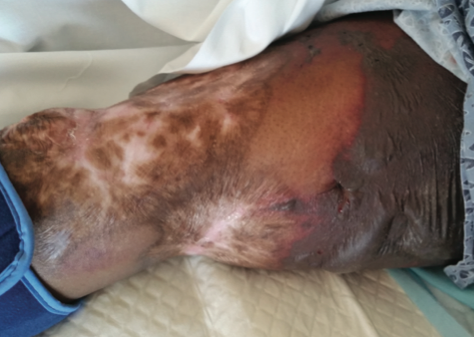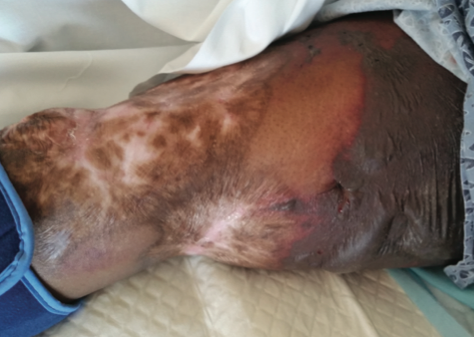
A 58-year-old African American woman presented to the emergency department with a 1-week history of tender sores and erosions on her arms, legs, and trunk. Her medical history included diabetes, hypertension, lupus, and congestive heart failure. She admitted to repeated cocaine use for more than 20 years. Physical examination demonstrated multiple hyperpigmented, excoriated plaques on a background of retiform purpura (Figure). At subsequent visits at the dermatology clinic, the clinical diagnosis of Coumadin (warfarin) necrosis was entertained. On further questioning and review of her medication list, the patient reported being on Coumadin for at least 6 months. Both original and repeat cutaneous biopsies demonstrated leukocytoclastic vasculitis with associated fibrin thrombi.
What's Your Diagnosis?
To learn the answer, go to page 2
{{pagebreak}}
Levamisole-adulterated cocaine abuse often presents a diagnostic challenge. Presentation typically includes marked cutaneous findings that often resemble a number of other clinical entities. Diagnostic testing can also be difficult without knowledge of both the entity and/or supportive patient history. We report a case of a patient with cutaneous manifestations of levamisole-adulterated cocaine use and review the clinical, diagnostic, and therapeutic actions utilized to treat such patients.
Levamisole is an immunostimulant first synthesized as an antihelminthic agent. It is being used to adulterate cocaine, creating a public health concern among recreational users. Many cocaine manufacturers are using levamisole as a cutting agent prior to distribution, thereby adding bulk to their product without changing its appearance. Recent evidence suggests that 80% of cocaine in the United States is adulterated with levamisole.
In addition to its bulking capability, levamisole is thought to enhance the psychotropic effects of cocaine, thus creating a more intense euphoria during the high recreational users seek. It is thought that levamisole may also inhibit the action of monoamine oxidase and catechol O-methyltransferase, both of which are responsible for metabolizing dopamine and serotonin within the synaptic cleft, thereby prolonging the duration of action and enhancing the psychotropic effects of cocaine by allowing increased dopamine and serotonin availability for postsynaptic uptake. It has been postulated that both cocaine and levamisole increase dopamine concentrations in the euphoric centers of the brain, thus enhancing the addictive potential of levamisole-adulterated cocaine in comparison to unadulterated cocaine.
Of particular concern is the potential for levamisole to cause the formation of antibodies to various antigens due to its ability to act as a hapten. This can lead to an immune response caused by the opsonization and eventual destruction of leukocytes.
The wide differential diagnosis of levamisole-adulterated cocaine use makes for a difficult initial diagnosis, especially a poor history and denial of drug abuse. Additionally, its resemblance to other conditions such as Coumadin necrosis might push therapeutic action in a different manner than might be helpful.
The vasculitic syndrome associated with levamisole-adulterated cocaine usage is often characterized by positive p-ANCA (antineutrophil cytoplasmic antibodies) serologies (with or without antibodies against myeloperoxidase), neutropenia/agranulocytosis, purpuric lesions, and some evidence of hypercoagulability. Additionally, a majority of cases are also positive for antiphospholipid antibodies. The presence of these antibodies can help distinguish levamisole-induced cocaine vasculitis from other ANCA-associated vasculitides (eg, Wegener granulomatosis), which may present similarly. However, other ANCA-associated vasculitides most often present with lower ANCA titers compared with the ANCA titers of levamisole-induced cocaine vasculitis, and these antibodies are often specific to 1 neutrophilic antigen rather than several, further differentiating it from levamisole-adulterated cocaine vasculitis.
Also, it is thought that ANCA antibodies against human elastase can also distinguish between levamisole-induced cocaine vasculitis and other autoimmune vasculitides.4 Unadulterated cocaine can also induce ANCA-associated vasculitis; however, this cocaine-induced granulomatosis with polyangitis often demonstrates positive c-ANCA and PR3 antibody. This is different from levamisole-induced cocaine vasculitis, which often demonstrates a p-ANCA predominant pattern.3
Cutaneous biopsies demonstrate leukocytoclastic vasculitis with or without microthrombi.4 Fibrinoid necrosis of vascular walls is also often seen and can extend into perivascular connective tissue.
Clinical Presentation
The presentation of levamisole-induced cocaine vasculitis is often ambiguous and includes nonspecific constitutional symptoms such as fever, fatigue, night sweats, weight loss, and other flu-like symptoms. Cutaneous manifestations will eventually present upon further usage and include retiform purpuric plaques in half of the cases (Figure). These lesions have a predilection for ear lobes, the nose, and the lower extremities with relative sparing of the trunk and back. This type of distribution is unique to levamisole-induced cocaine vasculitis and can be used as a distinguishing feature in comparison to the cutaneous manifestations observed in ANCA-associated systemic vasculitides.3 In severe cases, such cutaneous findings can eventually lead to auto-amputation, particularly of the nose, or a need for amputation of the lower extremities.
Diagnosing levamisole-induced cocaine vasculitis is centered around a history of adulterated cocaine use. Biopsy can be confirmatory but may not be a straightforward histologic diagnosis without some clinical hint of this possibility.4 Common emergency medicine laboratory screening such as urine drug screen may be the first indicator as many patients will deny the use of recreational drugs. Because levamisole has a short half-life and slight renal excretion, detection within urine is only possible within 48 hours of exposure.
Treatment
Treatment of levamisole-induced cocaine vasculitis is largely supportive, including discontinuation of levamisole-induced cocaine. For symptomatic relief in the case of mild organ damage, a corticosteroid treatment may be warranted. In severe cases, however, aggressive immunosuppressive therapy and plasmapheresis may be necessary.4
Our Patient
Treatment of our patient consisted of supportive wound care. Her lack of compliance and continued use of cocaine hindered improvement.
Conclusion
Levamisole-adulterated cocaine abuse often presents a diagnostic challenge, particularly without supportive history of cocaine abuse. Because patients are often hesitant to reveal this information, diagnosis hinges on recognition of clinical findings. In addition, the presentation is complicated by resemblance to a number of other clinical entities.
Aarti Duggal is with the department of internal medicine at Mercer University School of Medicine in Macon, GA.
Dr Goldman is with the department of family practice at Mercer University School of Medicine in Macon, GA.
Dr Lane is with the department of internal medicine and the department of surgery at Mercer University School of Medicine in Macon, GA.
Disclosure: The authors report no relevant financial relationships.
References
1. Crowe DR, Kim PS, Mutasim DF. Clinical, histopathologic, and immunofluorescence findings in levamisole/cocaine-induced thrombotic vasculitis. Int J Dermatol. 2014;53(5):635-637.
2. Chung C, Tumeh PC, Birnbaum R, et al. Characteristic purpura of the ears, vasculitis, and neutropenia–a potential public health epidemic associated with levamisole-adulterated cocaine. J Am Acad Dermatol. 2011;65(4):722-725.
3. Nolan AL, Jen KY. Pathologic manifestations of levamisole-adulterated cocaine exposure. Diagn Pathol. 2015;10:48.
4. Strazzula L, Brown KK, Brieva JC, et al. Levamisole toxicity mimicking autoimmune disease. J Am Acad Dermatol. 2013;69(6):954-959.

A 58-year-old African American woman presented to the emergency department with a 1-week history of tender sores and erosions on her arms, legs, and trunk. Her medical history included diabetes, hypertension, lupus, and congestive heart failure. She admitted to repeated cocaine use for more than 20 years. Physical examination demonstrated multiple hyperpigmented, excoriated plaques on a background of retiform purpura (Figure). At subsequent visits at the dermatology clinic, the clinical diagnosis of Coumadin (warfarin) necrosis was entertained. On further questioning and review of her medication list, the patient reported being on Coumadin for at least 6 months. Both original and repeat cutaneous biopsies demonstrated leukocytoclastic vasculitis with associated fibrin thrombi.
What's Your Diagnosis?
Levamisole-adulterated cocaine abuse often presents a diagnostic challenge. Presentation typically includes marked cutaneous findings that often resemble a number of other clinical entities. Diagnostic testing can also be difficult without knowledge of both the entity and/or supportive patient history. We report a case of a patient with cutaneous manifestations of levamisole-adulterated cocaine use and review the clinical, diagnostic, and therapeutic actions utilized to treat such patients.
Levamisole is an immunostimulant first synthesized as an antihelminthic agent. It is being used to adulterate cocaine, creating a public health concern among recreational users. Many cocaine manufacturers are using levamisole as a cutting agent prior to distribution, thereby adding bulk to their product without changing its appearance. Recent evidence suggests that 80% of cocaine in the United States is adulterated with levamisole.
In addition to its bulking capability, levamisole is thought to enhance the psychotropic effects of cocaine, thus creating a more intense euphoria during the high recreational users seek. It is thought that levamisole may also inhibit the action of monoamine oxidase and catechol O-methyltransferase, both of which are responsible for metabolizing dopamine and serotonin within the synaptic cleft, thereby prolonging the duration of action and enhancing the psychotropic effects of cocaine by allowing increased dopamine and serotonin availability for postsynaptic uptake. It has been postulated that both cocaine and levamisole increase dopamine concentrations in the euphoric centers of the brain, thus enhancing the addictive potential of levamisole-adulterated cocaine in comparison to unadulterated cocaine.
Of particular concern is the potential for levamisole to cause the formation of antibodies to various antigens due to its ability to act as a hapten. This can lead to an immune response caused by the opsonization and eventual destruction of leukocytes.
The wide differential diagnosis of levamisole-adulterated cocaine use makes for a difficult initial diagnosis, especially a poor history and denial of drug abuse. Additionally, its resemblance to other conditions such as Coumadin necrosis might push therapeutic action in a different manner than might be helpful.
The vasculitic syndrome associated with levamisole-adulterated cocaine usage is often characterized by positive p-ANCA (antineutrophil cytoplasmic antibodies) serologies (with or without antibodies against myeloperoxidase), neutropenia/agranulocytosis, purpuric lesions, and some evidence of hypercoagulability. Additionally, a majority of cases are also positive for antiphospholipid antibodies. The presence of these antibodies can help distinguish levamisole-induced cocaine vasculitis from other ANCA-associated vasculitides (eg, Wegener granulomatosis), which may present similarly. However, other ANCA-associated vasculitides most often present with lower ANCA titers compared with the ANCA titers of levamisole-induced cocaine vasculitis, and these antibodies are often specific to 1 neutrophilic antigen rather than several, further differentiating it from levamisole-adulterated cocaine vasculitis.
Also, it is thought that ANCA antibodies against human elastase can also distinguish between levamisole-induced cocaine vasculitis and other autoimmune vasculitides.4 Unadulterated cocaine can also induce ANCA-associated vasculitis; however, this cocaine-induced granulomatosis with polyangitis often demonstrates positive c-ANCA and PR3 antibody. This is different from levamisole-induced cocaine vasculitis, which often demonstrates a p-ANCA predominant pattern.3
Cutaneous biopsies demonstrate leukocytoclastic vasculitis with or without microthrombi.4 Fibrinoid necrosis of vascular walls is also often seen and can extend into perivascular connective tissue.
Clinical Presentation
The presentation of levamisole-induced cocaine vasculitis is often ambiguous and includes nonspecific constitutional symptoms such as fever, fatigue, night sweats, weight loss, and other flu-like symptoms. Cutaneous manifestations will eventually present upon further usage and include retiform purpuric plaques in half of the cases (Figure). These lesions have a predilection for ear lobes, the nose, and the lower extremities with relative sparing of the trunk and back. This type of distribution is unique to levamisole-induced cocaine vasculitis and can be used as a distinguishing feature in comparison to the cutaneous manifestations observed in ANCA-associated systemic vasculitides.3 In severe cases, such cutaneous findings can eventually lead to auto-amputation, particularly of the nose, or a need for amputation of the lower extremities.
Diagnosing levamisole-induced cocaine vasculitis is centered around a history of adulterated cocaine use. Biopsy can be confirmatory but may not be a straightforward histologic diagnosis without some clinical hint of this possibility.4 Common emergency medicine laboratory screening such as urine drug screen may be the first indicator as many patients will deny the use of recreational drugs. Because levamisole has a short half-life and slight renal excretion, detection within urine is only possible within 48 hours of exposure.
Treatment
Treatment of levamisole-induced cocaine vasculitis is largely supportive, including discontinuation of levamisole-induced cocaine. For symptomatic relief in the case of mild organ damage, a corticosteroid treatment may be warranted. In severe cases, however, aggressive immunosuppressive therapy and plasmapheresis may be necessary.4
Our Patient
Treatment of our patient consisted of supportive wound care. Her lack of compliance and continued use of cocaine hindered improvement.
Conclusion
Levamisole-adulterated cocaine abuse often presents a diagnostic challenge, particularly without supportive history of cocaine abuse. Because patients are often hesitant to reveal this information, diagnosis hinges on recognition of clinical findings. In addition, the presentation is complicated by resemblance to a number of other clinical entities.
Aarti Duggal is with the department of internal medicine at Mercer University School of Medicine in Macon, GA.
Dr Goldman is with the department of family practice at Mercer University School of Medicine in Macon, GA.
Dr Lane is with the department of internal medicine and the department of surgery at Mercer University School of Medicine in Macon, GA.
Disclosure: The authors report no relevant financial relationships.
References
1. Crowe DR, Kim PS, Mutasim DF. Clinical, histopathologic, and immunofluorescence findings in levamisole/cocaine-induced thrombotic vasculitis. Int J Dermatol. 2014;53(5):635-637.
2. Chung C, Tumeh PC, Birnbaum R, et al. Characteristic purpura of the ears, vasculitis, and neutropenia–a potential public health epidemic associated with levamisole-adulterated cocaine. J Am Acad Dermatol. 2011;65(4):722-725.
3. Nolan AL, Jen KY. Pathologic manifestations of levamisole-adulterated cocaine exposure. Diagn Pathol. 2015;10:48.
4. Strazzula L, Brown KK, Brieva JC, et al. Levamisole toxicity mimicking autoimmune disease. J Am Acad Dermatol. 2013;69(6):954-959.

A 58-year-old African American woman presented to the emergency department with a 1-week history of tender sores and erosions on her arms, legs, and trunk. Her medical history included diabetes, hypertension, lupus, and congestive heart failure. She admitted to repeated cocaine use for more than 20 years. Physical examination demonstrated multiple hyperpigmented, excoriated plaques on a background of retiform purpura (Figure). At subsequent visits at the dermatology clinic, the clinical diagnosis of Coumadin (warfarin) necrosis was entertained. On further questioning and review of her medication list, the patient reported being on Coumadin for at least 6 months. Both original and repeat cutaneous biopsies demonstrated leukocytoclastic vasculitis with associated fibrin thrombi.
What's Your Diagnosis?
,
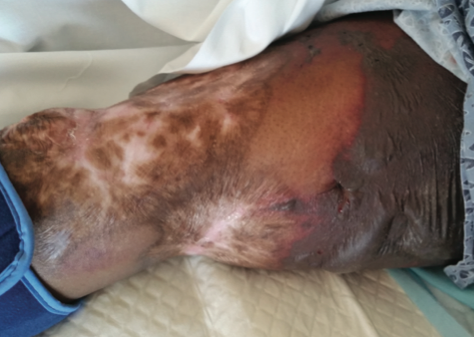
A 58-year-old African American woman presented to the emergency department with a 1-week history of tender sores and erosions on her arms, legs, and trunk. Her medical history included diabetes, hypertension, lupus, and congestive heart failure. She admitted to repeated cocaine use for more than 20 years. Physical examination demonstrated multiple hyperpigmented, excoriated plaques on a background of retiform purpura (Figure). At subsequent visits at the dermatology clinic, the clinical diagnosis of Coumadin (warfarin) necrosis was entertained. On further questioning and review of her medication list, the patient reported being on Coumadin for at least 6 months. Both original and repeat cutaneous biopsies demonstrated leukocytoclastic vasculitis with associated fibrin thrombi.
What's Your Diagnosis?
To learn the answer, go to page 2
{{pagebreak}}
Levamisole-adulterated cocaine abuse often presents a diagnostic challenge. Presentation typically includes marked cutaneous findings that often resemble a number of other clinical entities. Diagnostic testing can also be difficult without knowledge of both the entity and/or supportive patient history. We report a case of a patient with cutaneous manifestations of levamisole-adulterated cocaine use and review the clinical, diagnostic, and therapeutic actions utilized to treat such patients.
Levamisole is an immunostimulant first synthesized as an antihelminthic agent. It is being used to adulterate cocaine, creating a public health concern among recreational users. Many cocaine manufacturers are using levamisole as a cutting agent prior to distribution, thereby adding bulk to their product without changing its appearance. Recent evidence suggests that 80% of cocaine in the United States is adulterated with levamisole.
In addition to its bulking capability, levamisole is thought to enhance the psychotropic effects of cocaine, thus creating a more intense euphoria during the high recreational users seek. It is thought that levamisole may also inhibit the action of monoamine oxidase and catechol O-methyltransferase, both of which are responsible for metabolizing dopamine and serotonin within the synaptic cleft, thereby prolonging the duration of action and enhancing the psychotropic effects of cocaine by allowing increased dopamine and serotonin availability for postsynaptic uptake. It has been postulated that both cocaine and levamisole increase dopamine concentrations in the euphoric centers of the brain, thus enhancing the addictive potential of levamisole-adulterated cocaine in comparison to unadulterated cocaine.
Of particular concern is the potential for levamisole to cause the formation of antibodies to various antigens due to its ability to act as a hapten. This can lead to an immune response caused by the opsonization and eventual destruction of leukocytes.
The wide differential diagnosis of levamisole-adulterated cocaine use makes for a difficult initial diagnosis, especially a poor history and denial of drug abuse. Additionally, its resemblance to other conditions such as Coumadin necrosis might push therapeutic action in a different manner than might be helpful.
The vasculitic syndrome associated with levamisole-adulterated cocaine usage is often characterized by positive p-ANCA (antineutrophil cytoplasmic antibodies) serologies (with or without antibodies against myeloperoxidase), neutropenia/agranulocytosis, purpuric lesions, and some evidence of hypercoagulability. Additionally, a majority of cases are also positive for antiphospholipid antibodies. The presence of these antibodies can help distinguish levamisole-induced cocaine vasculitis from other ANCA-associated vasculitides (eg, Wegener granulomatosis), which may present similarly. However, other ANCA-associated vasculitides most often present with lower ANCA titers compared with the ANCA titers of levamisole-induced cocaine vasculitis, and these antibodies are often specific to 1 neutrophilic antigen rather than several, further differentiating it from levamisole-adulterated cocaine vasculitis.
Also, it is thought that ANCA antibodies against human elastase can also distinguish between levamisole-induced cocaine vasculitis and other autoimmune vasculitides.4 Unadulterated cocaine can also induce ANCA-associated vasculitis; however, this cocaine-induced granulomatosis with polyangitis often demonstrates positive c-ANCA and PR3 antibody. This is different from levamisole-induced cocaine vasculitis, which often demonstrates a p-ANCA predominant pattern.3
Cutaneous biopsies demonstrate leukocytoclastic vasculitis with or without microthrombi.4 Fibrinoid necrosis of vascular walls is also often seen and can extend into perivascular connective tissue.
Clinical Presentation
The presentation of levamisole-induced cocaine vasculitis is often ambiguous and includes nonspecific constitutional symptoms such as fever, fatigue, night sweats, weight loss, and other flu-like symptoms. Cutaneous manifestations will eventually present upon further usage and include retiform purpuric plaques in half of the cases (Figure). These lesions have a predilection for ear lobes, the nose, and the lower extremities with relative sparing of the trunk and back. This type of distribution is unique to levamisole-induced cocaine vasculitis and can be used as a distinguishing feature in comparison to the cutaneous manifestations observed in ANCA-associated systemic vasculitides.3 In severe cases, such cutaneous findings can eventually lead to auto-amputation, particularly of the nose, or a need for amputation of the lower extremities.
Diagnosing levamisole-induced cocaine vasculitis is centered around a history of adulterated cocaine use. Biopsy can be confirmatory but may not be a straightforward histologic diagnosis without some clinical hint of this possibility.4 Common emergency medicine laboratory screening such as urine drug screen may be the first indicator as many patients will deny the use of recreational drugs. Because levamisole has a short half-life and slight renal excretion, detection within urine is only possible within 48 hours of exposure.
Treatment
Treatment of levamisole-induced cocaine vasculitis is largely supportive, including discontinuation of levamisole-induced cocaine. For symptomatic relief in the case of mild organ damage, a corticosteroid treatment may be warranted. In severe cases, however, aggressive immunosuppressive therapy and plasmapheresis may be necessary.4
Our Patient
Treatment of our patient consisted of supportive wound care. Her lack of compliance and continued use of cocaine hindered improvement.
Conclusion
Levamisole-adulterated cocaine abuse often presents a diagnostic challenge, particularly without supportive history of cocaine abuse. Because patients are often hesitant to reveal this information, diagnosis hinges on recognition of clinical findings. In addition, the presentation is complicated by resemblance to a number of other clinical entities.
Aarti Duggal is with the department of internal medicine at Mercer University School of Medicine in Macon, GA.
Dr Goldman is with the department of family practice at Mercer University School of Medicine in Macon, GA.
Dr Lane is with the department of internal medicine and the department of surgery at Mercer University School of Medicine in Macon, GA.
Disclosure: The authors report no relevant financial relationships.
References
1. Crowe DR, Kim PS, Mutasim DF. Clinical, histopathologic, and immunofluorescence findings in levamisole/cocaine-induced thrombotic vasculitis. Int J Dermatol. 2014;53(5):635-637.
2. Chung C, Tumeh PC, Birnbaum R, et al. Characteristic purpura of the ears, vasculitis, and neutropenia–a potential public health epidemic associated with levamisole-adulterated cocaine. J Am Acad Dermatol. 2011;65(4):722-725.
3. Nolan AL, Jen KY. Pathologic manifestations of levamisole-adulterated cocaine exposure. Diagn Pathol. 2015;10:48.
4. Strazzula L, Brown KK, Brieva JC, et al. Levamisole toxicity mimicking autoimmune disease. J Am Acad Dermatol. 2013;69(6):954-959.

A 58-year-old African American woman presented to the emergency department with a 1-week history of tender sores and erosions on her arms, legs, and trunk. Her medical history included diabetes, hypertension, lupus, and congestive heart failure. She admitted to repeated cocaine use for more than 20 years. Physical examination demonstrated multiple hyperpigmented, excoriated plaques on a background of retiform purpura (Figure). At subsequent visits at the dermatology clinic, the clinical diagnosis of Coumadin (warfarin) necrosis was entertained. On further questioning and review of her medication list, the patient reported being on Coumadin for at least 6 months. Both original and repeat cutaneous biopsies demonstrated leukocytoclastic vasculitis with associated fibrin thrombi.
What's Your Diagnosis?
Levamisole-adulterated cocaine abuse often presents a diagnostic challenge. Presentation typically includes marked cutaneous findings that often resemble a number of other clinical entities. Diagnostic testing can also be difficult without knowledge of both the entity and/or supportive patient history. We report a case of a patient with cutaneous manifestations of levamisole-adulterated cocaine use and review the clinical, diagnostic, and therapeutic actions utilized to treat such patients.
Levamisole is an immunostimulant first synthesized as an antihelminthic agent. It is being used to adulterate cocaine, creating a public health concern among recreational users. Many cocaine manufacturers are using levamisole as a cutting agent prior to distribution, thereby adding bulk to their product without changing its appearance. Recent evidence suggests that 80% of cocaine in the United States is adulterated with levamisole.
In addition to its bulking capability, levamisole is thought to enhance the psychotropic effects of cocaine, thus creating a more intense euphoria during the high recreational users seek. It is thought that levamisole may also inhibit the action of monoamine oxidase and catechol O-methyltransferase, both of which are responsible for metabolizing dopamine and serotonin within the synaptic cleft, thereby prolonging the duration of action and enhancing the psychotropic effects of cocaine by allowing increased dopamine and serotonin availability for postsynaptic uptake. It has been postulated that both cocaine and levamisole increase dopamine concentrations in the euphoric centers of the brain, thus enhancing the addictive potential of levamisole-adulterated cocaine in comparison to unadulterated cocaine.
Of particular concern is the potential for levamisole to cause the formation of antibodies to various antigens due to its ability to act as a hapten. This can lead to an immune response caused by the opsonization and eventual destruction of leukocytes.
The wide differential diagnosis of levamisole-adulterated cocaine use makes for a difficult initial diagnosis, especially a poor history and denial of drug abuse. Additionally, its resemblance to other conditions such as Coumadin necrosis might push therapeutic action in a different manner than might be helpful.
The vasculitic syndrome associated with levamisole-adulterated cocaine usage is often characterized by positive p-ANCA (antineutrophil cytoplasmic antibodies) serologies (with or without antibodies against myeloperoxidase), neutropenia/agranulocytosis, purpuric lesions, and some evidence of hypercoagulability. Additionally, a majority of cases are also positive for antiphospholipid antibodies. The presence of these antibodies can help distinguish levamisole-induced cocaine vasculitis from other ANCA-associated vasculitides (eg, Wegener granulomatosis), which may present similarly. However, other ANCA-associated vasculitides most often present with lower ANCA titers compared with the ANCA titers of levamisole-induced cocaine vasculitis, and these antibodies are often specific to 1 neutrophilic antigen rather than several, further differentiating it from levamisole-adulterated cocaine vasculitis.
Also, it is thought that ANCA antibodies against human elastase can also distinguish between levamisole-induced cocaine vasculitis and other autoimmune vasculitides.4 Unadulterated cocaine can also induce ANCA-associated vasculitis; however, this cocaine-induced granulomatosis with polyangitis often demonstrates positive c-ANCA and PR3 antibody. This is different from levamisole-induced cocaine vasculitis, which often demonstrates a p-ANCA predominant pattern.3
Cutaneous biopsies demonstrate leukocytoclastic vasculitis with or without microthrombi.4 Fibrinoid necrosis of vascular walls is also often seen and can extend into perivascular connective tissue.
Clinical Presentation
The presentation of levamisole-induced cocaine vasculitis is often ambiguous and includes nonspecific constitutional symptoms such as fever, fatigue, night sweats, weight loss, and other flu-like symptoms. Cutaneous manifestations will eventually present upon further usage and include retiform purpuric plaques in half of the cases (Figure). These lesions have a predilection for ear lobes, the nose, and the lower extremities with relative sparing of the trunk and back. This type of distribution is unique to levamisole-induced cocaine vasculitis and can be used as a distinguishing feature in comparison to the cutaneous manifestations observed in ANCA-associated systemic vasculitides.3 In severe cases, such cutaneous findings can eventually lead to auto-amputation, particularly of the nose, or a need for amputation of the lower extremities.
Diagnosing levamisole-induced cocaine vasculitis is centered around a history of adulterated cocaine use. Biopsy can be confirmatory but may not be a straightforward histologic diagnosis without some clinical hint of this possibility.4 Common emergency medicine laboratory screening such as urine drug screen may be the first indicator as many patients will deny the use of recreational drugs. Because levamisole has a short half-life and slight renal excretion, detection within urine is only possible within 48 hours of exposure.
Treatment
Treatment of levamisole-induced cocaine vasculitis is largely supportive, including discontinuation of levamisole-induced cocaine. For symptomatic relief in the case of mild organ damage, a corticosteroid treatment may be warranted. In severe cases, however, aggressive immunosuppressive therapy and plasmapheresis may be necessary.4
Our Patient
Treatment of our patient consisted of supportive wound care. Her lack of compliance and continued use of cocaine hindered improvement.
Conclusion
Levamisole-adulterated cocaine abuse often presents a diagnostic challenge, particularly without supportive history of cocaine abuse. Because patients are often hesitant to reveal this information, diagnosis hinges on recognition of clinical findings. In addition, the presentation is complicated by resemblance to a number of other clinical entities.
Aarti Duggal is with the department of internal medicine at Mercer University School of Medicine in Macon, GA.
Dr Goldman is with the department of family practice at Mercer University School of Medicine in Macon, GA.
Dr Lane is with the department of internal medicine and the department of surgery at Mercer University School of Medicine in Macon, GA.
Disclosure: The authors report no relevant financial relationships.
References
1. Crowe DR, Kim PS, Mutasim DF. Clinical, histopathologic, and immunofluorescence findings in levamisole/cocaine-induced thrombotic vasculitis. Int J Dermatol. 2014;53(5):635-637.
2. Chung C, Tumeh PC, Birnbaum R, et al. Characteristic purpura of the ears, vasculitis, and neutropenia–a potential public health epidemic associated with levamisole-adulterated cocaine. J Am Acad Dermatol. 2011;65(4):722-725.
3. Nolan AL, Jen KY. Pathologic manifestations of levamisole-adulterated cocaine exposure. Diagn Pathol. 2015;10:48.
4. Strazzula L, Brown KK, Brieva JC, et al. Levamisole toxicity mimicking autoimmune disease. J Am Acad Dermatol. 2013;69(6):954-959.
Levamisole-adulterated cocaine abuse often presents a diagnostic challenge. Presentation typically includes marked cutaneous findings that often resemble a number of other clinical entities. Diagnostic testing can also be difficult without knowledge of both the entity and/or supportive patient history. We report a case of a patient with cutaneous manifestations of levamisole-adulterated cocaine use and review the clinical, diagnostic, and therapeutic actions utilized to treat such patients.
Levamisole is an immunostimulant first synthesized as an antihelminthic agent. It is being used to adulterate cocaine, creating a public health concern among recreational users. Many cocaine manufacturers are using levamisole as a cutting agent prior to distribution, thereby adding bulk to their product without changing its appearance. Recent evidence suggests that 80% of cocaine in the United States is adulterated with levamisole.
In addition to its bulking capability, levamisole is thought to enhance the psychotropic effects of cocaine, thus creating a more intense euphoria during the high recreational users seek. It is thought that levamisole may also inhibit the action of monoamine oxidase and catechol O-methyltransferase, both of which are responsible for metabolizing dopamine and serotonin within the synaptic cleft, thereby prolonging the duration of action and enhancing the psychotropic effects of cocaine by allowing increased dopamine and serotonin availability for postsynaptic uptake. It has been postulated that both cocaine and levamisole increase dopamine concentrations in the euphoric centers of the brain, thus enhancing the addictive potential of levamisole-adulterated cocaine in comparison to unadulterated cocaine.
Of particular concern is the potential for levamisole to cause the formation of antibodies to various antigens due to its ability to act as a hapten. This can lead to an immune response caused by the opsonization and eventual destruction of leukocytes.
The wide differential diagnosis of levamisole-adulterated cocaine use makes for a difficult initial diagnosis, especially a poor history and denial of drug abuse. Additionally, its resemblance to other conditions such as Coumadin necrosis might push therapeutic action in a different manner than might be helpful.
The vasculitic syndrome associated with levamisole-adulterated cocaine usage is often characterized by positive p-ANCA (antineutrophil cytoplasmic antibodies) serologies (with or without antibodies against myeloperoxidase), neutropenia/agranulocytosis, purpuric lesions, and some evidence of hypercoagulability. Additionally, a majority of cases are also positive for antiphospholipid antibodies. The presence of these antibodies can help distinguish levamisole-induced cocaine vasculitis from other ANCA-associated vasculitides (eg, Wegener granulomatosis), which may present similarly. However, other ANCA-associated vasculitides most often present with lower ANCA titers compared with the ANCA titers of levamisole-induced cocaine vasculitis, and these antibodies are often specific to 1 neutrophilic antigen rather than several, further differentiating it from levamisole-adulterated cocaine vasculitis.
Also, it is thought that ANCA antibodies against human elastase can also distinguish between levamisole-induced cocaine vasculitis and other autoimmune vasculitides.4 Unadulterated cocaine can also induce ANCA-associated vasculitis; however, this cocaine-induced granulomatosis with polyangitis often demonstrates positive c-ANCA and PR3 antibody. This is different from levamisole-induced cocaine vasculitis, which often demonstrates a p-ANCA predominant pattern.3
Cutaneous biopsies demonstrate leukocytoclastic vasculitis with or without microthrombi.4 Fibrinoid necrosis of vascular walls is also often seen and can extend into perivascular connective tissue.
Clinical Presentation
The presentation of levamisole-induced cocaine vasculitis is often ambiguous and includes nonspecific constitutional symptoms such as fever, fatigue, night sweats, weight loss, and other flu-like symptoms. Cutaneous manifestations will eventually present upon further usage and include retiform purpuric plaques in half of the cases (Figure). These lesions have a predilection for ear lobes, the nose, and the lower extremities with relative sparing of the trunk and back. This type of distribution is unique to levamisole-induced cocaine vasculitis and can be used as a distinguishing feature in comparison to the cutaneous manifestations observed in ANCA-associated systemic vasculitides.3 In severe cases, such cutaneous findings can eventually lead to auto-amputation, particularly of the nose, or a need for amputation of the lower extremities.
Diagnosing levamisole-induced cocaine vasculitis is centered around a history of adulterated cocaine use. Biopsy can be confirmatory but may not be a straightforward histologic diagnosis without some clinical hint of this possibility.4 Common emergency medicine laboratory screening such as urine drug screen may be the first indicator as many patients will deny the use of recreational drugs. Because levamisole has a short half-life and slight renal excretion, detection within urine is only possible within 48 hours of exposure.
Treatment
Treatment of levamisole-induced cocaine vasculitis is largely supportive, including discontinuation of levamisole-induced cocaine. For symptomatic relief in the case of mild organ damage, a corticosteroid treatment may be warranted. In severe cases, however, aggressive immunosuppressive therapy and plasmapheresis may be necessary.4
Our Patient
Treatment of our patient consisted of supportive wound care. Her lack of compliance and continued use of cocaine hindered improvement.
Conclusion
Levamisole-adulterated cocaine abuse often presents a diagnostic challenge, particularly without supportive history of cocaine abuse. Because patients are often hesitant to reveal this information, diagnosis hinges on recognition of clinical findings. In addition, the presentation is complicated by resemblance to a number of other clinical entities.
Aarti Duggal is with the department of internal medicine at Mercer University School of Medicine in Macon, GA.
Dr Goldman is with the department of family practice at Mercer University School of Medicine in Macon, GA.
Dr Lane is with the department of internal medicine and the department of surgery at Mercer University School of Medicine in Macon, GA.
Disclosure: The authors report no relevant financial relationships.
References
1. Crowe DR, Kim PS, Mutasim DF. Clinical, histopathologic, and immunofluorescence findings in levamisole/cocaine-induced thrombotic vasculitis. Int J Dermatol. 2014;53(5):635-637.
2. Chung C, Tumeh PC, Birnbaum R, et al. Characteristic purpura of the ears, vasculitis, and neutropenia–a potential public health epidemic associated with levamisole-adulterated cocaine. J Am Acad Dermatol. 2011;65(4):722-725.
3. Nolan AL, Jen KY. Pathologic manifestations of levamisole-adulterated cocaine exposure. Diagn Pathol. 2015;10:48.
4. Strazzula L, Brown KK, Brieva JC, et al. Levamisole toxicity mimicking autoimmune disease. J Am Acad Dermatol. 2013;69(6):954-959.