What Caused These Nonresponsive Pruritic, Erythematous, Scaly Patches and Plaques?
Case
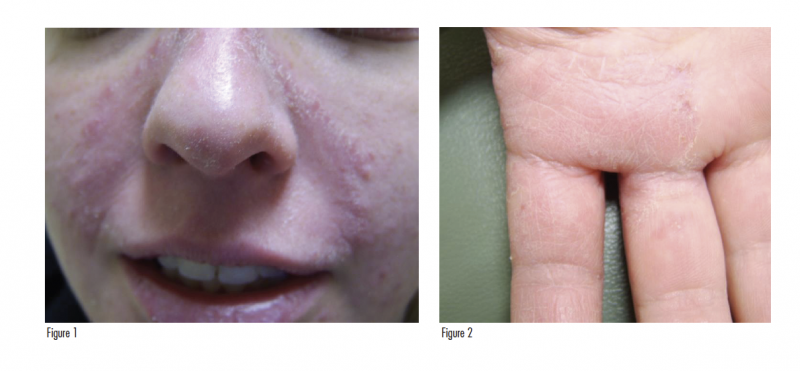
A 22-year-old female equestrian with a history of atopic dermatitis presented with mild to moderate pruritic, erythematous patches on her face (Figure 1), upper back, and fingers (Figure 2). Prior to this initial office visit, treatment with a “ringworm ointment” was unsuccessful. Physical examination revealed an erythematous, scaly patch on her upper cutaneous lip, erythematous, annular, scaly patches on her upper midline back, and dyshidrosiform vesicles on her fingers. Scalp lesions were not noted.
What is your diagnosis?
Answer
Diffuse Dermatophytosis Involving the Face, Hands, and Trunk
Dermatophytic infections involve keratinized tissues,1 including the superficial epidermis.2 While our patient’s diagnosis includes tinea corporis, tinea manuum, and tinea faciei, this article will focus on the latter 2 conditions.
Tinea manuum, a dermatophytic infection of the hands, is related to contact with hedgehogs,3 rabbits, guinea pigs, dogs, cats,4 and infected humans. The prevalence of tinea manuum peaks after puberty.5
Tinea faciei, a dermatophyte infection of the face, occurs most commonly in warm, humid regions among individuals of all ages. Two peaks in prevalence have been shown: childhood and early adulthood.6,7 In childhood, it is often a result of being in crowded areas such as schools, contact with other children, and contact with domestic pets, including cats, dogs, and rabbits.4 In adults, it can occur from contact with livestock, work, or physical and/or social activities, such as going to the gym.4,7 Similar to our patient’s history of contact with horses while living on a farm, tinea infections secondary to contact with horses have been documented, including tinea faciei,8 tinea corporis,8,9 and tinea capitis.10 Among adults, this condition has a higher prevalence in females.2,6,7 The incidence of tinea faciei is not increasing.6 Tinea manuum and tinea faciei are both rare, with each representing less than 5% of tinea patients.1,4,11,12 Tinea infections in concurrent locations can occur, including tinea faciei and tinea capitis (dermatophytic infection of the head), or tinea faciei and tinea corporis.7 Concurrent infection of the hands (tinea manuum) and feet (tinea pedis) is also possible.
Clinical Presentation of Dermatophytosis
Typical manifestations of tinea infections are referred to as “ringworm” due to their circular erythematous scaling plaque with central clearing.1 In contrast, atypical manifestations can present with more inflammation, less defined borders, less central scaling, follicular papules, and vesicles or pustules instead of the clearing. These findings may sometimes present with induration or hyperpigmentation.7 Atypical cases may also mimic other conditions (Tables 1 and 2). Based on the physical examination findings, our patient’s tinea presentation was atypical.
In one tinea faciei study, the majority of patients (61/107) were diagnosed with typical presentations, with typical cases more often occurring in younger patients (aged 2 to 15) and atypical forms presenting in all ages (mainly between 36 and 72 years of age). In all patients with atypical presentations, discordant topical therapy, including cortisone, was reported. In contrast, none of the typical cases received discordant topical therapy.7 Another factor involved in atypical presentations of tinea faciei is lesion location. A combination of distinct facial anatomy, facial washing, cosmetic use, and exposure to sunlight can play a role in the lesion morphology.7 In one study, the most common location for tinea faciei was the cheek, followed by the auricles, and the mandible.13
Suspicion of a tinea infection should occur with papulosquamous plaques with an annular scaly edge. This suspicion should rise if the lesions do not resolve with steroid treatment.2 Tinea manuum has been reported to present as an annular erythematous plaque with a raised, slightly scaly border.3
Mycology of Superficial Fungal Infections
Multiple tinea species have been described to cause lesions of the hands and face. Overall, zoophilic species result in more inflammation and smaller lesions in comparison to anthropophilic fungi.13 While zoophilic species often result in suppurative lesions, nonsuppurative cases have been described.14 The dominant tinea manuum and tinea faciei etiologic species has been shown to vary depending on the region of study.
Tinea manuum causative organisms:
- Trichophyton rubrum,4,15,16 T mentapgrophytes var. erinacei,3 Trichophyton interdigitale4
Tinea faciei causative organisms:
- United States: T tonsurans, T rubrum, Microsporum canis6
- Italy: M canis,6,7 T rubrum,7 T mentagrophytes,7 T interdigitale6
- Switzerland: T rubrum, T mentagrophytes6
- Japan: T rubrum, T tonsurans, T mentagrophytes, T verrucosum, T violaceum, M canis, M gypseum13
- Iran: T interdigitale, T tonsurans,T rubrum, M canis4
- China: T mentagrophytes, M canis15
- Nigeria: T rubrum12
- Unusual presentation: T erinacei14
Dermatophytoses secondary to contact with horses have also been reported, with causative organisms including Arthroderma vanbreuseghemii,8 M aenigmaticum,9 and T equinum.10
Diagnosis
With observation of the classical circular erythematous scaling plaque with central clearing, clinical diagnosis of tinea faciei is possible. To clinically diagnose atypical tinea faciei, Nicola and colleagues suggest the following clues7:
- Small follicular papules and vesicle-pustules, with brittle or fragmented hairs inside.
- Serpiginous if not semi-annular borders with constant scaling, even if a central clearing is absent and desquamation seems diffused.
- Indolence and very slow progression of disease, especially if compared with diseases such as discoid lupus or polymorphous light eruption.
- Less symmetrical onset and progression of the lesion.
With suspicious cases, microscopic examination of skin scrapings of the lesion borders with potassium hydroxide (KOH) can lead to immediate diagnosis. On examination, hyphae and spores will be seen. While it does not alter the treatment, a culture can be used to identify the specific dermatophyte species. False-negative results, however, are possible with fungal scraping and cultures, especially after medical therapy with steroids and antifungal agents.2 In addition, sampling error may play a role in false-negative outcomes. In comparison to culture, molecular identification by polymerase chain reaction (PCR) is equal in cost, more accurate, and more rapid.17 PCR also allows for correlations between the host and the causative infectious agent.3 In rare occasions, a punch biopsy may be necessary to diagnose the infection or evaluate other causes.
Differential Diagnosis
As tinea manuum and tinea faciei can frequently present with atypical symptoms and/or phenotypes, a broad differential diagnosis for each condition results (Tables 1 and 2). Some less common tinea faciei differential diagnosis considerations include bacterial infections, herpes simplex,7 and impetigo.13
Management
In a majority of tinea cases, local topical antifungal therapy is sufficient, including imidazoles or allylamines. Systemic therapies should be considered for resistant, chronic, hyperkeratotic, widespread cases.5 Oral antifungal therapy should also be used if nails or hair are involved, as the topical therapy is unable to reach the depth of the follicle.2,7 In these cases, monitoring of systemic effects is indicated, including the hepatic, renal, and hematopoietic systems.5 In addition, in cases of tinea faciei, in order to prevent reinfection, a check of the nails is indicated.7
Our Patient
While the logical first step in the diagnosis of a dermatophytosis is a KOH fungal smear, our patient’s past medical history led us down another diagnostic path. Given her history of atopic dermatitis, a low-potency steroid was prescribed for use on her face, while a high-potency steroid (clobetasol cream twice a day) was prescribed for use on her fingers. Based on clinical appearance, econazole cream was prescribed for the patches on her back.
Four months after presentation, follow-up revealed extension of the scaly, erythematous patches on her face involving the lateral canthus of the left eye, as well as progression to an erythematous, well-demarcated plaque on her lower nose. She experienced mild improvement of the patches on her upper midline back, but no improvement of the hand lesions, which progressed to scaly, erythematous plaques with small fissures on her right medial hand. Similar to her previous visit, scalp lesions were not noted.
A 2 mm punch biopsy was performed from a representative scaly plaque on the right nasolabial sulcus and second right dorsal finger (see Figures 1 and 2), yielding the diagnoses of dermatophytosis with follicular involvement and dermatophytosis, respectively. Due to the follicular involvement of the dermatophytosis, grifulvin 250 mg orally twice a day for 1 month was initiated, which led to resolution of these erythematous, scaly patches and plaques. As a culture or PCR was not performed, the specific tinea etiologic species was not identified. While the source of infection is uncertain, the patient may have contracted the tinea from her history of contact with horses. Previous reports of this mode of infection have recently appeared, with the specific causative organisms listed above.8-10
Conclusion
This case illustrates nonresponsive, pruritic, erythematous patches which initially presented on the face, trunk, and hands. Biopsy revealed dermatophytosis, leading to the diagnoses of tinea faciei, tinea corporis, and tinea manuum, respectively. Tinea faciei is a dermatophyte infection of the glabrous skin of the face,13 which has been reported to occur secondary to contact with animals, including horses.8-10 Tinea faciei may present with typical manifestations (circular erythematous scaling lesion with central clearing) or with atypical manifestations (more inflammation, less defined borders and central scaling, follicular papules, vesicles, or pustules instead of the clearing). Tinea manuum, a dermatophytic infection of the hands, is often related to contact with hedgehogs,3 rabbits, guinea pigs, dogs, cats,4 and infected humans. Depending on the patient’s geographic location, the etiologic fungus may differ, but may be diagnosed clinically, with a KOH skin scraping, or through molecular identification. As tinea faciei may have a wide array of presentations, a large differential diagnosis is present. The majority of cases, however, will respond to topical antifungal therapy. In more resistant or widespread cases, systemic therapy may be indicated.
Affiliations and Disclosures
Mr Saikaly is a fourth-year medical student at University of Central Florida College of Medicine in Orlando, FL.
Dr Khachemoune, the Section Editor of Derm DX, is with the department of dermatology at Veteran Affairs Medical Center, and the department of dermatology at the State University of New York Downstate, both in Brooklyn, NY.
Disclosure: The authors report no relevant financial relationships.
References
1. Bhatia VK, Sharma PC. Epidemiological studies on Dermatophytosis in human patients in Himachal Pradesh, India. Springerplus. 2014;3:134.
2. Yeo BK, Tey HL. A persistent facial rash. Am Fam Physician. 2013;87(8):579-580.
3. Perrier P, Monod M. Tinea manuum caused by Trichophyton erinacei: first report in Switzerland. Int J Dermatol. 2015;54(8):959-960.
4. Abastabar M, Rezaei-Matehkolaei A, Shidfar MR, et al. A molecular epidemiological survey of clinically important Dermatophytes in Iran based on specific RFLP profiles of beta-tubulin Gene. Iran J Public Health. 2013;42(9):1049-1057.
5. Drake LA, Dinehart SM, Farmer ER, et al. Guidelines of care for superficial mycotic infections of the skin: tinea corporis, tinea cruris, tinea faciei, tinea manuum, and tinea pedis. Guidelines/Outcomes Committee. American Academy of Dermatology. J Am Acad Dermatol. 1996;34(2 Pt 1):282-286.
6. Kieliger S, Glatz M, Cozzio A, Bosshard PP. Tinea capitis and tinea faciei in the Zurich area—an 8-year survey of trends in the epidemiology and treatment patterns. J Eur Acad Dermatol Venereol. 2015;29(8):1524-1529.
7. Nicola A, Laura A, Natalia A, Monica P. A 20-year survey of tinea faciei. Mycoses. 2010;53(6):504-508.
8. Chollet A, Wespi B, Roosje P, et al. An outbreak of Arthroderma vanbreuseghemii dermatophytosis at a veterinary school associated with an infected horse. Mycoses. 2015;58(4):233-238.
9. Hubka V, Dobiasova S, Dobias R, Kolarik M. Microsporum aenigmaticum sp. nov. from M. gypseum complex, isolated as a cause of tinea corporis. Med Mycol. 2014;52(4):387-396.
10. Brasch J, Lögering B, Graser Y. Tinea capitis caused by Trichophyton equinum. Acta Derm Venereol. 2009;89(2):204-205.
11. Rezaei-Matehkolaei A, Makimura K, de Hoog S, et al. Molecular epidemiology of dermatophytosis in Tehran, Iran, a clinical and microbial survey. Med Mycol. 2013;51(2):203-207.
12. Oke OO, Onayemi O, Olasode OA, Omisore AG, Oninla OA. The prevalence and pattern of superficial fungal infections among school children in Ile-Ife, South-Western Nigeria. Dermatol Res Pract. 2014;2014:842917.
13. Noguchi H, Jinnin M, Miyata K, Hiruma M, Ihn H. Clinical features of 80 cases of tinea faciei treated at a rural clinic in Japan. Drug Discov Ther. 2014;8(6):245-248.
14. Lee DW, Yang JH, Choi SJ, et al. An unusual clinical presentation of tinea faciei caused by Trichophyton mentagrophytes var. erinacei. Pediatr Dermatol. 2011;28(2):210-212.
15. Cai W, Lu C, Li X, et al. Epidemiology of superficial fungal infections in Guangdong, Southern China: a retrospective study from 2004 to 2014. Mycopathologia. 2016;181(5-6):387-395.
16. Foster KW, Ghannoum MA, Elewski BE. Epidemiologic surveillance of cutaneous fungal infection in the United States from 1999 to 2002. J Am Acad Dermatol. 2004;50(5):748-752.
17. Kang D, Ran Y, Li C, Dai Y, Lama J. Impetigo-like tinea faciei around the nostrils caused by Arthroderma vanbreuseghemii identified using polymerase chain reaction-based sequencing of crusts. Pediatr Dermatol. 2013;30(6):e136-e137.
























