 A middle-aged woman without any significant past medical history presented with multiple discrete pink papules on the fingers of both of her hands that started 5 weeks prior to presentation. She was not taking any medications. She denied any fatigue, joint pains or fever. Physical examination revealed a thin, middle-aged woman. Her fingers demonstrated multiple 3 mm to 5 mm pink papules on a background of dusky erythema (Figure 1). There was no evidence of the eruption on her feet, legs, arms or trunk.
A middle-aged woman without any significant past medical history presented with multiple discrete pink papules on the fingers of both of her hands that started 5 weeks prior to presentation. She was not taking any medications. She denied any fatigue, joint pains or fever. Physical examination revealed a thin, middle-aged woman. Her fingers demonstrated multiple 3 mm to 5 mm pink papules on a background of dusky erythema (Figure 1). There was no evidence of the eruption on her feet, legs, arms or trunk.
WHAT IS YOUR DIAGNOSIS?
To learn the answer, go to page 2
{{pagebreak}}
Diagnosis: Idiopathic Chilblains
Jennifer C. Aronica, MS, and Nasir Aziz, MD
Chilblains, also referred to as pernio and perniosis, is an inflammatory disorder of acral skin that occurs on areas exposed to non-freezing temperatures. It can mimic vasculitis or thromboemboli and may lead to expensive diagnostic evaluations or inappropriate treatments when physicians are unfamiliar with its features.1
Chilblains was first seen in the damp and cold weather of western Europe.2 However, its occurrence in the northern United States is increasing, possibly as a result of a changing climate.
Epidemiology
Chilblains tends to occur more often in white young to middle age women during the winter and early spring months of November to April when it is damp and the temperature is above freezing. It has been proposed that humidity augments the chilling effect by enhancing thermal conductivity.3-5 Studies have also found an association between low body mass index (BMI) and chilblains, suggesting that these patients may develop the condition due to changes in their thermal regulation patterns.6
Chilblains has also been described in children and in teenagers diagnosed with anorexia nervosa, which could be related to their low BMI.6,7

Etiology
The exact pathogenesis of idiopathic chilblains is unknown. Studies have suggested that patients with chilblains have a continuous and prolonged cold-induced vasoconstriction, which leads to hypoxemia in the affected areas and an inflammatory reaction of the vessel wall.1,3
It is also important to distinguish idiopathic chilblains from that associated with an underlying autoimmune disease such as lupus erythematosus.8 This can be done by using the patient’s history, laboratory results and comparing the histopathological features on a cutaneous biopsy.
Patients with lupus chilblains tend to present at younger ages, have a known history of lupus erythematosus and are more likely to have positive antinuclear and/or anti-Ro/anti-La antibodies.9 A rare form of cutaneous lupus erythematosus has been described in the literature as familial chilblains lupus. This condition presents as inflammatory papules on acral areas, similar to that seen in idiopathic chilblains. A linkage analysis of a large German family with 18 affected individuals showed the locus for these familial lupus chilblains to map to chromosome 3p. Affected family members often showed evidence of antinuclear antibodies or immune complex formation.10
Clinical Findings
Idiopathic chilblains typically manifests as painful dusky erythematous or purple papules localized to acral areas of hands or feet that are associated with swelling and itching (Figure 1). The lesions are bilateral and there is a temporal association with exposure to non-freezing temperatures.1,3
Acute idiopathic chilblains can develop between 12 to 24 hours after cold exposure. These lesions are often self-limited and will resolve within days to months.3 There is also a chronic form in which lesions wax and wane for many months as a result of repeated exposure to cold temperatures.1 In idiopathic chilblains, there are usually no other associated symptoms except for the characteristic cutaneous complaints.
Histopathology
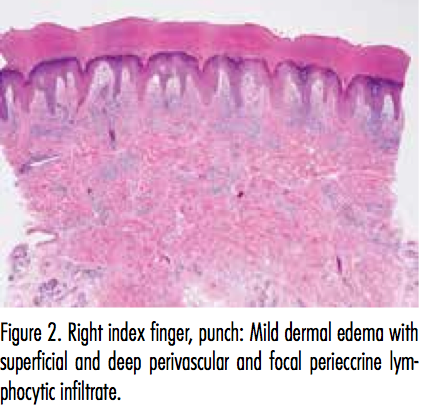
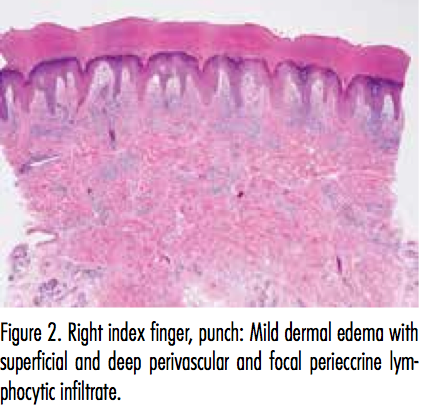
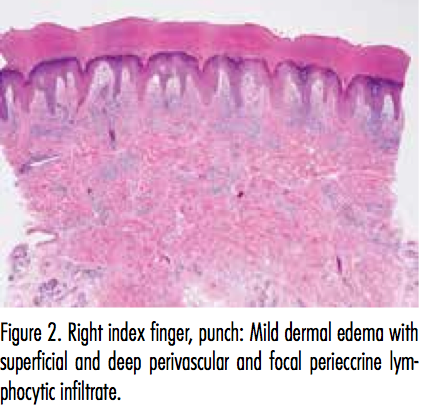
The histopathologic findings in idiopathic chilblains include a predominantly lymphocytic infiltrate with perivascular and perieccrine distribution, dermal edema and necrotic keratinocytes. Although controversial, some studies have asserted that the presence of a perieccrine inflammatory infiltrate in idiopathic chilblains can help distinguish it from the autoimmune lupus chilblains variant.8,9
Differential Diagnosis
The differential diagnosis of chilblains includes cryoglobulinemia, vasculitis, connective tissue disease, Raynaud’s phenomenon, frostbite and septic or cholesterol emboli.1,3,6 The distinction must be made between idiopathic and lupus chilblains because the latter can be associated with more severe cutaneous symptoms and systemic disease.1,9
Treatment
Idiopathic chilblains lesions are usually self-limiting and will resolve without treatment in 10 to 20 days.1 Patients are often managed conservatively. One of the key principles of therapy is to warm the affected areas and to protect them from the cold with gloves or socks during exposure to cool temperatures.1
The use of nifedipine may be helpful for severe or recurrent cases. One study showed that 7 out of 10 patients treated with 20 mg of nifedipine 3 times a day had lesions resolve within 10 days. None of the treated patients developed new lesions while taking the medication. Patients on nifedipine also reported decreased pain and irritation. The most common side effects reported were dizziness, flushing and headaches.11
Additionally, nifedipine has been used to treat pediatric patients with chilblains lesions.7 A retrospective study looking at patients between 6 months and 17 years old noted that nifedipine was efficacious in treating the more severe cases with marked acrocyanosis.12 Nifedipine is a calcium channel antagonist that has been shown to increase cutaneous blood flow following administration, which suggests that the vasodilator action may play a role in its treatment of chilblains.5,7,11-13 There is no evidence to support the use of topical steroids as treatment.
 Our Patient
Our Patient
A biopsy was taken of 1 of the lesions on her right index finger (Figure 2). Histologic examination demonstrated mild edema of the papillary dermis, few scattered dyskeratotic keratinocytes and a superficial and deep perivascular and focal perieccrine lymphocytic infiltrate. There was an absence of prominent vacuolar change and a colloidal iron stain failed to reveal significant mucin deposition. Significant dermal mucin deposition has been described in connective tissue disorders.
The above histological findings, along with a negative serum antinuclear antibody test favored the diagnosis of idiopathic chilblains. The patient was educated about the diagnosis and instructed to wear warm gloves and to avoid direct cold exposure to her hands as much as possible. Her lesions resolved several weeks later.
Conclusion
Idiopathic chilblains is a rather uncommon inflammatory disorder most often presenting as painful bilateral erythematous or purple papules found on the distal extremities upon exposure to non-freezing cold temperatures. It typically affects females and those with a lower BMI. The lesions are usually self-limiting and improve with warming the affected area and limiting cold exposure. Several studies support the use of nifedipine to treat severe and recurrent cases of idiopathic chilblains.5,7,11-13
Ms. Aronica is a medical student at Georgetown University School of Medicine in Washington, DC.
Dr. Aziz is a staff dermatologist at the Veterans Affairs Medical Center, department of dermatology, and assistant professor at Howard University College of Medicine, department of dermatology, in Washington, DC.
Disclosure: The authors report no relevant financial relationships.
References
1. Goette DK. Chilblains (perniosis). J Am Acad Dermatol. 1990;23(2 Pt 1):257-262.
2. Almahameed A, Pinto DS. Pernio (chilblains). Curr Treat Options Cardiovasc Med. 2008;10(2):128-135.
3. Prakash S, Weisman MH. Idiopathic chilblains. Am J Med. 2009;122(12):1152-1155.
4. Yang X, Perez OA, English JC 3rd. Adult perniosis and cryoglobulinemia: A retrospective study and review of the literature. J Am Acad Dermatol. 2010;62(6):e21-22.
5. Parlette EC, Parlette HL 3rd. Erythrocyanotic discoloration of the toes. Cutis. 2000;65(4):223-224, 226.
6. White KP, Roth MJ, Milanese A, Grant-Kels JM. Perniosis in association with anorexia nervosa. Pediatr Dermatiol. 1994;11(1):1-5.
7. Simon TD, Soep JB, Hollister, JR. Pernio in pediatrics. Pediatrics. 2005;116(3):e472-475.
8. Millarrd LG, Rowell NR. Chilblain lupus erythematosus (Hutchinson). A clinical and laboratory study of 17 patients. Br J Dermatol. 1978;98(5):497-506.
9. Boada A, Bielsa I, Fernandez-Figueras MT, Ferrandiz, C. Perniosis: clinical and histopathological analysis. Am J Dermatopathol. 2010;32(1):19-23.
10. Lee-Kirsch MA, Gong M, Schulz H, et al. Familial chilblain lupus, a monogenic form of cutaneous lupus erythematosus, maps to chromosome 3p. Am J Hum Genet. 2006:79(4):731-737.
11. Dowd P, Rustin M, Lanigan S. Nifedipine in the treatment of chilblains. Br Med J (Clin Res Ed). 1986:293(6552):923-924.
12. Larkins N, Murray KJ. Major cluster of chilblain cases in a cold dry Western Australian winter. J Paediatr Child Health. 2013;49(2):144-147.
13. Rustin M, Newton JA, Smith NP, Dowd PM. The treatment of chilblains with nifedipine: the results of a pilot study, a double-blind placebo-controlled randomized study and a long-term open trial. Br J Dermatol. 1989;120(2):267-275.
 A middle-aged woman without any significant past medical history presented with multiple discrete pink papules on the fingers of both of her hands that started 5 weeks prior to presentation. She was not taking any medications. She denied any fatigue, joint pains or fever. Physical examination revealed a thin, middle-aged woman. Her fingers demonstrated multiple 3 mm to 5 mm pink papules on a background of dusky erythema (Figure 1). There was no evidence of the eruption on her feet, legs, arms or trunk.
A middle-aged woman without any significant past medical history presented with multiple discrete pink papules on the fingers of both of her hands that started 5 weeks prior to presentation. She was not taking any medications. She denied any fatigue, joint pains or fever. Physical examination revealed a thin, middle-aged woman. Her fingers demonstrated multiple 3 mm to 5 mm pink papules on a background of dusky erythema (Figure 1). There was no evidence of the eruption on her feet, legs, arms or trunk.
Diagnosis: Idiopathic Chilblains
Jennifer C. Aronica, MS, and Nasir Aziz, MD
Chilblains, also referred to as pernio and perniosis, is an inflammatory disorder of acral skin that occurs on areas exposed to non-freezing temperatures. It can mimic vasculitis or thromboemboli and may lead to expensive diagnostic evaluations or inappropriate treatments when physicians are unfamiliar with its features.1
Chilblains was first seen in the damp and cold weather of western Europe.2 However, its occurrence in the northern United States is increasing, possibly as a result of a changing climate.
Epidemiology
Chilblains tends to occur more often in white young to middle age women during the winter and early spring months of November to April when it is damp and the temperature is above freezing. It has been proposed that humidity augments the chilling effect by enhancing thermal conductivity.3-5 Studies have also found an association between low body mass index (BMI) and chilblains, suggesting that these patients may develop the condition due to changes in their thermal regulation patterns.6
Chilblains has also been described in children and in teenagers diagnosed with anorexia nervosa, which could be related to their low BMI.6,7

Etiology
The exact pathogenesis of idiopathic chilblains is unknown. Studies have suggested that patients with chilblains have a continuous and prolonged cold-induced vasoconstriction, which leads to hypoxemia in the affected areas and an inflammatory reaction of the vessel wall.1,3
It is also important to distinguish idiopathic chilblains from that associated with an underlying autoimmune disease such as lupus erythematosus.8 This can be done by using the patient’s history, laboratory results and comparing the histopathological features on a cutaneous biopsy.
Patients with lupus chilblains tend to present at younger ages, have a known history of lupus erythematosus and are more likely to have positive antinuclear and/or anti-Ro/anti-La antibodies.9 A rare form of cutaneous lupus erythematosus has been described in the literature as familial chilblains lupus. This condition presents as inflammatory papules on acral areas, similar to that seen in idiopathic chilblains. A linkage analysis of a large German family with 18 affected individuals showed the locus for these familial lupus chilblains to map to chromosome 3p. Affected family members often showed evidence of antinuclear antibodies or immune complex formation.10
Clinical Findings
Idiopathic chilblains typically manifests as painful dusky erythematous or purple papules localized to acral areas of hands or feet that are associated with swelling and itching (Figure 1). The lesions are bilateral and there is a temporal association with exposure to non-freezing temperatures.1,3
Acute idiopathic chilblains can develop between 12 to 24 hours after cold exposure. These lesions are often self-limited and will resolve within days to months.3 There is also a chronic form in which lesions wax and wane for many months as a result of repeated exposure to cold temperatures.1 In idiopathic chilblains, there are usually no other associated symptoms except for the characteristic cutaneous complaints.
Histopathology
The histopathologic findings in idiopathic chilblains include a predominantly lymphocytic infiltrate with perivascular and perieccrine distribution, dermal edema and necrotic keratinocytes. Although controversial, some studies have asserted that the presence of a perieccrine inflammatory infiltrate in idiopathic chilblains can help distinguish it from the autoimmune lupus chilblains variant.8,9
Differential Diagnosis
The differential diagnosis of chilblains includes cryoglobulinemia, vasculitis, connective tissue disease, Raynaud’s phenomenon, frostbite and septic or cholesterol emboli.1,3,6 The distinction must be made between idiopathic and lupus chilblains because the latter can be associated with more severe cutaneous symptoms and systemic disease.1,9
Treatment
Idiopathic chilblains lesions are usually self-limiting and will resolve without treatment in 10 to 20 days.1 Patients are often managed conservatively. One of the key principles of therapy is to warm the affected areas and to protect them from the cold with gloves or socks during exposure to cool temperatures.1
The use of nifedipine may be helpful for severe or recurrent cases. One study showed that 7 out of 10 patients treated with 20 mg of nifedipine 3 times a day had lesions resolve within 10 days. None of the treated patients developed new lesions while taking the medication. Patients on nifedipine also reported decreased pain and irritation. The most common side effects reported were dizziness, flushing and headaches.11
Additionally, nifedipine has been used to treat pediatric patients with chilblains lesions.7 A retrospective study looking at patients between 6 months and 17 years old noted that nifedipine was efficacious in treating the more severe cases with marked acrocyanosis.12 Nifedipine is a calcium channel antagonist that has been shown to increase cutaneous blood flow following administration, which suggests that the vasodilator action may play a role in its treatment of chilblains.5,7,11-13 There is no evidence to support the use of topical steroids as treatment.
 Our Patient
Our Patient
A biopsy was taken of 1 of the lesions on her right index finger (Figure 2). Histologic examination demonstrated mild edema of the papillary dermis, few scattered dyskeratotic keratinocytes and a superficial and deep perivascular and focal perieccrine lymphocytic infiltrate. There was an absence of prominent vacuolar change and a colloidal iron stain failed to reveal significant mucin deposition. Significant dermal mucin deposition has been described in connective tissue disorders.
The above histological findings, along with a negative serum antinuclear antibody test favored the diagnosis of idiopathic chilblains. The patient was educated about the diagnosis and instructed to wear warm gloves and to avoid direct cold exposure to her hands as much as possible. Her lesions resolved several weeks later.
Conclusion
Idiopathic chilblains is a rather uncommon inflammatory disorder most often presenting as painful bilateral erythematous or purple papules found on the distal extremities upon exposure to non-freezing cold temperatures. It typically affects females and those with a lower BMI. The lesions are usually self-limiting and improve with warming the affected area and limiting cold exposure. Several studies support the use of nifedipine to treat severe and recurrent cases of idiopathic chilblains.5,7,11-13
Ms. Aronica is a medical student at Georgetown University School of Medicine in Washington, DC.
Dr. Aziz is a staff dermatologist at the Veterans Affairs Medical Center, department of dermatology, and assistant professor at Howard University College of Medicine, department of dermatology, in Washington, DC.
Disclosure: The authors report no relevant financial relationships.
References
1. Goette DK. Chilblains (perniosis). J Am Acad Dermatol. 1990;23(2 Pt 1):257-262.
2. Almahameed A, Pinto DS. Pernio (chilblains). Curr Treat Options Cardiovasc Med. 2008;10(2):128-135.
3. Prakash S, Weisman MH. Idiopathic chilblains. Am J Med. 2009;122(12):1152-1155.
4. Yang X, Perez OA, English JC 3rd. Adult perniosis and cryoglobulinemia: A retrospective study and review of the literature. J Am Acad Dermatol. 2010;62(6):e21-22.
5. Parlette EC, Parlette HL 3rd. Erythrocyanotic discoloration of the toes. Cutis. 2000;65(4):223-224, 226.
6. White KP, Roth MJ, Milanese A, Grant-Kels JM. Perniosis in association with anorexia nervosa. Pediatr Dermatiol. 1994;11(1):1-5.
7. Simon TD, Soep JB, Hollister, JR. Pernio in pediatrics. Pediatrics. 2005;116(3):e472-475.
8. Millarrd LG, Rowell NR. Chilblain lupus erythematosus (Hutchinson). A clinical and laboratory study of 17 patients. Br J Dermatol. 1978;98(5):497-506.
9. Boada A, Bielsa I, Fernandez-Figueras MT, Ferrandiz, C. Perniosis: clinical and histopathological analysis. Am J Dermatopathol. 2010;32(1):19-23.
10. Lee-Kirsch MA, Gong M, Schulz H, et al. Familial chilblain lupus, a monogenic form of cutaneous lupus erythematosus, maps to chromosome 3p. Am J Hum Genet. 2006:79(4):731-737.
11. Dowd P, Rustin M, Lanigan S. Nifedipine in the treatment of chilblains. Br Med J (Clin Res Ed). 1986:293(6552):923-924.
12. Larkins N, Murray KJ. Major cluster of chilblain cases in a cold dry Western Australian winter. J Paediatr Child Health. 2013;49(2):144-147.
13. Rustin M, Newton JA, Smith NP, Dowd PM. The treatment of chilblains with nifedipine: the results of a pilot study, a double-blind placebo-controlled randomized study and a long-term open trial. Br J Dermatol. 1989;120(2):267-275.
 A middle-aged woman without any significant past medical history presented with multiple discrete pink papules on the fingers of both of her hands that started 5 weeks prior to presentation. She was not taking any medications. She denied any fatigue, joint pains or fever. Physical examination revealed a thin, middle-aged woman. Her fingers demonstrated multiple 3 mm to 5 mm pink papules on a background of dusky erythema (Figure 1). There was no evidence of the eruption on her feet, legs, arms or trunk.
A middle-aged woman without any significant past medical history presented with multiple discrete pink papules on the fingers of both of her hands that started 5 weeks prior to presentation. She was not taking any medications. She denied any fatigue, joint pains or fever. Physical examination revealed a thin, middle-aged woman. Her fingers demonstrated multiple 3 mm to 5 mm pink papules on a background of dusky erythema (Figure 1). There was no evidence of the eruption on her feet, legs, arms or trunk.
,
 A middle-aged woman without any significant past medical history presented with multiple discrete pink papules on the fingers of both of her hands that started 5 weeks prior to presentation. She was not taking any medications. She denied any fatigue, joint pains or fever. Physical examination revealed a thin, middle-aged woman. Her fingers demonstrated multiple 3 mm to 5 mm pink papules on a background of dusky erythema (Figure 1). There was no evidence of the eruption on her feet, legs, arms or trunk.
A middle-aged woman without any significant past medical history presented with multiple discrete pink papules on the fingers of both of her hands that started 5 weeks prior to presentation. She was not taking any medications. She denied any fatigue, joint pains or fever. Physical examination revealed a thin, middle-aged woman. Her fingers demonstrated multiple 3 mm to 5 mm pink papules on a background of dusky erythema (Figure 1). There was no evidence of the eruption on her feet, legs, arms or trunk.
WHAT IS YOUR DIAGNOSIS?
To learn the answer, go to page 2
{{pagebreak}}
Diagnosis: Idiopathic Chilblains
Jennifer C. Aronica, MS, and Nasir Aziz, MD
Chilblains, also referred to as pernio and perniosis, is an inflammatory disorder of acral skin that occurs on areas exposed to non-freezing temperatures. It can mimic vasculitis or thromboemboli and may lead to expensive diagnostic evaluations or inappropriate treatments when physicians are unfamiliar with its features.1
Chilblains was first seen in the damp and cold weather of western Europe.2 However, its occurrence in the northern United States is increasing, possibly as a result of a changing climate.
Epidemiology
Chilblains tends to occur more often in white young to middle age women during the winter and early spring months of November to April when it is damp and the temperature is above freezing. It has been proposed that humidity augments the chilling effect by enhancing thermal conductivity.3-5 Studies have also found an association between low body mass index (BMI) and chilblains, suggesting that these patients may develop the condition due to changes in their thermal regulation patterns.6
Chilblains has also been described in children and in teenagers diagnosed with anorexia nervosa, which could be related to their low BMI.6,7

Etiology
The exact pathogenesis of idiopathic chilblains is unknown. Studies have suggested that patients with chilblains have a continuous and prolonged cold-induced vasoconstriction, which leads to hypoxemia in the affected areas and an inflammatory reaction of the vessel wall.1,3
It is also important to distinguish idiopathic chilblains from that associated with an underlying autoimmune disease such as lupus erythematosus.8 This can be done by using the patient’s history, laboratory results and comparing the histopathological features on a cutaneous biopsy.
Patients with lupus chilblains tend to present at younger ages, have a known history of lupus erythematosus and are more likely to have positive antinuclear and/or anti-Ro/anti-La antibodies.9 A rare form of cutaneous lupus erythematosus has been described in the literature as familial chilblains lupus. This condition presents as inflammatory papules on acral areas, similar to that seen in idiopathic chilblains. A linkage analysis of a large German family with 18 affected individuals showed the locus for these familial lupus chilblains to map to chromosome 3p. Affected family members often showed evidence of antinuclear antibodies or immune complex formation.10
Clinical Findings
Idiopathic chilblains typically manifests as painful dusky erythematous or purple papules localized to acral areas of hands or feet that are associated with swelling and itching (Figure 1). The lesions are bilateral and there is a temporal association with exposure to non-freezing temperatures.1,3
Acute idiopathic chilblains can develop between 12 to 24 hours after cold exposure. These lesions are often self-limited and will resolve within days to months.3 There is also a chronic form in which lesions wax and wane for many months as a result of repeated exposure to cold temperatures.1 In idiopathic chilblains, there are usually no other associated symptoms except for the characteristic cutaneous complaints.
Histopathology
The histopathologic findings in idiopathic chilblains include a predominantly lymphocytic infiltrate with perivascular and perieccrine distribution, dermal edema and necrotic keratinocytes. Although controversial, some studies have asserted that the presence of a perieccrine inflammatory infiltrate in idiopathic chilblains can help distinguish it from the autoimmune lupus chilblains variant.8,9
Differential Diagnosis
The differential diagnosis of chilblains includes cryoglobulinemia, vasculitis, connective tissue disease, Raynaud’s phenomenon, frostbite and septic or cholesterol emboli.1,3,6 The distinction must be made between idiopathic and lupus chilblains because the latter can be associated with more severe cutaneous symptoms and systemic disease.1,9
Treatment
Idiopathic chilblains lesions are usually self-limiting and will resolve without treatment in 10 to 20 days.1 Patients are often managed conservatively. One of the key principles of therapy is to warm the affected areas and to protect them from the cold with gloves or socks during exposure to cool temperatures.1
The use of nifedipine may be helpful for severe or recurrent cases. One study showed that 7 out of 10 patients treated with 20 mg of nifedipine 3 times a day had lesions resolve within 10 days. None of the treated patients developed new lesions while taking the medication. Patients on nifedipine also reported decreased pain and irritation. The most common side effects reported were dizziness, flushing and headaches.11
Additionally, nifedipine has been used to treat pediatric patients with chilblains lesions.7 A retrospective study looking at patients between 6 months and 17 years old noted that nifedipine was efficacious in treating the more severe cases with marked acrocyanosis.12 Nifedipine is a calcium channel antagonist that has been shown to increase cutaneous blood flow following administration, which suggests that the vasodilator action may play a role in its treatment of chilblains.5,7,11-13 There is no evidence to support the use of topical steroids as treatment.
 Our Patient
Our Patient
A biopsy was taken of 1 of the lesions on her right index finger (Figure 2). Histologic examination demonstrated mild edema of the papillary dermis, few scattered dyskeratotic keratinocytes and a superficial and deep perivascular and focal perieccrine lymphocytic infiltrate. There was an absence of prominent vacuolar change and a colloidal iron stain failed to reveal significant mucin deposition. Significant dermal mucin deposition has been described in connective tissue disorders.
The above histological findings, along with a negative serum antinuclear antibody test favored the diagnosis of idiopathic chilblains. The patient was educated about the diagnosis and instructed to wear warm gloves and to avoid direct cold exposure to her hands as much as possible. Her lesions resolved several weeks later.
Conclusion
Idiopathic chilblains is a rather uncommon inflammatory disorder most often presenting as painful bilateral erythematous or purple papules found on the distal extremities upon exposure to non-freezing cold temperatures. It typically affects females and those with a lower BMI. The lesions are usually self-limiting and improve with warming the affected area and limiting cold exposure. Several studies support the use of nifedipine to treat severe and recurrent cases of idiopathic chilblains.5,7,11-13
Ms. Aronica is a medical student at Georgetown University School of Medicine in Washington, DC.
Dr. Aziz is a staff dermatologist at the Veterans Affairs Medical Center, department of dermatology, and assistant professor at Howard University College of Medicine, department of dermatology, in Washington, DC.
Disclosure: The authors report no relevant financial relationships.
References
1. Goette DK. Chilblains (perniosis). J Am Acad Dermatol. 1990;23(2 Pt 1):257-262.
2. Almahameed A, Pinto DS. Pernio (chilblains). Curr Treat Options Cardiovasc Med. 2008;10(2):128-135.
3. Prakash S, Weisman MH. Idiopathic chilblains. Am J Med. 2009;122(12):1152-1155.
4. Yang X, Perez OA, English JC 3rd. Adult perniosis and cryoglobulinemia: A retrospective study and review of the literature. J Am Acad Dermatol. 2010;62(6):e21-22.
5. Parlette EC, Parlette HL 3rd. Erythrocyanotic discoloration of the toes. Cutis. 2000;65(4):223-224, 226.
6. White KP, Roth MJ, Milanese A, Grant-Kels JM. Perniosis in association with anorexia nervosa. Pediatr Dermatiol. 1994;11(1):1-5.
7. Simon TD, Soep JB, Hollister, JR. Pernio in pediatrics. Pediatrics. 2005;116(3):e472-475.
8. Millarrd LG, Rowell NR. Chilblain lupus erythematosus (Hutchinson). A clinical and laboratory study of 17 patients. Br J Dermatol. 1978;98(5):497-506.
9. Boada A, Bielsa I, Fernandez-Figueras MT, Ferrandiz, C. Perniosis: clinical and histopathological analysis. Am J Dermatopathol. 2010;32(1):19-23.
10. Lee-Kirsch MA, Gong M, Schulz H, et al. Familial chilblain lupus, a monogenic form of cutaneous lupus erythematosus, maps to chromosome 3p. Am J Hum Genet. 2006:79(4):731-737.
11. Dowd P, Rustin M, Lanigan S. Nifedipine in the treatment of chilblains. Br Med J (Clin Res Ed). 1986:293(6552):923-924.
12. Larkins N, Murray KJ. Major cluster of chilblain cases in a cold dry Western Australian winter. J Paediatr Child Health. 2013;49(2):144-147.
13. Rustin M, Newton JA, Smith NP, Dowd PM. The treatment of chilblains with nifedipine: the results of a pilot study, a double-blind placebo-controlled randomized study and a long-term open trial. Br J Dermatol. 1989;120(2):267-275.
 A middle-aged woman without any significant past medical history presented with multiple discrete pink papules on the fingers of both of her hands that started 5 weeks prior to presentation. She was not taking any medications. She denied any fatigue, joint pains or fever. Physical examination revealed a thin, middle-aged woman. Her fingers demonstrated multiple 3 mm to 5 mm pink papules on a background of dusky erythema (Figure 1). There was no evidence of the eruption on her feet, legs, arms or trunk.
A middle-aged woman without any significant past medical history presented with multiple discrete pink papules on the fingers of both of her hands that started 5 weeks prior to presentation. She was not taking any medications. She denied any fatigue, joint pains or fever. Physical examination revealed a thin, middle-aged woman. Her fingers demonstrated multiple 3 mm to 5 mm pink papules on a background of dusky erythema (Figure 1). There was no evidence of the eruption on her feet, legs, arms or trunk.
Diagnosis: Idiopathic Chilblains
Jennifer C. Aronica, MS, and Nasir Aziz, MD
Chilblains, also referred to as pernio and perniosis, is an inflammatory disorder of acral skin that occurs on areas exposed to non-freezing temperatures. It can mimic vasculitis or thromboemboli and may lead to expensive diagnostic evaluations or inappropriate treatments when physicians are unfamiliar with its features.1
Chilblains was first seen in the damp and cold weather of western Europe.2 However, its occurrence in the northern United States is increasing, possibly as a result of a changing climate.
Epidemiology
Chilblains tends to occur more often in white young to middle age women during the winter and early spring months of November to April when it is damp and the temperature is above freezing. It has been proposed that humidity augments the chilling effect by enhancing thermal conductivity.3-5 Studies have also found an association between low body mass index (BMI) and chilblains, suggesting that these patients may develop the condition due to changes in their thermal regulation patterns.6
Chilblains has also been described in children and in teenagers diagnosed with anorexia nervosa, which could be related to their low BMI.6,7

Etiology
The exact pathogenesis of idiopathic chilblains is unknown. Studies have suggested that patients with chilblains have a continuous and prolonged cold-induced vasoconstriction, which leads to hypoxemia in the affected areas and an inflammatory reaction of the vessel wall.1,3
It is also important to distinguish idiopathic chilblains from that associated with an underlying autoimmune disease such as lupus erythematosus.8 This can be done by using the patient’s history, laboratory results and comparing the histopathological features on a cutaneous biopsy.
Patients with lupus chilblains tend to present at younger ages, have a known history of lupus erythematosus and are more likely to have positive antinuclear and/or anti-Ro/anti-La antibodies.9 A rare form of cutaneous lupus erythematosus has been described in the literature as familial chilblains lupus. This condition presents as inflammatory papules on acral areas, similar to that seen in idiopathic chilblains. A linkage analysis of a large German family with 18 affected individuals showed the locus for these familial lupus chilblains to map to chromosome 3p. Affected family members often showed evidence of antinuclear antibodies or immune complex formation.10
Clinical Findings
Idiopathic chilblains typically manifests as painful dusky erythematous or purple papules localized to acral areas of hands or feet that are associated with swelling and itching (Figure 1). The lesions are bilateral and there is a temporal association with exposure to non-freezing temperatures.1,3
Acute idiopathic chilblains can develop between 12 to 24 hours after cold exposure. These lesions are often self-limited and will resolve within days to months.3 There is also a chronic form in which lesions wax and wane for many months as a result of repeated exposure to cold temperatures.1 In idiopathic chilblains, there are usually no other associated symptoms except for the characteristic cutaneous complaints.
Histopathology
The histopathologic findings in idiopathic chilblains include a predominantly lymphocytic infiltrate with perivascular and perieccrine distribution, dermal edema and necrotic keratinocytes. Although controversial, some studies have asserted that the presence of a perieccrine inflammatory infiltrate in idiopathic chilblains can help distinguish it from the autoimmune lupus chilblains variant.8,9
Differential Diagnosis
The differential diagnosis of chilblains includes cryoglobulinemia, vasculitis, connective tissue disease, Raynaud’s phenomenon, frostbite and septic or cholesterol emboli.1,3,6 The distinction must be made between idiopathic and lupus chilblains because the latter can be associated with more severe cutaneous symptoms and systemic disease.1,9
Treatment
Idiopathic chilblains lesions are usually self-limiting and will resolve without treatment in 10 to 20 days.1 Patients are often managed conservatively. One of the key principles of therapy is to warm the affected areas and to protect them from the cold with gloves or socks during exposure to cool temperatures.1
The use of nifedipine may be helpful for severe or recurrent cases. One study showed that 7 out of 10 patients treated with 20 mg of nifedipine 3 times a day had lesions resolve within 10 days. None of the treated patients developed new lesions while taking the medication. Patients on nifedipine also reported decreased pain and irritation. The most common side effects reported were dizziness, flushing and headaches.11
Additionally, nifedipine has been used to treat pediatric patients with chilblains lesions.7 A retrospective study looking at patients between 6 months and 17 years old noted that nifedipine was efficacious in treating the more severe cases with marked acrocyanosis.12 Nifedipine is a calcium channel antagonist that has been shown to increase cutaneous blood flow following administration, which suggests that the vasodilator action may play a role in its treatment of chilblains.5,7,11-13 There is no evidence to support the use of topical steroids as treatment.
 Our Patient
Our Patient
A biopsy was taken of 1 of the lesions on her right index finger (Figure 2). Histologic examination demonstrated mild edema of the papillary dermis, few scattered dyskeratotic keratinocytes and a superficial and deep perivascular and focal perieccrine lymphocytic infiltrate. There was an absence of prominent vacuolar change and a colloidal iron stain failed to reveal significant mucin deposition. Significant dermal mucin deposition has been described in connective tissue disorders.
The above histological findings, along with a negative serum antinuclear antibody test favored the diagnosis of idiopathic chilblains. The patient was educated about the diagnosis and instructed to wear warm gloves and to avoid direct cold exposure to her hands as much as possible. Her lesions resolved several weeks later.
Conclusion
Idiopathic chilblains is a rather uncommon inflammatory disorder most often presenting as painful bilateral erythematous or purple papules found on the distal extremities upon exposure to non-freezing cold temperatures. It typically affects females and those with a lower BMI. The lesions are usually self-limiting and improve with warming the affected area and limiting cold exposure. Several studies support the use of nifedipine to treat severe and recurrent cases of idiopathic chilblains.5,7,11-13
Ms. Aronica is a medical student at Georgetown University School of Medicine in Washington, DC.
Dr. Aziz is a staff dermatologist at the Veterans Affairs Medical Center, department of dermatology, and assistant professor at Howard University College of Medicine, department of dermatology, in Washington, DC.
Disclosure: The authors report no relevant financial relationships.
References
1. Goette DK. Chilblains (perniosis). J Am Acad Dermatol. 1990;23(2 Pt 1):257-262.
2. Almahameed A, Pinto DS. Pernio (chilblains). Curr Treat Options Cardiovasc Med. 2008;10(2):128-135.
3. Prakash S, Weisman MH. Idiopathic chilblains. Am J Med. 2009;122(12):1152-1155.
4. Yang X, Perez OA, English JC 3rd. Adult perniosis and cryoglobulinemia: A retrospective study and review of the literature. J Am Acad Dermatol. 2010;62(6):e21-22.
5. Parlette EC, Parlette HL 3rd. Erythrocyanotic discoloration of the toes. Cutis. 2000;65(4):223-224, 226.
6. White KP, Roth MJ, Milanese A, Grant-Kels JM. Perniosis in association with anorexia nervosa. Pediatr Dermatiol. 1994;11(1):1-5.
7. Simon TD, Soep JB, Hollister, JR. Pernio in pediatrics. Pediatrics. 2005;116(3):e472-475.
8. Millarrd LG, Rowell NR. Chilblain lupus erythematosus (Hutchinson). A clinical and laboratory study of 17 patients. Br J Dermatol. 1978;98(5):497-506.
9. Boada A, Bielsa I, Fernandez-Figueras MT, Ferrandiz, C. Perniosis: clinical and histopathological analysis. Am J Dermatopathol. 2010;32(1):19-23.
10. Lee-Kirsch MA, Gong M, Schulz H, et al. Familial chilblain lupus, a monogenic form of cutaneous lupus erythematosus, maps to chromosome 3p. Am J Hum Genet. 2006:79(4):731-737.
11. Dowd P, Rustin M, Lanigan S. Nifedipine in the treatment of chilblains. Br Med J (Clin Res Ed). 1986:293(6552):923-924.
12. Larkins N, Murray KJ. Major cluster of chilblain cases in a cold dry Western Australian winter. J Paediatr Child Health. 2013;49(2):144-147.
13. Rustin M, Newton JA, Smith NP, Dowd PM. The treatment of chilblains with nifedipine: the results of a pilot study, a double-blind placebo-controlled randomized study and a long-term open trial. Br J Dermatol. 1989;120(2):267-275.
Diagnosis: Idiopathic Chilblains
Jennifer C. Aronica, MS, and Nasir Aziz, MD
Chilblains, also referred to as pernio and perniosis, is an inflammatory disorder of acral skin that occurs on areas exposed to non-freezing temperatures. It can mimic vasculitis or thromboemboli and may lead to expensive diagnostic evaluations or inappropriate treatments when physicians are unfamiliar with its features.1
Chilblains was first seen in the damp and cold weather of western Europe.2 However, its occurrence in the northern United States is increasing, possibly as a result of a changing climate.
Epidemiology
Chilblains tends to occur more often in white young to middle age women during the winter and early spring months of November to April when it is damp and the temperature is above freezing. It has been proposed that humidity augments the chilling effect by enhancing thermal conductivity.3-5 Studies have also found an association between low body mass index (BMI) and chilblains, suggesting that these patients may develop the condition due to changes in their thermal regulation patterns.6
Chilblains has also been described in children and in teenagers diagnosed with anorexia nervosa, which could be related to their low BMI.6,7

Etiology
The exact pathogenesis of idiopathic chilblains is unknown. Studies have suggested that patients with chilblains have a continuous and prolonged cold-induced vasoconstriction, which leads to hypoxemia in the affected areas and an inflammatory reaction of the vessel wall.1,3
It is also important to distinguish idiopathic chilblains from that associated with an underlying autoimmune disease such as lupus erythematosus.8 This can be done by using the patient’s history, laboratory results and comparing the histopathological features on a cutaneous biopsy.
Patients with lupus chilblains tend to present at younger ages, have a known history of lupus erythematosus and are more likely to have positive antinuclear and/or anti-Ro/anti-La antibodies.9 A rare form of cutaneous lupus erythematosus has been described in the literature as familial chilblains lupus. This condition presents as inflammatory papules on acral areas, similar to that seen in idiopathic chilblains. A linkage analysis of a large German family with 18 affected individuals showed the locus for these familial lupus chilblains to map to chromosome 3p. Affected family members often showed evidence of antinuclear antibodies or immune complex formation.10
Clinical Findings
Idiopathic chilblains typically manifests as painful dusky erythematous or purple papules localized to acral areas of hands or feet that are associated with swelling and itching (Figure 1). The lesions are bilateral and there is a temporal association with exposure to non-freezing temperatures.1,3
Acute idiopathic chilblains can develop between 12 to 24 hours after cold exposure. These lesions are often self-limited and will resolve within days to months.3 There is also a chronic form in which lesions wax and wane for many months as a result of repeated exposure to cold temperatures.1 In idiopathic chilblains, there are usually no other associated symptoms except for the characteristic cutaneous complaints.
Histopathology
The histopathologic findings in idiopathic chilblains include a predominantly lymphocytic infiltrate with perivascular and perieccrine distribution, dermal edema and necrotic keratinocytes. Although controversial, some studies have asserted that the presence of a perieccrine inflammatory infiltrate in idiopathic chilblains can help distinguish it from the autoimmune lupus chilblains variant.8,9
Differential Diagnosis
The differential diagnosis of chilblains includes cryoglobulinemia, vasculitis, connective tissue disease, Raynaud’s phenomenon, frostbite and septic or cholesterol emboli.1,3,6 The distinction must be made between idiopathic and lupus chilblains because the latter can be associated with more severe cutaneous symptoms and systemic disease.1,9
Treatment
Idiopathic chilblains lesions are usually self-limiting and will resolve without treatment in 10 to 20 days.1 Patients are often managed conservatively. One of the key principles of therapy is to warm the affected areas and to protect them from the cold with gloves or socks during exposure to cool temperatures.1
The use of nifedipine may be helpful for severe or recurrent cases. One study showed that 7 out of 10 patients treated with 20 mg of nifedipine 3 times a day had lesions resolve within 10 days. None of the treated patients developed new lesions while taking the medication. Patients on nifedipine also reported decreased pain and irritation. The most common side effects reported were dizziness, flushing and headaches.11
Additionally, nifedipine has been used to treat pediatric patients with chilblains lesions.7 A retrospective study looking at patients between 6 months and 17 years old noted that nifedipine was efficacious in treating the more severe cases with marked acrocyanosis.12 Nifedipine is a calcium channel antagonist that has been shown to increase cutaneous blood flow following administration, which suggests that the vasodilator action may play a role in its treatment of chilblains.5,7,11-13 There is no evidence to support the use of topical steroids as treatment.
 Our Patient
Our Patient
A biopsy was taken of 1 of the lesions on her right index finger (Figure 2). Histologic examination demonstrated mild edema of the papillary dermis, few scattered dyskeratotic keratinocytes and a superficial and deep perivascular and focal perieccrine lymphocytic infiltrate. There was an absence of prominent vacuolar change and a colloidal iron stain failed to reveal significant mucin deposition. Significant dermal mucin deposition has been described in connective tissue disorders.
The above histological findings, along with a negative serum antinuclear antibody test favored the diagnosis of idiopathic chilblains. The patient was educated about the diagnosis and instructed to wear warm gloves and to avoid direct cold exposure to her hands as much as possible. Her lesions resolved several weeks later.
Conclusion
Idiopathic chilblains is a rather uncommon inflammatory disorder most often presenting as painful bilateral erythematous or purple papules found on the distal extremities upon exposure to non-freezing cold temperatures. It typically affects females and those with a lower BMI. The lesions are usually self-limiting and improve with warming the affected area and limiting cold exposure. Several studies support the use of nifedipine to treat severe and recurrent cases of idiopathic chilblains.5,7,11-13
Ms. Aronica is a medical student at Georgetown University School of Medicine in Washington, DC.
Dr. Aziz is a staff dermatologist at the Veterans Affairs Medical Center, department of dermatology, and assistant professor at Howard University College of Medicine, department of dermatology, in Washington, DC.
Disclosure: The authors report no relevant financial relationships.
References
1. Goette DK. Chilblains (perniosis). J Am Acad Dermatol. 1990;23(2 Pt 1):257-262.
2. Almahameed A, Pinto DS. Pernio (chilblains). Curr Treat Options Cardiovasc Med. 2008;10(2):128-135.
3. Prakash S, Weisman MH. Idiopathic chilblains. Am J Med. 2009;122(12):1152-1155.
4. Yang X, Perez OA, English JC 3rd. Adult perniosis and cryoglobulinemia: A retrospective study and review of the literature. J Am Acad Dermatol. 2010;62(6):e21-22.
5. Parlette EC, Parlette HL 3rd. Erythrocyanotic discoloration of the toes. Cutis. 2000;65(4):223-224, 226.
6. White KP, Roth MJ, Milanese A, Grant-Kels JM. Perniosis in association with anorexia nervosa. Pediatr Dermatiol. 1994;11(1):1-5.
7. Simon TD, Soep JB, Hollister, JR. Pernio in pediatrics. Pediatrics. 2005;116(3):e472-475.
8. Millarrd LG, Rowell NR. Chilblain lupus erythematosus (Hutchinson). A clinical and laboratory study of 17 patients. Br J Dermatol. 1978;98(5):497-506.
9. Boada A, Bielsa I, Fernandez-Figueras MT, Ferrandiz, C. Perniosis: clinical and histopathological analysis. Am J Dermatopathol. 2010;32(1):19-23.
10. Lee-Kirsch MA, Gong M, Schulz H, et al. Familial chilblain lupus, a monogenic form of cutaneous lupus erythematosus, maps to chromosome 3p. Am J Hum Genet. 2006:79(4):731-737.
11. Dowd P, Rustin M, Lanigan S. Nifedipine in the treatment of chilblains. Br Med J (Clin Res Ed). 1986:293(6552):923-924.
12. Larkins N, Murray KJ. Major cluster of chilblain cases in a cold dry Western Australian winter. J Paediatr Child Health. 2013;49(2):144-147.
13. Rustin M, Newton JA, Smith NP, Dowd PM. The treatment of chilblains with nifedipine: the results of a pilot study, a double-blind placebo-controlled randomized study and a long-term open trial. Br J Dermatol. 1989;120(2):267-275.
 A middle-aged woman without any significant past medical history presented with multiple discrete pink papules on the fingers of both of her hands that started 5 weeks prior to presentation. She was not taking any medications. She denied any fatigue, joint pains or fever. Physical examination revealed a thin, middle-aged woman. Her fingers demonstrated multiple 3 mm to 5 mm pink papules on a background of dusky erythema (Figure 1). There was no evidence of the eruption on her feet, legs, arms or trunk.
A middle-aged woman without any significant past medical history presented with multiple discrete pink papules on the fingers of both of her hands that started 5 weeks prior to presentation. She was not taking any medications. She denied any fatigue, joint pains or fever. Physical examination revealed a thin, middle-aged woman. Her fingers demonstrated multiple 3 mm to 5 mm pink papules on a background of dusky erythema (Figure 1). There was no evidence of the eruption on her feet, legs, arms or trunk. 





 A middle-aged woman without any significant past medical history presented with multiple discrete pink papules on the fingers of both of her hands that started 5 weeks prior to presentation. She was not taking any medications. She denied any fatigue, joint pains or fever. Physical examination revealed a thin, middle-aged woman. Her fingers demonstrated multiple 3 mm to 5 mm pink papules on a background of dusky erythema (Figure 1). There was no evidence of the eruption on her feet, legs, arms or trunk.
A middle-aged woman without any significant past medical history presented with multiple discrete pink papules on the fingers of both of her hands that started 5 weeks prior to presentation. She was not taking any medications. She denied any fatigue, joint pains or fever. Physical examination revealed a thin, middle-aged woman. Her fingers demonstrated multiple 3 mm to 5 mm pink papules on a background of dusky erythema (Figure 1). There was no evidence of the eruption on her feet, legs, arms or trunk. 
 Our Patient
Our Patient
 Our Patient
Our Patient

















