ADVERTISEMENT
Podiatrists Weigh In On Impact Of ACA
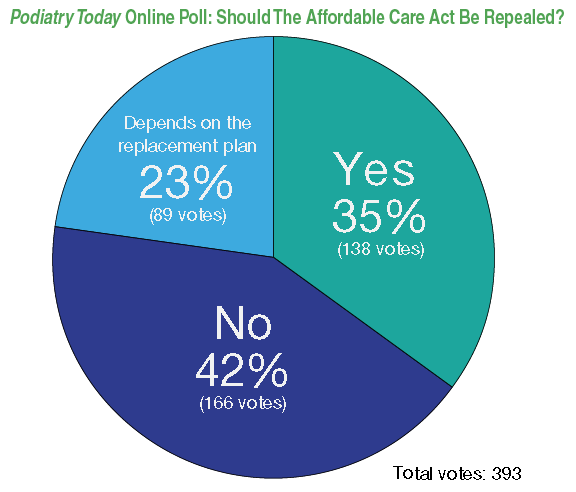 Podiatrists appear to hold a favorable view of the Affordable Care Act (ACA), albeit by a slim margin. In a recent online poll conducted by Podiatry Today, 42 percent of almost 400 respondents answered “no” to the question of whether the ACA should be repealed.
Podiatrists appear to hold a favorable view of the Affordable Care Act (ACA), albeit by a slim margin. In a recent online poll conducted by Podiatry Today, 42 percent of almost 400 respondents answered “no” to the question of whether the ACA should be repealed.
Thirty-five percent said the ACA should be overturned while the remaining 23 percent responded that the decision to repeal the legislation depends on the replacement plan.
The poll reflects a larger trend of growing support among the American public. On April 4, Gallup announced that public support of the ACA gained a majority among Americans for the first time. Fifty-five percent of U.S. adults now approve of the act, up from 42 percent in November 2016. It marked the first time a majority of Americans approved of the law since Gallup first began tracking public opinion of the ACA in this format in 2012.
Enacted by the 111th Congress and signed into law by President Obama in 2010, the Patient Protection and Affordable Care Act — as it’s officially known — implemented a series of mandates, subsidies and insurance exchanges with the stated goals of improving access to care and lowering costs.
“The ACA has resulted in more patients being covered with health insurance through both the state exchange markets and new Medicaid expansion,” comments Lee C. Rogers, DPM, Medical Director of the Amputation Treatment Centers of America in White Plains, NY. “We should commend our profession’s leaders since care by a podiatrist is now covered by Medicaid in almost all states.”
However, while favorability is rising, the debate is far from settled. According to Gallup, while most Americans now approve of the ACA, just 26 percent want to keep it mostly as is. According to Dr. Rogers, “There is a downside to a large portion of the new privately insured patients through the state exchanges.” For these patients, high deductibles and coinsurance often render the insurance almost useless except in catastrophic circumstances, notes Dr. Rogers.
Regardless of one’s personal opinion on the legislation, examining the ACA’s impact on cost and access to care should be an objective, nonpartisan exercise in evaluating its goals and consequences, says Jon A. Hultman, DPM, MBA, CVA, Executive Director of the California Podiatric Medical Association and a consultant for Medical Business Advisors, a medical practice consultancy based in Rockville, MD.
In an ideal scenario, “As problems arise, the entire project isn’t cancelled,” he says. “Instead, the sources of problems are identified and appropriate measures taken to fix them.”
While Dr. Rogers prefers modifying the ACA over outright repeal, he recognizes that rising healthcare expenditures are still on an unsustainable path.
“As doctors, we know it’s not professional fees that are responsible for this growth,” says Dr. Rogers. “In order to stem this spiral, the government needs to regulate the price of health insurance and negotiate the price of pharmaceuticals.”
“If government is going to be involved in healthcare, the only way they will ever come up with an optimum policy would be if state and federal lawmakers were required to have the same health policy as everyone else,” adds Dr. Hultman. “They would more quickly understand the access problems created by narrow networks, high deductibles, and high co-pays.”
Study Questions Validity Of Root Model When Prescribing Orthoses
By Brian McCurdy, Managing Editor
Authors of a recent study believe the foot assessment protocol based on the long-used Root model is “no longer a suitable base” for podiatric physicians. The authors note these study findings have “profound implications” in combination with the wider body of evidence.
The study, published in the Journal of Foot and Ankle Research, screened 140 asymptomatic patients, who had a Root biomechanical assessment to identify five foot deformities. Researchers used a six segment foot model to measure foot kinematics during walking gait in 100 of the 140 patients. Authors noted none of the deformities the Root model proposed were associated with distinct differences in foot kinematics during gait.
The authors recommend that clinicians no longer use the subtalar neutral position during clinical assessments. They also suggest that to define associated foot deformities, physicians should no longer assess the non-weightbearing range of ankle dorsiflexion, first ray position or forefoot alignments and movement.
“It has been long believed by the international podiatric medical community that some of the ideas taught over the years by Root and colleagues need to be more critically evaluated in today’s world of evidence-based medicine,” says Kevin Kirby, DPM, an Adjunct Associate Professor within the Department of Applied Biomechanics at the California School of Podiatric Medicine at Samuel Merritt University in Oakland, Calif.
Dr. Kirby notes that he and others have for three decades publically questioned the biomechanics theories of Merton Root, DPM, and colleagues. He notes that 20 years ago Menz and colleagues discussed inaccuracies with Root’s measurement system and how podiatrists could improve on Root’s static morphologic measurement system.
However, Dr. Kirby also notes “significant issues” with the study and suggests that some of its conclusions are “overstated.” He notes the study participants were asymptomatic as opposed to being patients with pathologies so it is unknown whether the Root measurements correlated to any mechanically-based pathologies of the lower extremity.
Dr. Kirby says the research was a kinematics (position and motion) study rather than a kinetics (forces and moments) study so researchers did not use pressure insoles or pressure mats to study temporal and segmental plantar pressure patterns during walking. Even though there was no significant correlation of foot motions to the Root static measurements, he says the researchers did not measure the external forces and pressures acting on the foot, or measure the muscle activity or internal forces, stresses or moments acting within the structural components of the foot and lower extremity during gait.
“Since abnormal magnitudes of external and internal forces, moments, pressures and stresses are the cause of the mechanically-based pathologies seen in the podiatrist’s offices on a daily basis, and not abnormal foot motion, measuring the kinetics of the foot and lower extremity is absolutely essential to understand if foot and lower extremity ‘deformities’ may or may not cause musculoskeletal injury,” asserts Dr. Kirby. “Thus, using kinematics-only research to suggest elimination of a clinical evaluation system for treating musculoskeletal injuries that are directly caused by abnormal forces and moments, seems unwise at best.”
For a related DPM Blog, see https://www.podiatrytoday.com/blogged/defending-root-new-study-jarvis-and-colleagues-all-it-cracked-be .
Can Lower Extremity X-Rays Help Predict Osteoporosis Risk?
By Brian McCurdy, Managing Editor
A recent poster study presented at the American College of Foot and Ankle Surgeons Annual Scientific Conference notes that X-rays can help clinicians determine the risk of osteoporosis.
The poster, which won second place in the scientific category, focused on 40 women with osteoporosis and 40 control patients with a mean age of 64.4 for the study population. Patients had dual-energy X-ray absorptiometry (DEXA) scans and two X-rays each. The study authors found that patients are at an increased risk of osteoporosis when AP X-rays detect less than 50 percent of the second metatarsal consists of cortical bone or the presence of intracortical tunneling in at least one lesser metatarsal.
Lead study author Adam Fleischer, DPM, MPH, supports physicians placing more emphasis on detecting osteoporosis in the lower extremity.
“Day in and day out, we see numerous patients who fall into the ‘older adult’ and ‘elderly’ age categories who are at risk for having diminished skeletal bone mass,” says Dr. Fleischer, who is affiliated with the Department of Surgery at Advocate Illinois Masonic Medical Center in Chicago. “We also see patients who develop non-traumatic fractures in the foot, sometimes multiple times, and we need to do a better job of ensuring that their bone health is being investigated and properly worked up.”
As with most disease processes, Dr. Fleischer points out that the earlier one detects osteoporosis, the better the opportunity for corrective action. He notes that is when pharmacologic interventions and vitamin supplementation will have their greatest impact on bone metabolism and bone health. To that end, he says establishing the diagnosis of osteoporosis in a 50-year-old woman who presents after her second go-round with a central metatarsal stress fracture would likely have more impact than establishing the diagnosis in a 75-year-old patient who presented to the practice with heel spurs.
In letting osteoporosis go undiagnosed, Dr. Fleischer cites a “missed opportunity”to make an important difference in the lives of patients. He and his colleagues are attempting to develop some simple rules that podiatrists can apply to X-rays that, in combination with clinical indicators, prompt the physician to look further into the patient’s bone health.











