Epidermotropic marginal zone B-cell lymphoma is a rare variant of marginal zone lymphoma first described in 1999 by Chui et al.1 Since, only 7 cases have been reported in the literature.2-4 Part of the
 diagnostic challenge is a clinical presentation which is unlike any form of cutaneous B-cell neoplasia being that of a generalized diffuse truncal and extremity papulosquamous eruption that resembles pityriasis rosea. There has been one recently described case by Barzilai et al5 with a similar phenotype as our patient, mimicking granulomatous rosacea. It has a peculiar predilection to involve middle-aged to older adult males. At further variance with the typical indolent skin confined nature of primary cutaneous marginal zone lymphoma, is the tendency toward extracutaneous dissemination with characteristic bone marrow and spleen involvement.4
diagnostic challenge is a clinical presentation which is unlike any form of cutaneous B-cell neoplasia being that of a generalized diffuse truncal and extremity papulosquamous eruption that resembles pityriasis rosea. There has been one recently described case by Barzilai et al5 with a similar phenotype as our patient, mimicking granulomatous rosacea. It has a peculiar predilection to involve middle-aged to older adult males. At further variance with the typical indolent skin confined nature of primary cutaneous marginal zone lymphoma, is the tendency toward extracutaneous dissemination with characteristic bone marrow and spleen involvement.4
Clinical History
In this case of epidermotropic marginal zone B-cell lymphoma, a 50-year-old man presented initially with an intensely pruritic granulomatous appearing papular rash that developed on the bilateral malar cheeks and face (Figures 1A and B). He underwent a bone marrow biopsy, which revealed infiltration with abnormal CD23+ B lymphocytes at which time he was diagnosed with chronic lymphocytic leukemia despite not having a peripheral blood lymphocytosis. He was otherwise healthy. The initial episode resolved, but he had a recurrence 4 years later along with widespread truncal and extremity papulosquamous eruption. A lesion on the left upper back was biopsied (Figure 1C). Interestingly, 1 month later, a new glabellar nodule was noted and was subsequently biopsied.
 Microscopic Findings
Microscopic Findings
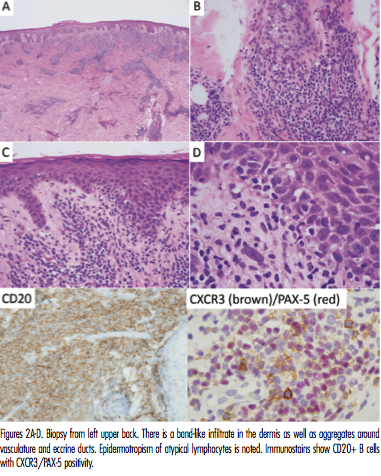
Analysis of a biopsy taken from the back revealed a psoriasiform epidermal hyperplasia accompanied by areas of superficial band-like lymphocytic infiltration with focal infiltration of the epidermis by atypical noncerebriform lymphocytes and plasma cells. A supervening perivascular and perieccrine lymphocytic infiltrate was noted as well. Comprehensive phenotypic studies done revealed that many of the intraepidermal lymphocytes were positive for CXCR3, CD20 but did not express CD5 (Figures 2A-D). There was evidence of lambda light chain restriction amidst the plasma cells. Monoclonality of IgH/IgK were detected via polymerase chain reaction.
The second biopsy, which was performed on new glabellar lesions had findings consistent with folliculotropic mycosis fungoides along with concomitant features of epidermotropic marginal zone lymphoma. There were collections of CD3+, CD4+, and CD7- cerebriform lymphocytes that colonized the hair follicle with intrafollicular Pautrier microabscess formation (Figure 3).
Discussion
This is an interesting case of an epidermotropic marginal zone lymphoma with bone marrow and spleen involvement, as well as concomitant 
follicular mycosis fungoides. The CD23 positivity is unusual but does isolate a subset of marginal zone lymphomas that have a greater tendency toward large cell transformation. Splenic marginal zone lymphoma is also characteristically CD23+. In this and other reported cases, the epidermotropism of the neoplastic B cells resulted in a distinctive clinical presentation that resembled other T-cell disorders exhibiting epidermal T-cell infiltration namely pityriasis rosea. A 2015 study from Magro et al6 hypothesized that CXCR3 expression among neoplastic B cells contributes to the epidermotropic properties of this marginal zone lymphoma based on the expression of its ligand MIG within the epidermis. A similar CXCR3 MIG ligand interaction may be the basis for splenic marginal zone lymphoma and also explain the unusual tendency for epidermotropic marginal zone lymphoma to metastasize to spleen.4,7-10
Our patient also had mycosis fungoides. An analysis on patients with concomittant B-cell and T-cell neoplasms by Barzilai’s group9 led them to propose that the development of one hematologic neoplasm such as mycosis fungoides may predispose that patient to a second hematologic neoplasm, such as a B-cell lymphoma. The epidermotropic nature of mycosis fungoides likely reflects the interaction between the neoplastic T-cell expression of CCR4 and CCR10 that bind to the respective epidermal keratinocyte-derived ligands CCL17 and CCL27. IL-15 may also play a role.
Dr Magro is the director of dermatopathology at Weill Cornell Medicine in New York, NY.
Dr Wang is with Weill Cornell Medical College and Memorial Sloan Kettering Cancer Center, both in New York, NY.
Mr Muhlbauer is with Weill Cornell Medical College in New York, NY.
Dr Roy is with Pine Belt Dermatology in Petal, MS.
Disclosure: The authors report no relevant financial relationships.
References
1. Chui CT, Hoppe RT, Kohler S, Kim YH. Epidermotropic cutaneous B-cell lymphoma mimicking mycosis fungoides. J Am Acad Dermatol. 1999;41(2 Pt 1):271-274.
2. Chiang S, DiCaudo DJ, Valdez R, Swanson DL. Cutaneous B-cell lymphoma with histologic features of mycosis fungoides. J Am Acad Dermatol. 2010;62(2):320-323.
3. Lee BA, Jacobson M, Seidel G. Epidermotropic marginal zone lymphoma simulating mycosis fungoides. J Cutan Pathol. 2013;40(6):569-572.
4. Gómez-de le Guente E, Villalón LB, Calzado-Villarreal L, Pinedo-Moraleda F, López-Estebaranz JL. Splenic marginal zone B-cell lymphoma with epidermotropic skin involvement. Actas Dermosifiliogr. 2012;103(5):427-431.
5. Barzilai A, Feuerman H, Quaglino P, et al. Cutaneous B-cell neoplasms mimicking granulomatous rosacea or rhinophyma. Arch Dermatol. 2012;148(7):824-831.
6. Magro CM, Momtahen S, Lee BA, Swanson DL, Pavlovic MD. Epidermotropic B-cell lymphoma: A unique subset of CXCR3-positive marginal zone lymphoma. Am J Dermatopathol. 2016;38(2):105-112.
7. Trentin L, Agostini C, Facco M, et al. The chemokine receptor CXCR3 is expressed on malignant B cells and mediates chemotaxis. J Clin Investig. 1999;104(1):115-121.
8. Jones D, Benjamin RJ, Shahsafaei A, Dorfman DM. The chemokine receptor CXCR3 is expressed in a subset of B cell lymphomas and is a marker of B cell chronic lymphocytic leaukemia. Blood. 2000;95(2):627-632.
9. Barzilai A, Trau H, David M, et al. Mycosis fungoides associated with B-cell malignancies. Br J Dermatol. 2006;155(2):379-386.
10. Suefuji H, Ohshima K, Karube K, et al. CXCR3-positive B cells found at elevated frequence in the peripheral blood of patients with MALT lymphoma are attracted by MIG and belong to the lymphoma clone. Int J Cancer. 2005;114(6):896-901.
Epidermotropic marginal zone B-cell lymphoma is a rare variant of marginal zone lymphoma first described in 1999 by Chui et al.1 Since, only 7 cases have been reported in the literature.2-4 Part of the diagnostic challenge is a clinical presentation which is unlike any form of cutaneous B-cell neoplasia being that of a generalized diffuse truncal and extremity papulosquamous eruption that resembles pityriasis rosea. There has been one recently described case by Barzilai et al5 with a similar phenotype as our patient, mimicking granulomatous rosacea. It has a peculiar predilection to involve middle-aged to older adult males. At further variance with the typical indolent skin confined nature of primary cutaneous marginal zone lymphoma, is the tendency toward extracutaneous dissemination with characteristic bone marrow and spleen involvement.4 
Clinical History
In this case of epidermotropic marginal zone B-cell lymphoma, a 50-year-old man presented initially with an intensely pruritic granulomatous appearing papular rash that developed on the bilateral malar cheeks and face (Figures 1A and B). He underwent a bone marrow biopsy, which revealed infiltration with abnormal CD23+ B lymphocytes at which time he was diagnosed with chronic lymphocytic leukemia despite not having a peripheral blood lymphocytosis. He was otherwise healthy. The initial episode resolved, but he had a recurrence 4 years later along with widespread truncal and extremity papulosquamous eruption. A lesion on the left upper back was biopsied (Figure 1C). Interestingly, 1 month later, a new glabellar nodule was noted and was subsequently biopsied.
 Microscopic Findings
Microscopic Findings
Analysis of a biopsy taken from the back revealed a psoriasiform epidermal hyperplasia accompanied by areas of superficial band-like lymphocytic infiltration with focal infiltration of the epidermis by atypical noncerebriform lymphocytes and plasma cells. A supervening perivascular and perieccrine lymphocytic infiltrate was noted as well. Comprehensive phenotypic studies done revealed that many of the intraepidermal lymphocytes were positive for CXCR3, CD20 but did not express CD5 (Figures 2A-D). There was evidence of lambda light chain restriction amidst the plasma cells. Monoclonality of IgH/IgK were detected via polymerase chain reaction.
The second biopsy, which was performed on new glabellar lesions had findings consistent with folliculotropic mycosis fungoides along with concomitant features of epidermotropic marginal zone lymphoma. There were collections of CD3+, CD4+, and CD7- cerebriform lymphocytes that colonized the hair follicle with intrafollicular Pautrier microabscess formation (Figure 3).
Discussion
This is an interesting case of an epidermotropic marginal zone lymphoma with bone marrow and spleen involvement, as well as concomitant 
follicular mycosis fungoides. The CD23 positivity is unusual but does isolate a subset of marginal zone lymphomas that have a greater tendency toward large cell transformation. Splenic marginal zone lymphoma is also characteristically CD23+. In this and other reported cases, the epidermotropism of the neoplastic B cells resulted in a distinctive clinical presentation that resembled other T-cell disorders exhibiting epidermal T-cell infiltration namely pityriasis rosea. A 2015 study from Magro et al6 hypothesized that CXCR3 expression among neoplastic B cells contributes to the epidermotropic properties of this marginal zone lymphoma based on the expression of its ligand MIG within the epidermis. A similar CXCR3 MIG ligand interaction may be the basis for splenic marginal zone lymphoma and also explain the unusual tendency for epidermotropic marginal zone lymphoma to metastasize to spleen.4,7-10
Our patient also had mycosis fungoides. An analysis on patients with concomittant B-cell and T-cell neoplasms by Barzilai’s group9 led them to propose that the development of one hematologic neoplasm such as mycosis fungoides may predispose that patient to a second hematologic neoplasm, such as a B-cell lymphoma. The epidermotropic nature of mycosis fungoides likely reflects the interaction between the neoplastic T-cell expression of CCR4 and CCR10 that bind to the respective epidermal keratinocyte-derived ligands CCL17 and CCL27. IL-15 may also play a role.
Dr Magro is the director of dermatopathology at Weill Cornell Medicine in New York, NY.
Dr Wang is with Weill Cornell Medical College and Memorial Sloan Kettering Cancer Center, both in New York, NY.
Mr Muhlbauer is with Weill Cornell Medical College in New York, NY.
Dr Roy is with Pine Belt Dermatology in Petal, MS.
Disclosure: The authors report no relevant financial relationships.
References
1. Chui CT, Hoppe RT, Kohler S, Kim YH. Epidermotropic cutaneous B-cell lymphoma mimicking mycosis fungoides. J Am Acad Dermatol. 1999;41(2 Pt 1):271-274.
2. Chiang S, DiCaudo DJ, Valdez R, Swanson DL. Cutaneous B-cell lymphoma with histologic features of mycosis fungoides. J Am Acad Dermatol. 2010;62(2):320-323.
3. Lee BA, Jacobson M, Seidel G. Epidermotropic marginal zone lymphoma simulating mycosis fungoides. J Cutan Pathol. 2013;40(6):569-572.
4. Gómez-de le Guente E, Villalón LB, Calzado-Villarreal L, Pinedo-Moraleda F, López-Estebaranz JL. Splenic marginal zone B-cell lymphoma with epidermotropic skin involvement. Actas Dermosifiliogr. 2012;103(5):427-431.
5. Barzilai A, Feuerman H, Quaglino P, et al. Cutaneous B-cell neoplasms mimicking granulomatous rosacea or rhinophyma. Arch Dermatol. 2012;148(7):824-831.
6. Magro CM, Momtahen S, Lee BA, Swanson DL, Pavlovic MD. Epidermotropic B-cell lymphoma: A unique subset of CXCR3-positive marginal zone lymphoma. Am J Dermatopathol. 2016;38(2):105-112.
7. Trentin L, Agostini C, Facco M, et al. The chemokine receptor CXCR3 is expressed on malignant B cells and mediates chemotaxis. J Clin Investig. 1999;104(1):115-121.
8. Jones D, Benjamin RJ, Shahsafaei A, Dorfman DM. The chemokine receptor CXCR3 is expressed in a subset of B cell lymphomas and is a marker of B cell chronic lymphocytic leaukemia. Blood. 2000;95(2):627-632.
9. Barzilai A, Trau H, David M, et al. Mycosis fungoides associated with B-cell malignancies. Br J Dermatol. 2006;155(2):379-386.
10. Suefuji H, Ohshima K, Karube K, et al. CXCR3-positive B cells found at elevated frequence in the peripheral blood of patients with MALT lymphoma are attracted by MIG and belong to the lymphoma clone. Int J Cancer. 2005;114(6):896-901.
Epidermotropic marginal zone B-cell lymphoma is a rare variant of marginal zone lymphoma first described in 1999 by Chui et al.1 Since, only 7 cases have been reported in the literature.2-4 Part of the diagnostic challenge is a clinical presentation which is unlike any form of cutaneous B-cell neoplasia being that of a generalized diffuse truncal and extremity papulosquamous eruption that resembles pityriasis rosea. There has been one recently described case by Barzilai et al5 with a similar phenotype as our patient, mimicking granulomatous rosacea. It has a peculiar predilection to involve middle-aged to older adult males. At further variance with the typical indolent skin confined nature of primary cutaneous marginal zone lymphoma, is the tendency toward extracutaneous dissemination with characteristic bone marrow and spleen involvement.4 
Clinical History
In this case of epidermotropic marginal zone B-cell lymphoma, a 50-year-old man presented initially with an intensely pruritic granulomatous appearing papular rash that developed on the bilateral malar cheeks and face (Figures 1A and B). He underwent a bone marrow biopsy, which revealed infiltration with abnormal CD23+ B lymphocytes at which time he was diagnosed with chronic lymphocytic leukemia despite not having a peripheral blood lymphocytosis. He was otherwise healthy. The initial episode resolved, but he had a recurrence 4 years later along with widespread truncal and extremity papulosquamous eruption. A lesion on the left upper back was biopsied (Figure 1C). Interestingly, 1 month later, a new glabellar nodule was noted and was subsequently biopsied.
 Microscopic Findings
Microscopic Findings
Analysis of a biopsy taken from the back revealed a psoriasiform epidermal hyperplasia accompanied by areas of superficial band-like lymphocytic infiltration with focal infiltration of the epidermis by atypical noncerebriform lymphocytes and plasma cells. A supervening perivascular and perieccrine lymphocytic infiltrate was noted as well. Comprehensive phenotypic studies done revealed that many of the intraepidermal lymphocytes were positive for CXCR3, CD20 but did not express CD5 (Figures 2A-D). There was evidence of lambda light chain restriction amidst the plasma cells. Monoclonality of IgH/IgK were detected via polymerase chain reaction.
The second biopsy, which was performed on new glabellar lesions had findings consistent with folliculotropic mycosis fungoides along with concomitant features of epidermotropic marginal zone lymphoma. There were collections of CD3+, CD4+, and CD7- cerebriform lymphocytes that colonized the hair follicle with intrafollicular Pautrier microabscess formation (Figure 3).
Discussion
This is an interesting case of an epidermotropic marginal zone lymphoma with bone marrow and spleen involvement, as well as concomitant 
follicular mycosis fungoides. The CD23 positivity is unusual but does isolate a subset of marginal zone lymphomas that have a greater tendency toward large cell transformation. Splenic marginal zone lymphoma is also characteristically CD23+. In this and other reported cases, the epidermotropism of the neoplastic B cells resulted in a distinctive clinical presentation that resembled other T-cell disorders exhibiting epidermal T-cell infiltration namely pityriasis rosea. A 2015 study from Magro et al6 hypothesized that CXCR3 expression among neoplastic B cells contributes to the epidermotropic properties of this marginal zone lymphoma based on the expression of its ligand MIG within the epidermis. A similar CXCR3 MIG ligand interaction may be the basis for splenic marginal zone lymphoma and also explain the unusual tendency for epidermotropic marginal zone lymphoma to metastasize to spleen.4,7-10
Our patient also had mycosis fungoides. An analysis on patients with concomittant B-cell and T-cell neoplasms by Barzilai’s group9 led them to propose that the development of one hematologic neoplasm such as mycosis fungoides may predispose that patient to a second hematologic neoplasm, such as a B-cell lymphoma. The epidermotropic nature of mycosis fungoides likely reflects the interaction between the neoplastic T-cell expression of CCR4 and CCR10 that bind to the respective epidermal keratinocyte-derived ligands CCL17 and CCL27. IL-15 may also play a role.
Dr Magro is the director of dermatopathology at Weill Cornell Medicine in New York, NY.
Dr Wang is with Weill Cornell Medical College and Memorial Sloan Kettering Cancer Center, both in New York, NY.
Mr Muhlbauer is with Weill Cornell Medical College in New York, NY.
Dr Roy is with Pine Belt Dermatology in Petal, MS.
Disclosure: The authors report no relevant financial relationships.
References
1. Chui CT, Hoppe RT, Kohler S, Kim YH. Epidermotropic cutaneous B-cell lymphoma mimicking mycosis fungoides. J Am Acad Dermatol. 1999;41(2 Pt 1):271-274.
2. Chiang S, DiCaudo DJ, Valdez R, Swanson DL. Cutaneous B-cell lymphoma with histologic features of mycosis fungoides. J Am Acad Dermatol. 2010;62(2):320-323.
3. Lee BA, Jacobson M, Seidel G. Epidermotropic marginal zone lymphoma simulating mycosis fungoides. J Cutan Pathol. 2013;40(6):569-572.
4. Gómez-de le Guente E, Villalón LB, Calzado-Villarreal L, Pinedo-Moraleda F, López-Estebaranz JL. Splenic marginal zone B-cell lymphoma with epidermotropic skin involvement. Actas Dermosifiliogr. 2012;103(5):427-431.
5. Barzilai A, Feuerman H, Quaglino P, et al. Cutaneous B-cell neoplasms mimicking granulomatous rosacea or rhinophyma. Arch Dermatol. 2012;148(7):824-831.
6. Magro CM, Momtahen S, Lee BA, Swanson DL, Pavlovic MD. Epidermotropic B-cell lymphoma: A unique subset of CXCR3-positive marginal zone lymphoma. Am J Dermatopathol. 2016;38(2):105-112.
7. Trentin L, Agostini C, Facco M, et al. The chemokine receptor CXCR3 is expressed on malignant B cells and mediates chemotaxis. J Clin Investig. 1999;104(1):115-121.
8. Jones D, Benjamin RJ, Shahsafaei A, Dorfman DM. The chemokine receptor CXCR3 is expressed in a subset of B cell lymphomas and is a marker of B cell chronic lymphocytic leaukemia. Blood. 2000;95(2):627-632.
9. Barzilai A, Trau H, David M, et al. Mycosis fungoides associated with B-cell malignancies. Br J Dermatol. 2006;155(2):379-386.
10. Suefuji H, Ohshima K, Karube K, et al. CXCR3-positive B cells found at elevated frequence in the peripheral blood of patients with MALT lymphoma are attracted by MIG and belong to the lymphoma clone. Int J Cancer. 2005;114(6):896-901.

 Microscopic Findings
Microscopic Findings






 diagnostic challenge is a clinical presentation which is unlike any form of cutaneous B-cell neoplasia being that of a generalized diffuse truncal and extremity papulosquamous eruption that resembles pityriasis rosea. There has been one recently described case by Barzilai et al5 with a similar phenotype as our patient, mimicking granulomatous rosacea. It has a peculiar predilection to involve middle-aged to older adult males. At further variance with the typical indolent skin confined nature of primary cutaneous marginal zone lymphoma, is the tendency toward extracutaneous dissemination with characteristic bone marrow and spleen involvement.4
diagnostic challenge is a clinical presentation which is unlike any form of cutaneous B-cell neoplasia being that of a generalized diffuse truncal and extremity papulosquamous eruption that resembles pityriasis rosea. There has been one recently described case by Barzilai et al5 with a similar phenotype as our patient, mimicking granulomatous rosacea. It has a peculiar predilection to involve middle-aged to older adult males. At further variance with the typical indolent skin confined nature of primary cutaneous marginal zone lymphoma, is the tendency toward extracutaneous dissemination with characteristic bone marrow and spleen involvement.4 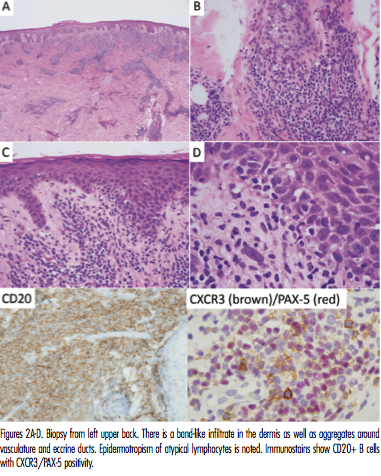 Microscopic Findings
Microscopic Findings















