The Rise of the Machine: Can Artificial Intelligence Impact Wound Care Outcomes?
Over the past several years, artificial intelligence (AI)-based innovation in the medical field has emerged, including in various types of imaging. How might such technology apply to the field of wound care? In this edition of the Wound Care Q & A column, the panelists share their experiences and thoughts on if AI could bring a new era of improved outcomes.
Q: Many clinics still use manual ruler-based wound measurements even though research suggests this method is subject to high variability.1,2 What, if any, technologies are you using to obtain wound photographs and measurements?
A:
Barbara Aung, DPM, DABPM, CWS, FAPWHc has experience using many different methods of wound measurement. These methods range from Silhouette (Aranz Medical), which she says is often used in clinical trial settings, to a plain digital camera and software (PictZar) that can load images and measure digitally.
“More recently I have used the imaging and measurement process available with the MolecuLight imaging device,” she continues. “It provides length and width, but you still have to measure the depth independently. I have also tried WoundZoom (Perceptive) in the past, which is similar to Aranz.”
Dr. Aung also points out that there are apps, such as Minuteful for Wounds (Healthy.io), that one can use with a cell phone.
Eric J. Lullove, DPM, CWSP, DABLES, FAPWHc adds that his clinic no longer uses manual ruler-based wound measurements, and instead relies on digital-based measurements.
“The technology that we utilize is spatial 3D camera tech with imbedded AI to measure wound parameters,” he explains.
Matthew Garoufalis, DPM, FASPS, FACPM, CWS relates that, with new AI imaging models, such as spatial frequency domain imaging (SFDI) and near-infrared spectroscopy (NIRS), clinicians can not only measure wounds with more exactness than before, but that the results are reproducible and consistent with each visit, even though the provider may be different.
“These devices allow for full wound volume measurement, instead of guessing at length and width as well as depth,” he says. “The wound is always oriented in the same way on each visit, resulting in consistent measurement of wound volume and tracking of wound healing progress.”
Brian Lepow, DPM, DABPM agrees, and adds that some of the variability in manual wound measurement may relate to changes in trajectory of wounds week over week. Similar to Dr. Aung, Dr. Lepow has used the Silhouette Camera by Aranz at his institution.
“This system captures a 3D image of the wound, which not only provides a length-to-width ratio, but also can provide a topographical evaluation of the wound, removing human error,” he says.
Q: Currently there is no standard wound tissue assessment method. However, new AI technologies can enable automated analysis of diagnostic images. Can you share your experience utilizing advanced wound imaging devices and software in your practice?
A:
Dr. Garoufalis shares that because of such technology, not only can clinicians obtain more reliable wound measurements, helping to assess wound progress, but they also get other valuable information. This includes, but is not limited to, wound perfusion, hemoglobin distribution and oxygenation biomarkers.
“This allows us to better understand what is happening below and around the wound that we are trying to heal,” he explains. “With this information we can make better decisions about what products to use that will be the best at assisting wound closure.”
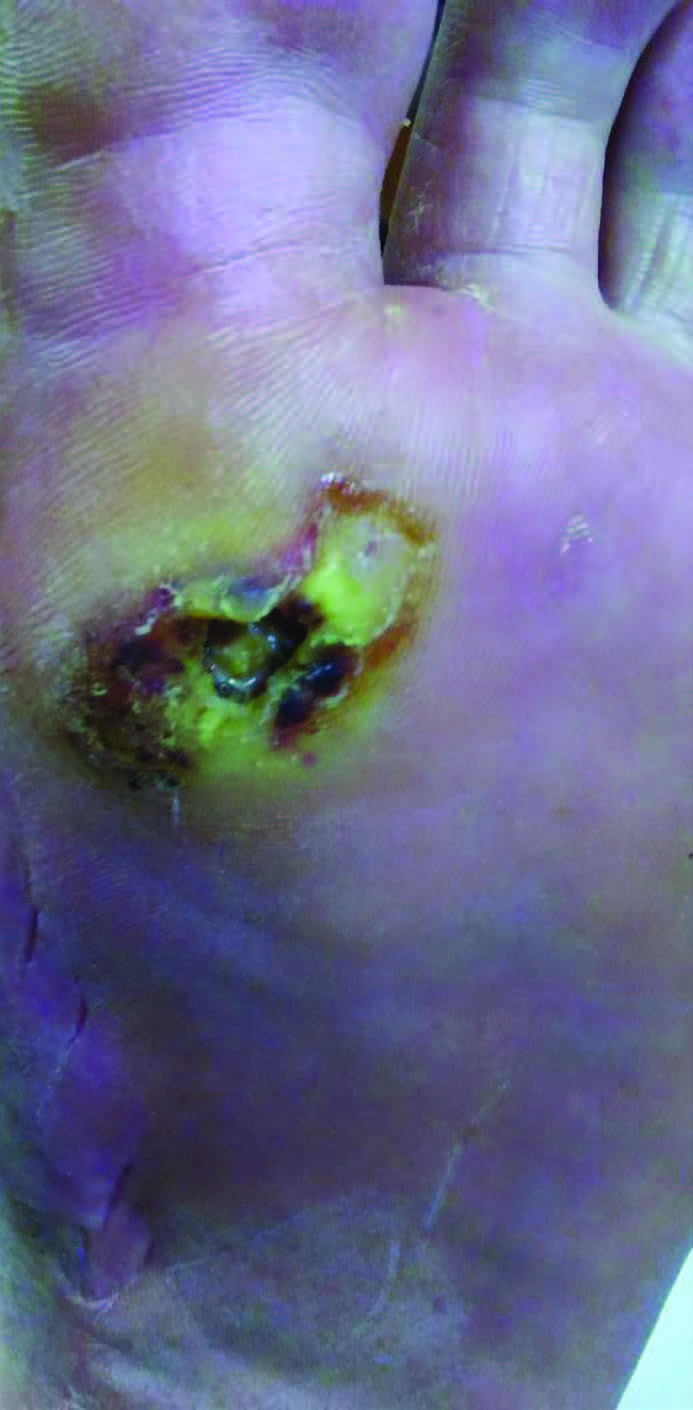
Dr. Aung shares that she has experience using MolecuLight imaging, which looks at bacteria presence in the wound that may prevent progression, as well with NIRS technology looking at tissue oxygenation and blood flow to assess wound healing potential.
Over the years, there has been exceptional development in the industry with regard to these technologies, from Visitrak (Smith + Nephew) to newer systems such as MolecuLight, says Dr. Lullove.
“I think the most advantageous experience is for any wound center/clinic to adopt one or more of these technologies to help improve outcomes,” he says. “Being able to digitally track the progression of healing (or non-healing) is vital in the health care economy of wound care. The stratification of outcome-based payments is on the cusp of becoming reality and the “old” way of wound management just is not going to remain viable without one of these advanced imaging technologies.”

Q: What additional trends in AI have you seen in the wound care space that might influence best clinical practices in the future?
A:
Dr. Lullove says that the AI-based wound care space continues to evolve, with programs such as eKare, Moleculight, Kent Imaging, Modulim, etc.
“The way that one can influence best clinical practice will be about continued submission of claims data to payors and the continued need for advanced level 1 research in this space,” he adds.
Dr. Lepow echoes that such technology may play a role in multiple aspects of wound care, including ulcer prediction, surgical decision making, vascular assessment and timing of application of skin substitutes.
In his experience, Dr. Garoufalis feels that AI now allows clinicians to see what is happening beyond what one can see with the naked eye. With this additional information, providers can make better decisions about how to best treat chronic wounds and speed wound closure.
“This can only improve our best clinical practices in the future,” he says. “AI is already used in cancer detection and in dermatology. Wound care is a logical and practical use of this tool.”
Dr. Aung shares that she is eager to try some of the newer options available, including smart wound dressings with sensors and wearable technologies.
“I feel these will become more prevalent in everyday life, and will ultimately translate into advances in wound care,” she adds.

Q: In your experience, has the adoption of these innovative technologies led to an overall cost savings or improved patient outcomes?
A:
Dr. Aung points out that in some cases, a roadblock in implementing these technologies is the cost associated with acquiring them, and a potential lack of reimbursement available for these devices.
“I do feel that technological innovation can lead to cost savings, which reflect in the preliminary outcomes I have reached using the MolecuLight imaging device, which I presented at two conferences in 2019.3,4 I found this technology could help to show when a wound might be ready for using tissue allografts by determining bacteria presence in quantities that may inhibit healing. This is both a cost savings to patients and to the health care system, which then leads to improved patient outcomes.”
She goes on to say that she has used such technology under both clinical trial and reimbursement review settings, and that billing for these devices and services can prove challenging, in her experience. She adds that if HCPCS codes are recently assigned or are in experimental or trial modes, that affordability in a private practice setting can be discouraging. But, she also notes hospital systems or universities may not face those same hurdles.
Overall, Dr. Lullove does think that use of AI technologies both saves in cost and improves patient outcomes. He relates that the need for technology to assist in documentation of progression of wound healing, imaging of bacterial loads in tissue or to use spectroscopy to identify vascular perfusion is paramount in these cases to succeed.
“While these technologies are not weekly, ‘all-the-time’ on every visit, they do achieve the unmet need of documenting areas of wound management in difficult-to-treat patient populations to help oversee and direct care decisions,” he says.
Dr. Lepow adds that, in his current experience with the use of these technologies, he does believe they are improving patient outcomes by reducing human error and allowing computer-based technologies to help assist in the most advanced care possible.
“Early assessment leading to more rapid management of a problem will lead to better patient outcomes and in turn will translate to a cost savings across the entire system of care,” he says.
Dr. Garoufalis stresses that, in his opinion, AI-based technology could be a game changer for wound care.
“Without a doubt, these new technologies will and do lead to better patient outcomes which in turn lead to overall cost savings,” he explains. “This is what the payors are asking for, but the challenge is getting them to understand that the investment in this new technology up front, will lead to better cost savings and improved patient outcomes in the long run. It really is a true win-win.”

Dr. Cole is the Director of Wound Care Research at Kent State University College of Podiatric Medicine and is the Director of Professional Development and Clinical Education for Woundtech. She is board certified by the American Board of Foot and Ankle Surgery and the American Board of Wound Management. Dr. Cole is a Fellow of the Academy of Physicians in Wound Healing.
Dr. Aung is Chief of the Podiatry Section of the Tenet Health System/St. Joseph’s Hospital in Tucson, Ariz. She is a member of the APMA Coding Committee, the APMA MACRA/MIPS Task Force and is on the Exam Committee of the American Board of Wound Management. Dr. Aung is also on the Editorial Review Board for Wound Management and Prevention.
Dr. Lepow is an Assistant Professor of Surgery in the Division of Vascular Surgery and Endovascular Therapy at The Baylor College of Medicine in Houston, TX. He is a Diplomate of the American Board of Podiatric Medicine, holding a certificate of added qualification in Amputation Prevention and Wound Care. Dr. Lepow is a member of the Board of Directors for the American Board of Podiatric Medicine and is the Founding Treasurer of the American Limb Preservation Society (ALPS). Dr. Lepow discloses that he is a consultant for Kent Imaging.
Dr. Lullove is in private practice in Coconut Creek, FL. He is the Chief Medical Officer of the West Boca Center for Wound Healing, the WHS Liaison to the Alliance of Wound Care Stakeholders, and is a committee member of the FDA Wound Care Community Collaborative. He also serves on the exam committee of the American Board of Wound Management. Dr. Lullove is Board-Certified by the American Board of Wound Management and a Fellow of the Academy of Physicians in Wound Healing. He also serves as an Editorial Board Member of Today’s Wound Clinic.
Dr. Garoufalis is a Past President of the American Podiatric Medical Association, Past President of the International Federation of Podiatrists and Co-Chair of the Alliance of Wound Care Stakeholders. He is in private practice in Chicago. Dr. Garoufalis discloses that he is a member of the Medical Advisory Board for Modulim.
This content was created in partnership with the American Podiatric Medical Association.

1. Wendland DM, Taylor DWM. Wound measurement tools and techniques: a review. J Acute Care Phys Ther. 2017;8(2):42-57.
2. Shah AJ, Wollak C, Shah JB. Wound measurement techniques: comparing the use of ruler method, 2D imaging and 3D scanner. J Am Coll Clin Wound Spec. 2015;5(3):52-57. doi: 10.1016/j.jccw.2015.02.001.
3. Aung B. A pilot study comparing clinical visual judgement to using MolecuLight i:x imaging device as decision support for patients receiving cellular tissue product for wound healing. Poster presented at SAWC Fall 2019, October 12-14, 2019, Las Vegas, NV.
4. Aung B. Potential cost savings of using Moleculight i:X fluorescence imaging to predict success of cellular tissue products for wound closure. Poster presented at Desert Foot 2019, December 4-7, 2019, Phoenix, AZ.











