ADVERTISEMENT
Study Cites Benefits Of TBI And SPP In Diagnosing PAD
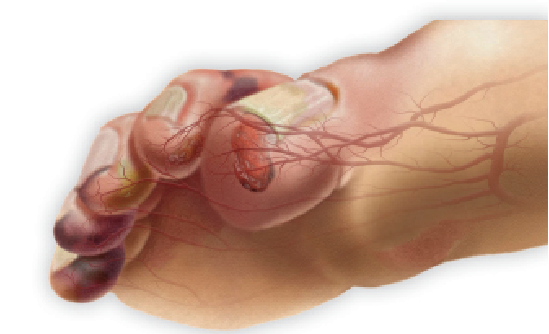 What are the best options for diagnosing peripheral arterial disease (PAD)? A new study in the Journal of Vascular Surgery cites the advantages of the toe brachial index (TBI) and skin perfusion pressure (SPP) testing.
What are the best options for diagnosing peripheral arterial disease (PAD)? A new study in the Journal of Vascular Surgery cites the advantages of the toe brachial index (TBI) and skin perfusion pressure (SPP) testing.
In a study using a Markov model and involving 10,000 patients with diabetes, the authors found that the TBI and SPP testing are sensitive and cost-effective strategies in detecting PAD in patients with diabetic foot ulcers (DFUs). Specifically, they noted that using these tests to corroborate normal pulse examination findings decreased lower extremity amputation rates by 36 percent.
Desmond Bell, DPM, CWS, says screening for PAD can be as simple as asking patients some simple questions, especially when advanced PAD, otherwise known as critical limb ischemia (CLI), is present.
“Understanding that many patients with diabetes, smokers and anyone over the age of 70 are automatically at increased risk for developing PAD should create a concern in the mind of the clinician that PAD may be present,” says Dr. Bell, the founder and President of The Save a Leg, Save a Life Foundation.
Dr. Bell cites the handheld Doppler as the most effective hands-on screening tool for PAD. After obtaining a medical history, he says other invaluable tools include learning to recognize turbulence or distant audible signals in the dorsalis pedis, posterior tibial and peroneal arteries.
As Eric Espensen, DPM, says, measuring toe pressures is key to a true assessment and TBI tests are very useful in patients with diabetes. Along with SPP, TBI tests offer another layer of sensitivity to diagnostic testing, says Dr. Espensen, the Director of Resident Education at the Southern Arizona Limb Salvage Alliance (SALSA)/University of Arizona Hospital.
Dr. Bell says the TBI provides limited useful information when it comes to the preservation of digits that have a higher level of occlusion. He says the TBI may show whether some blood flow is present when one uses the test in conjunction with waveform readings.
Skin perfusion pressure, notes Dr. Bell, measures tissue reactive hyperemia and provides a good overall objective measurement as to where tissue oxygenation is occurring. He says measuring SPP can be extremely useful when assessing pre-vascular intervention (whether it is for a surgical bypass or endovascular intervention, such as atherectomy or stenting) to correlate with any discovered or suspected arterial occlusions, and post-vascular intervention to assess the amount of perfusion to specific areas.
Every patient with diabetes needs screening for PAD, according to Dr. Espensen.
“Simple screening by a skilled physician is a bare minimum to head off problems,” maintains Dr. Espensen. As he notes, many physicians will delay testing until patients demonstrate ulcers but often, early diagnostic screening will prevent PAD and assist patients in attaining a higher quality of health.
Dr. Bell stresses that every patient with diabetes over age 50 should have a PAD screening at least once a year as per the American College of Cardiology/American Heart Association guidelines. In addition, he says any patient with diabetes who receives regular wound care should have a skin inspection and, at a minimum, palpation of pulses, at each doctor’s visit. Dr. Bell emphasizes that if there is concern for PAD or CLI, one should refer the patient to a vascular or endovascular specialist “who has a proven passion for lower extremity preservation.
“You will be providing a potential limb and life-saving service for your patients, and will certainly build a referral base while establishing a limb preservation team in your community,” says Dr. Bell.
FDA Adds Boxed Warnings To Opioids And Benzodiazepines
By Brian McCurdy, Managing Editor
 The U.S. Food and Drug Administration (FDA) is adding boxed warnings to prescription opioid pain medicines, prescription opioid cough medicines and benzodiazepines.
The U.S. Food and Drug Administration (FDA) is adding boxed warnings to prescription opioid pain medicines, prescription opioid cough medicines and benzodiazepines.
The warnings, the administration’s strongest, come after a review revealing that combining opioid medicines with benzodiazepines or other drugs that depress the central nervous system can lead to side effects including slowed or difficult breathing and death, according to the FDA. The FDA advises healthcare professionals to limit prescribing opioid pain medicines with benzodiazepines or other central nervous system depressants only to patients who do not have adequate alternative treatment options. If one prescribes these medicines together, the FDA advises limiting the dosages and durations of each drug to the minimum.
Robert Smith, DPM, MSc, RPh, CPed, notes that millions of Americans suffer from opioid use disorders involving prescription pain medications, and each day more than 40 people fatally overdose on them. While he acknowledges that opioids have a legitimate and important role in treating severe acute pain as well as severe chronic pain conditions and syndromes, Dr. Smith says, “It is clear to me that many times, these products are overprescribed or prescribed without adequate safeguards and monitoring.”
Kristine Hoffman, DPM, concurs. “There was a staggering increase in opioid use in the early 2000s,” she notes. “We have seen a high number of deaths associated with opioid use and concomitant benzodiazepine use increases this risk further.”
In her practice, Dr. Hoffman has already seen a large shift in prescribing practices with a decrease in the amount and duration of opioid pain medications for managing both acute and chronic pain. She cites the problem of “legacy” patients who are already taking large doses of opioids that are often combined with benzodiazepines. The physical dependence as well as mental addiction that can result from this long-term use can be difficult to reduce and/or reverse, according to Dr. Hoffman, who is an Attending Physician in the Department of Orthopedics at Denver Health Medical Center.
As Dr. Smith notes, the new FDA guidelines recommend considering non-opioid therapies, such as non-steroidal anti-inflammatory drugs (NSAIDs) like aspirin and ibuprofen, as well as non-drug treatments like exercise and cognitive behavioral therapy, in lieu of or in conjunction with opioid medications. However, Dr. Hoffman asserts that finding adequate alternatives to opioids can be challenging in the management of acute and chronic pain. She notes NSAIDs, acetaminophen and gabapentin-like medications have numerous associated side effects, may not provide adequate pain relief, and not all patients tolerate them. Alternative treatment modalities for chronic pain, including physical therapy, massage, acupuncture and mental health services, can be costly and insurance does not cover many of those modalities, notes Dr. Hoffman.
Dr. Hoffman cites a new guideline by the Centers for Disease Control and Prevention (CDC) for prescribing opioids for chronic pain as well as a statement from the American Academy of Orthopedic Surgeons on opioids.
To decrease opioid and benzodiazepine abuse, Dr. Hoffman emphasizes adhering to practice guidelines regarding the prescribing of acute and chronic opioid pain medications, and consulting pain management specialists for any patients requiring chronic narcotic treatment or acute narcotic treatment with higher than average dosages or concomitant benzodiazepine use.
There are a number of strategies for educating patients about the risk of opioids, according to Dr. Smith, who is in private practice at Shoe String Podiatry in Ormond Beach, Fla., and is currently deployed in Iraq. He notes physicians should encourage patients to read the medication guides or patient information leaflets that come with their filled prescriptions. To prevent opioid overdoses, Dr. Smith says healthcare professionals should screen patients for risk of substance use disorders and should report adverse events involving pain medications.











