Practical Approaches To Addressing Fall Risk In Your Clinic
I previously wrote an APMA News article on fall risk and fall risk assessment as it relates to the podiatric physician.1 At that time, I discussed the vital importance of looking for those at risk and addressing the etiology of their deficit. The risk factors common among our patient population include muscle weakness (symmetrical), ankle instability, neuropathy, abnormal gait or deficits in gait.
Change is slow. Since the article’s publication, an increasing number of podiatrists have begun using the recommended protocols. Still, many did not see the benefits of combining podiatric biomechanical principles with a plan to mitigate fall risk factors.
However, in a December 2014 study, Yalla and coworkers assessed the use of custom AFOs in 30 ambulatory senior citizens with an average age of 73.2 During eyes-open balance testing, the study authors found that the use of bilateral AFOs resulted in an average reduction of center of mass sway by 49 percent and 40.7 percent respectively in comparison to going barefoot or wearing shoes without AFOs. Other studies are underway.
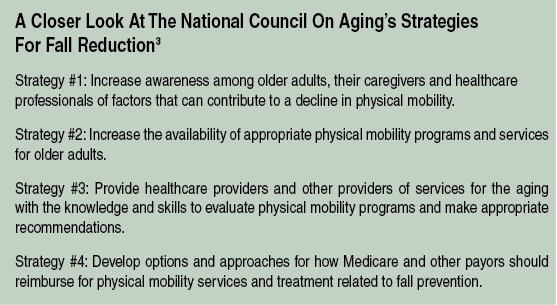
The American Podiatric Medical Association (APMA) now supports the National Council on Aging’s “Falls Free Initiative.”3 Additionally, Medicare’s Physician Quality Reporting System (PQRS) preventative care program includes two measures, 154 and 155, that promote fall risk assessment for all Medicare patients and provide a “plan of care” for all patients who have a history of falls.
 Five Steps To Reducing Falls
Five Steps To Reducing Falls
Our podiatric clinics feature a Fall Prevention and Balance Center that operates in conjunction with our physical therapy department and shoe store. Connecting podiatry, physical therapy and footwear are key to a successful fall risk program.
Accordingly, allow me to propose a protocol that I (and others) have been using in our clinics for years. In our experience, these protocols work, are practical and impact peoples’ lives every day. Here are my five steps to address fall risk successfully in your clinic.
1. Your fall risk protocol should include staff training in how to evaluate patients based on the various factors that can affect balance. In our clinics, we perform fall risk assessments on every patient, not just those with a cane or walker, or those who require assistance due to a gait deficit. Such an approach will satisfy PQRS measure 154.
2. Have a written treatment plan that you can review with your fall risk patients (and their families). It could go something like this:
“Mrs. Jones, you have failed a standardized fall risk assessment that essentially identifies you as being at high risk for falling. I’m concerned about you and I don’t have to tell you how devastating a fall can be. Mrs. Jones, we at the (insert the name of your clinic) have a program for patients just like you and I would like to review our program with you. Don’t wait until you have broken a hip or are in a nursing home from a fall to get serious about fall risk. Our program (Stable Steps or whatever you want to call it) includes physical therapy, home assessment, proper footwear and a mobility enhancing AFO available in a standard flexible and articulated version.”
Patients at risk for falls should also get a recommendation to take a daily supplement of vitamin D. This will satisfy PQRS Measure 155 for “Falls: Plan of Care.”
 3. Have a physical therapy partner who knows how to perform balance physical therapy for your patients at risk for falls. This can be hard for several reasons. First, many in the physical therapy world do not know how to perform proper balance physical therapy. An alternative for patients who cannot go or are reluctant to go to outpatient physical therapy is to order physical therapy through home health.
3. Have a physical therapy partner who knows how to perform balance physical therapy for your patients at risk for falls. This can be hard for several reasons. First, many in the physical therapy world do not know how to perform proper balance physical therapy. An alternative for patients who cannot go or are reluctant to go to outpatient physical therapy is to order physical therapy through home health.
Mobility, strengthening and balance training are key to reducing fall risk and I always recommend these. There are innumerable opportunities to lecture to and find a valuable partner in a home health company. Many in fact have their own fall program but if you use a company, it is vital that you educate staff as to what you do for the patient so there is no confusion.
4. Footwear is key. It is important to ensure a correct fit for shoes. The best shoes are lightweight, easy to don and have a firm heel counter. Having a non-skid sole is important too. Simply wearing properly fitting shoes in the home and not going barefoot or walking in socks can reportedly facilitate an 11-fold reduction in the likelihood of falling in people 65 years of age or older.4
5. Understand the benefits of AFO intervention in reducing fall risk. The APMA recommends “orthotics” for patients who are at risk for falls as orthotics can enhance proprioception on the bottom of the foot. While not part of the APMA recommendation, based on this same principle, a balance AFO offers greater benefit as it contacts a greater surface area. While foot orthotics can improve postural stability via support of the foots longitudinal and transverse arches, an AFO can additionally support weak muscles around the ankle. Postural stability is a key underlying component in falls along with weakness.
In Conclusion
Don’t wait until your patients fall before you start talking to them about their options. Increasing awareness is important but if that is all you are doing, your patients are missing out on a host of tools that may help reduce fall risk.
Dr. Moore is the managing partner of the Cumberland Foot and Ankle Centers of Kentucky. He is a national lecturer and author on a variety of clinical and practice management topics, and has served on the board of the American Association Of Podiatric Practice Management for over 10 years. Dr. Moore has disclosed that he is the inventor of the Moore Balance Brace and is a consultant and lecturer for OHI.
References
1. Moore J. Stepping up to prevent falls. APMA News. June 2011. Available at https://www.bfaas.com/docs/Prevent%20Falls.pdf .
2. Yalla SV, Crews RT, Fleischer AE, et al. An immediate effect of custom-made ankle foot orthoses on postural stability in older adults. Clin Biomech. 2014; 29(10):1081-8.
3. National Council on Aging. Falls Free Initiative: Promoting the National Action Plan to Prevent Falls. Available at https://www.ncoa.org/wp-content/uploads/NCOA18-Month-Falls-Report_FINAL.pdf .
4. Koepsell TD, Wolf ME, Buchner DM, et al. Footwear style and risk of falls in older adults. J Am Geriatr Soc. 2004; 52(9):1495–1501.
Editor’s note: For related articles, see “Preventing Falls In The Elderly: Where DPMs Can Have An Impact in the September 2012 issue of Podiatry Today or the DPM Blog “Emphasizing The Need For Accurate Reporting Of Research On Falls And AFOs” by Doug Richie, DPM at https://tinyurl.com/pxafxnd











