Locking Plates: What Have We Learned?
Although traditional plate designs date back decades, these authors discuss the emergence and potential of locking compression plates, polyaxial locking plates, and minimally invasive plate osteosynthesis.
 The popularization of traditional plate and screw constructs dates back to the late 19th century as well as the efforts of the Belgian surgeon Robert Danis, MD.1,2 Danis designed a compression plate termed the coapteur, which rigidly stabilized diaphyseal fractures and produced fracture healing in the absence of callus formation.
The popularization of traditional plate and screw constructs dates back to the late 19th century as well as the efforts of the Belgian surgeon Robert Danis, MD.1,2 Danis designed a compression plate termed the coapteur, which rigidly stabilized diaphyseal fractures and produced fracture healing in the absence of callus formation.
This discovery along with Danis’ publication of The Theory and Practice of Osteosynthesis inspired Mueller and other Swiss surgeons to eventually form the Arbeitsgemeinschaft für Osteosynthesefragen (AO) Foundation in March 1959.1,2 Their work imparted the four basic concepts of fracture management that included: anatomic reduction, stable fixation, atraumatic surgical technique and pain-free immobilization after surgery.3
Over the past several decades, as surgeons have gained a better understanding of the utility of plate and screw constructs, the application of the devices has evolved. In addition to incorporating these devices into the surgical repair of fractures, surgeons may utilize them for joint arthrodesis and other reconstructive osseous surgeries. One advance with these modalities has been the advent and evolution of the locking plate construct, which has several applications within foot and ankle surgery.
Reviewing The Different Kinds Of Plate Fixation
Traditional fixation plates vary in size, shape, thickness and material. However, their primary function remains the same: to provide stability to bone by resisting physiological loads and thereby maintaining anatomic alignment and osseous contact to allow primary bone healing. In general, we can categorize bone plates based on their principal function.
 Neutralization plates function as load-sharing apparatuses that shield lag screws from the torsional forces the surgeon encounters during range of motion.4
Neutralization plates function as load-sharing apparatuses that shield lag screws from the torsional forces the surgeon encounters during range of motion.4
Buttress plates and anti-glide plates are load-bearing devices that can support a section or segment of bone, which are frequently areas of impaction associated with significant comminution of the cortex, thus leaving a compromised diaphyseal construct and/or voids within the cancellous bone. By fixing the plate proximally and distally to stable areas of bone, the surgeon can prevent the segments from re-approximating during axial loading.5
There are two kinds of compression plates: static compression plates and dynamic compression plates. With the static compression plate, the compression yielded at the fracture interface is secondary to the tension one applies to the implant. This technique is beneficial for those transverse or short oblique fractures when insertion of a lag screw is not attainable. In order to achieve compression, drill the initial screws eccentrically through oval holes in the plate away from the fracture site. As the screw heads contact the plate and sit centrally in the oval holes, the fragments compress together.
The dynamic compression plate adheres to the tension band principle. This refers to the application of a plate on the tension (convex) side, preventing gapping that normally would occur and converting the distracting forces into compression forces.
The placement of a plate to bone serves as both an expediter and a temporary inhibitor of osseous repair.5 The compression yielded by the plate as well as axial force shielding come at a cost typically forfeited during the installation process when the bone’s vascularity can be compromised. While the emergence of newer percutaneous, minimally invasive techniques and radiolucent guides can limit the amount of soft tissue dissection, some degree of vascular disruption is inevitable.
 Certain plate designs have addressed the effects of reduced blood flow that can occur underneath a plate due to reduced bone density. This plate-associated osteoporosis has a detrimental effect on the mechanical properties of healing bone. Limited contact dynamic compression plates were designed with recesses or undercuts in the plate to reduce contact between the plate and the bone, therefore reducing the risk of plate-associated osteoporosis.
Certain plate designs have addressed the effects of reduced blood flow that can occur underneath a plate due to reduced bone density. This plate-associated osteoporosis has a detrimental effect on the mechanical properties of healing bone. Limited contact dynamic compression plates were designed with recesses or undercuts in the plate to reduce contact between the plate and the bone, therefore reducing the risk of plate-associated osteoporosis.
Recognizing The Potential Benefits Of Locking Compression Plates
Conventional plates loaded axially in tension and/or compression rely on the applied force to convert to shear stress at the plate-bone interface.6 Therefore, axial forces are countered by the shear force between the plate and the bone that relies on the screw purchase into the underlying bone. However, when there is osteoporotic, comminuted or pathologic bone, problems arise with screw purchase. In these instances, it becomes impossible to generate sufficient torque to withstand plate and fracture motion.
There have been efforts to improve the weakest part of the construct (the screw-bone interface) by increasing the contact area between the screw and the bone with the placement of screws in polymethyl methacrylate (PMMA) or by creating a single-beam construct. This is the principle behind locking plates with the creation of a construct to address the lack of motion between the components of the beam (i.e., the plate, screw and bone).6 Functionally, a locking plate works as a fixed-angle construct when one inserts the locking screws.
 The locking compression plate arose from the desire to increase stability, which at the time was limited by the torque generated during screw purchase into the plate-bone interface. Cancellous, osteoporotic or pathologic bone and comminution limit the amount of torque that one can generate to enhance stability.7 In order to increase the friction coefficient between the plate and the bone, excessive soft tissue stripping was necessary, thereby increasing the chance of avascular necrosis to the bony fragments and soft tissue flaps.
The locking compression plate arose from the desire to increase stability, which at the time was limited by the torque generated during screw purchase into the plate-bone interface. Cancellous, osteoporotic or pathologic bone and comminution limit the amount of torque that one can generate to enhance stability.7 In order to increase the friction coefficient between the plate and the bone, excessive soft tissue stripping was necessary, thereby increasing the chance of avascular necrosis to the bony fragments and soft tissue flaps.
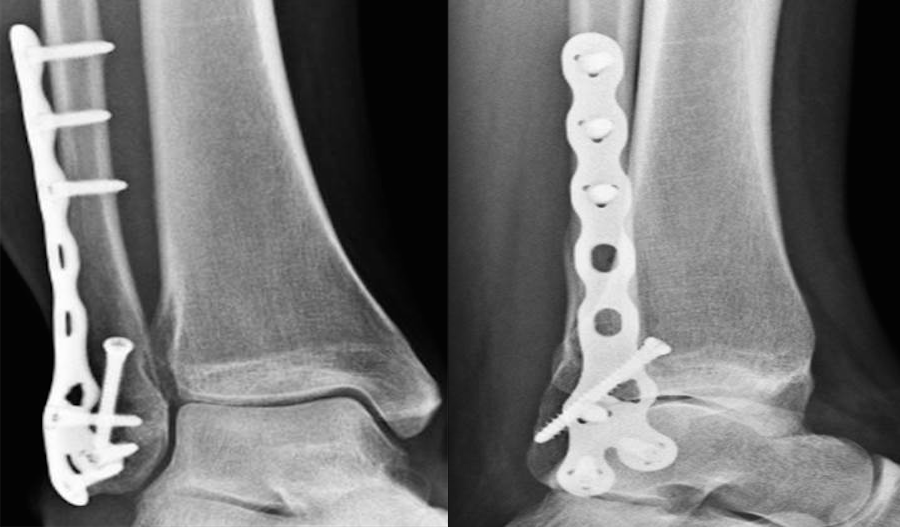
This led to the development of the locking compression plate, which has the ability to preserve the blood supply to bone by reducing periosteal stripping. The traditional plating techniques provided stability by compressing the plate to the bone surface with the screws achieving bicortical purchase as the second point of fixation. However, locking compression plate technology features unicortical locking screws that can be an “internal fixator” that can act as a bridge over compromised bone.8
However, in areas or regions where high torsional and axial loads are expected, one should utilize bicortical locking screws. With locking plates, the sum of all the interfaces between the screws and bone equals the strength of fixation as opposed to the unlocked plates’ single screw pullout strength.7 Alternately, conventional screws fail by toggling within the bone with each screw essentially functioning alone.
One of the benefits of locking plates is their ability to be “bridge plates,” whereby they provide excellent axial and angular stability, preserve fragmentary blood supply, and reduce the risk of loss of reduction. Indeed, surgeons do not have to contour these plates anatomically to the bone, and the plates have the potential benefit of providing superior fixation in osteoporotic bone. Indications for the use of locking plates include diaphyseal/metaphyseal fractures in osteoporotic bone, multifragmentary diaphyseal/metaphyseal fractures, osteotomies in at-risk patients (poor bone stock, revisions, etc.), articular fractures, segmental fractures with multiple patterns, and any combination of the above.9
 In their guidelines for using the locking compression plate, Gautier and Sommer emphasize the importance of the reduction technique, minimally invasive plate insertion and fixation to keep bone viability undisturbed.9 They also note that achieving sound fixation depends on selecting the proper length and type of implant, and employing the appropriate number of screws. Doing so can prevent potential complications with pullout of screws and secondary displacement, according to these authors.
In their guidelines for using the locking compression plate, Gautier and Sommer emphasize the importance of the reduction technique, minimally invasive plate insertion and fixation to keep bone viability undisturbed.9 They also note that achieving sound fixation depends on selecting the proper length and type of implant, and employing the appropriate number of screws. Doing so can prevent potential complications with pullout of screws and secondary displacement, according to these authors.
Pertinent Insights On Minimally Invasive Plate Osteosynthesis
Another recent evolution is that of minimally invasive plate osteosynthesis. This technique is an endeavor to reduce the risk of soft tissue and vascular intrusion that occurs during traditional open reduction internal fixation of long bone fractures.
 Minimally invasive plate osteosynthesis maintains bone vascularization with minimal periosteal stripping, thus improving bony consolidation and decreasing operative time, complications and infection rates. The application of a locking plate using the minimally invasive plate osteosynthesis technique generally consists of making small incisions proximal and/or distal to the fracture site, percutaneous reduction and subsequent extraperiosteal placement of the plate with any radiolucent percutaneous guide.
Minimally invasive plate osteosynthesis maintains bone vascularization with minimal periosteal stripping, thus improving bony consolidation and decreasing operative time, complications and infection rates. The application of a locking plate using the minimally invasive plate osteosynthesis technique generally consists of making small incisions proximal and/or distal to the fracture site, percutaneous reduction and subsequent extraperiosteal placement of the plate with any radiolucent percutaneous guide.
Can Polyaxial Locking Plates Have An Impact?
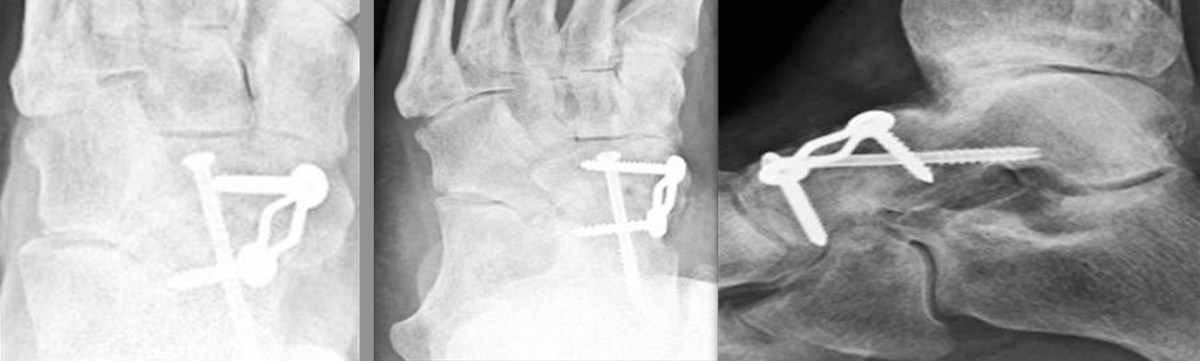
Another advancement in the development of locking plate technology is the addition of polyaxial or variable axial screw holes in the plate. This becomes extremely valuable when a surgeon is addressing a periarticular fracture, especially one that involves significant comminution or damage to the soft tissue envelope. These plates were designed to improve angular stability by allowing variable screw trajectory to the plate, thereby increasing the probability that the screw will be able to purchase good bone while avoiding articulating surfaces.
A recent study by Cullen and colleagues looked at a biomechanical comparison of polyaxial and uniaxial locking plate fixation in extra-articular proximal tibia metaphyseal fractures.10 The authors concluded that the polyaxial plates were as sturdy as the uniaxial locking plates and could achieve more stability with an angled screw through the fracture site.
A Closer Look At Potential Contraindications And Complications
 Currently, there are no absolute contraindications for locking plates. However, there are instances when applying them may be unnecessary. A good example would be in a case with a simple fracture pattern in a healthy patient with good quality bone.
Currently, there are no absolute contraindications for locking plates. However, there are instances when applying them may be unnecessary. A good example would be in a case with a simple fracture pattern in a healthy patient with good quality bone.
Another case would be a fracture pattern where the surgeon is trying to achieve compression through the plate itself without the addition of a lag screw. Also, if a patient has an oligotrophic non-union and the cause of the delayed healing is not related to an insufficient amount of stability, one should not employ locking plates.
Another matter to keep in mind is the increased cost of a locking plate-screw construct versus traditional plate-screw designs, which in some cases can be substantial. As always, consider the possibility of a metal allergy or intolerance.
 One of the more common complications with locking plates is creating an environment of too much stability, thus becoming “non-union generators.”11 Numerous biomechanical investigations have established this issue with the study of fracture gap and screw stress with locked plates.10 Gautier advocated pre-dynamizing the plates by allowing at least two empty screws over the fracture site, thus decreasing the internal stress of the plate while increasing the overall work length.9
One of the more common complications with locking plates is creating an environment of too much stability, thus becoming “non-union generators.”11 Numerous biomechanical investigations have established this issue with the study of fracture gap and screw stress with locked plates.10 Gautier advocated pre-dynamizing the plates by allowing at least two empty screws over the fracture site, thus decreasing the internal stress of the plate while increasing the overall work length.9
Final Thoughts
Manufacturing companies are developing new plate designs with the goals of improving the ease of application and minimizing bulk while maintaining strength. Combination plates with holes capable of receiving polyaxial locked or non-locked screws are becoming the norm. This allows the surgeon to insert either type of screw with respect to the underlying anatomy and not be constrained to the plate design or screw trajectory.
As we previously discussed, it is important to tailor the fixation of choice to the fracture pattern and location, the underlying bone quality and the overall needs of the patient. We still need to see more clinical data on locking plate technology in order to determine specific clinical scenarios in which the additional cost may be justified.
Dr. Fidler is a Fellow at the Orthopedic Foot and Ankle Center in Westerville, Ohio.
Dr. Prissel is a Fellow at the Orthopedic Foot and Ankle Center in Westerville, Ohio.
Dr. Hyer is the Fellowship Director of the Advanced Foot & Ankle Surgical Fellowship in Westerville, Ohio. He is a Fellow and a member of the Board of Directors for the American College of Foot and Ankle Surgeons.
References
- Bagby GW. Compression bone-plating: historical considerations. J Bone Joint Surg Am. 1977; 59(5):625-31.
- Danis R. Theorie Et Practique De L’ Osteosynthese. Masson, Paris, 1949.
- Colton CL. AO fixation. Injury. 1990; 21(5):287-290.
- Burstein AHWT. Fundamentals of Orthopaedic Biomechanics. Williams and Wilkins, Baltimore, 1994.
- Banks AS, Downey MS, et al. McGlamry’s Comprehensive Textbook of Foot and Ankle Surgery. Lippincott Williams & Wilkins, Philadelphia, 2001.
- Egol KA, Kubiak EN, Fulkerson E, et al. Biomechanics of locked plates and screws. J Orthop Trauma. 2004; 18(8):488-93.
- Cordey J, Borgeaud M, Perren SM. Force transfer between the plate and bone: relative importance of the bending stiffness of the screws friction between plate and bone. Injury. 2000; 31(Suppl 3):C21-8.
- DiDomenico LA, Garchar D. Fixation techniques in foot and ankle surgery. In: Levy L (ed): Principles and Practice of Podiatric Medicine, Chapter 52, Data Trace Publishing, Brooklandville, MD. 2007.
- Gautier E, Sommer C. Guidelines for the clinical application of the LCP. Injury. 2003; 34(Suppl 2):B63-76.
- Cullen AB, Curtiss S, Lee MA. Biomechanical comparison of polyaxial and uniaxial locking plate fixation in a proximal tibial gap model. J Orthop Trauma. 2009; 23(7):507-513.
- Stoffel K, Dieter U, Stachwiak G, et al. Biomechanical testing of the LCP- how can stability in locked internal fixators be controlled? Injury. 2003; 34(Suppl 2):B11-9.











