011;32(9):905-907.
8. Veraldi S, Nazzaro G, Vaira F, Cuka E. Presentation of orf (ecthyma contagiosum) after sheep slaughtering for religious feasts. Infection. 2014;42(4):767-769.
9. Nougairede A, Fossati C, Salez N, et al. Sheep-to-human transmission of Orf virus during Eid al-Adha religious practices, France. Emerg Infect Dis. 2013;19(1):102-105.
10. Turk BG, Senturk B, Dereli T, Yaman B. A rare human-to-human transmission of orf. Int J Dermatol. 2014;53(1):e63-65.
11. Midilli K, Erkiliç A, Kuskucu M, et al. Nosocomial outbreak of disseminated orf infection in a burn unit, Gaziantep, Turkey, October to December 2012. Euro Surveill. 2013;18(11):20425.
12. de Sant’Ana FJ, Leal FA, Rabelo RE, et al. Coinfection by Vaccinia virus and an Orf virus-like parapoxvirus in an outbreak of vesicular disease in dairy cows in midwestern Brazil. J Vet Diagn Invest. 2013;25(2):267-272.
13. de Oliveira CH, Assis FL, Neto JD, et al. Multifocal cutaneous ORF virus infection in goats in the Amazon region, Brazil. Vector Borne Zoonotic Dis. 2012;12(4):336-340.
14. Lieu TJ, Park AN, Ahmed AM, Blanco GM, Luby JP. PHOTO QUIZ. A generalized eruption in a rancher. Clin Infect Dis. 2013;56(11):1613, 1675-1676.
15. Zhao H, Wilkins K, Damon IK, Li Y. Specific qPCR assays for the detection of orf virus, pseudocowpox virus and bovine papular stomatitis virus. J Virol Methods. 2013;194(1-2):229-234.
16. Venkatesan G, Bhanuprakash V, Balamurugan V, et al. Rapid detection and quantification of Orf virus from infected scab materials of sheep and goats. Acta Virol. 2012;56(1):81-83.
17. Li J, Song D, He W, et al. Rapid detection of orf virus by loop-mediated isothermal amplification based on the DNA polymerase gene. Arch Virol. 2013;158(4):793-798.
18. Yu YZ, Tong CY, Song BF, et al. Molecular mechanism of ORFV intervention strategies based on the UPS of host cell: a review. Bing Du Xue Bao. 2013;29(6):662-666.
19. Yang H, Meng Q, Qiao J, et al. Detection of genetic variations in Orf virus isolates epidemic in Xinjiang China. J Basic Microbiol. 2014;54(11):1273-1278.
20. Kumar N, Wadhwa A, Chaubey KK, et al. Isolation and phylogenetic analysis of an orf virus from sheep in Makhdoom, India. Virus Genes. 2014;48(2):312-319.
21. Zhao K, He W, Gao W, et al. Orf virus DNA vaccines expressing ORFV 011 and ORFV 059 chimeric protein enhances immunogenicity.
Virol J. 2011;8:562.
22. Wang G, He W, Song D, et al. In vitro RNA interference targeting the DNA polymerase gene inhibits orf virus replication in primary ovine fetal turbinate cells. Arch Virol. 2014;159(5):915-920.