Key Pearls On Medial Column Procedures For Adult-Acquired Flatfoot
Discussing the pathomechanics of posterior tibial tendon dysfunction, what to look for in the clinical exam and pertinent surgical considerations, this author shares insights from his experience as well as the literature on surgical repair of adult-acquired flatfoot deformities.
 The surgical management of adult-acquired flatfoot deformities due to posterior tibial tendon dysfunction (PTTD) involves many soft tissue and bone procedures. It is common to perform a midfoot fusion in addition to other procedures. The complex architecture of the midfoot provides stability in the normal foot to allow the foot to become a rigid lever at the end of midstance to propel the body forward. Prachgosin and colleagues have demonstrated that in patients with flexible flatfoot, there is a greater eversion deforming force to the medial longitudinal arch in comparison to normal controls.1 This increased eversion unlocks the midtarsal joint and contributes to the forces that lead to tissue fatigue.
The surgical management of adult-acquired flatfoot deformities due to posterior tibial tendon dysfunction (PTTD) involves many soft tissue and bone procedures. It is common to perform a midfoot fusion in addition to other procedures. The complex architecture of the midfoot provides stability in the normal foot to allow the foot to become a rigid lever at the end of midstance to propel the body forward. Prachgosin and colleagues have demonstrated that in patients with flexible flatfoot, there is a greater eversion deforming force to the medial longitudinal arch in comparison to normal controls.1 This increased eversion unlocks the midtarsal joint and contributes to the forces that lead to tissue fatigue.
When repeated insults occur to the structural support due to hypermobility of the medial column and a short triceps surae complex, the tendinous and ligamentous structures may eventually become strained, leading to failure. This is the normal clinical course of the PTTD cascade. As the structural supports weaken, the medial column progressively breaks down as described with many staging systems.2,3 The tendinopathy of the posterior tibial tendon pairs the degenerative tendon pain and the impaired performance of the medial column structure. The goal of reconstruction should be to provide a stable and functional foot without significant overload to the supporting structures.
A subset of patients with a short triceps surae complex who do not have medial column hypermobility do not obtain structural collapse of the medial column. They create increased strain in the midfoot through the naviculocuneiform and tarsometatarsal joints. This sagittal plane loading phenomenon leads to progressive degenerative arthrosis of the tarsometatarsal and naviculocuneiform joints. Most foot and ankle surgeons clearly recognize this pattern of progressive arthrosis just as commonly as the PTTD course.4
 Foot and ankle surgeons commonly hear patients complain about their inability to lose weight due to their painful foot or ankle condition. This is a common presentation for patients with PTTD and will be a more frequent discussion in the future. There is clearly an increase in the incidence of adult obesity in the United States. A recent report of age-matched adults reveals the incidence of obesity (with a BMI > 30) rising from 14.4 percent in 1980 to 30.5 percent in a sampled population of over 4,000 individuals.5 In regard to severe obesity (BMI > 40), there previously was no information about this group in 1980 but most recently has been reported to be 4.7 percent in 2000.5
Foot and ankle surgeons commonly hear patients complain about their inability to lose weight due to their painful foot or ankle condition. This is a common presentation for patients with PTTD and will be a more frequent discussion in the future. There is clearly an increase in the incidence of adult obesity in the United States. A recent report of age-matched adults reveals the incidence of obesity (with a BMI > 30) rising from 14.4 percent in 1980 to 30.5 percent in a sampled population of over 4,000 individuals.5 In regard to severe obesity (BMI > 40), there previously was no information about this group in 1980 but most recently has been reported to be 4.7 percent in 2000.5
Essential Diagnostic Insights From The Clinical Evaluation
Patients with stage 2 PTTD present with a variety of deformities depending on planal dominance of the deformity. In patients with an unstable naviculocuneiform joint, one may note a sagittal plane collapse with a medial column sag demonstrating a naviculocuneiform fault radiographically. In transverse planal dominant deformities, one will see the too many toes sign with abduction of the midfoot and forefoot. The frontal plane deformities have a moderate heel valgus presentation with a forefoot supinatus or varus condition. The inability to perform a single limb rise test without inversion of the heel is common for advanced deformities where the function of the posterior tibial tendon has been lost due to an attenuated or ruptured posterior tibial tendon.
 The performance of Jack’s test will help reveal the reducibility of the flatfoot deformity.6 A test I commonly perform on my patients involves external rotation of the leg with maintenance of lateral column weightbearing while I find the midtarsal joint neutral position. I have the patient hold his or her foot in this position, and evaluate the forefoot position. If I can manually reduce the deformity to weightbearing on the first ray, I consider this forefoot supinatus, which will reduce once I have addressed the proximal deformity by improving the lever of the peroneus longus tendon. If I cannot manually reduce the forefoot deformity, it is a forefoot varus that requires surgical correction with a Lapidus procedure, Cotton osteotomy, or wedging the naviculocuneiform arthrodesis. It is important to assess the difference between forefoot supinatus and forefoot varus.
The performance of Jack’s test will help reveal the reducibility of the flatfoot deformity.6 A test I commonly perform on my patients involves external rotation of the leg with maintenance of lateral column weightbearing while I find the midtarsal joint neutral position. I have the patient hold his or her foot in this position, and evaluate the forefoot position. If I can manually reduce the deformity to weightbearing on the first ray, I consider this forefoot supinatus, which will reduce once I have addressed the proximal deformity by improving the lever of the peroneus longus tendon. If I cannot manually reduce the forefoot deformity, it is a forefoot varus that requires surgical correction with a Lapidus procedure, Cotton osteotomy, or wedging the naviculocuneiform arthrodesis. It is important to assess the difference between forefoot supinatus and forefoot varus.
The evaluation of ankle joint dorsiflexion will commonly reveal a tight posterior muscle group. There is no consensus on the exact definition of equinus but clearly the inability to dorsiflex to more than 10 degrees with the knee extended and the foot held in neutral alignment would indicate a short gastrocnemius muscle unit. When there is normal ankle dorsiflexion with the knee flexed, there is no need to weaken the soleus muscle.
During the clinical examination, one must take care to ensure the patient has no additional neuromuscular deficits or proximal deformities that may affect his or her ankle and foot alignment, or contribute to the patient’s post-surgical recovery. In patients with advancing age and concomitant progressive lower extremity deformities, their proximal joints are wearing down at the same or at a possibly accelerated rate due to their foot deformities. Patients may have had prior trauma to the foot, ankle or leg, and may have severe knee arthrosis with a frontal plane malalignment. They also may present with a limb length inequality from a prior knee or hip arthroplasty, which requires compensation at the foot and ankle. All of these require proper evaluation before definitive reconstruction.
 Imaging of the foot and ankle includes standard weightbearing views as well as long leg axial images to properly assess the foot to leg position. One may obtain advanced imaging with computed tomography (CT) or magnetic resonance imaging (MRI) if there is concern for additional deformities or to assess joint arthrosis. In certain cases, it may be helpful to obtain single-photon emission computed tomography (SPECT-CT) imaging to further pinpoint areas of increased bone activity.
Imaging of the foot and ankle includes standard weightbearing views as well as long leg axial images to properly assess the foot to leg position. One may obtain advanced imaging with computed tomography (CT) or magnetic resonance imaging (MRI) if there is concern for additional deformities or to assess joint arthrosis. In certain cases, it may be helpful to obtain single-photon emission computed tomography (SPECT-CT) imaging to further pinpoint areas of increased bone activity.
Step-By-Step Surgical Pearls
Almost all patients require lengthening of the posterior muscle group unless this has happened previously. Routinely, I perform a Baumann procedure to limit violation of the gastrocnemius muscle and avoid unnecessary lengthening of the soleus muscle.7 I find the patients recover much quicker and regain their strength in a much shorter period of time in comparison to the traditional tongue and groove tendo-Achilles lengthening or Strayer procedure. Once the surgeon has addressed the equinus, he or she would perform additional lateral column procedures such as the medial displacement calcaneal osteotomy and/or the Evans calcaneal osteotomy. These two procedures have a powerful effect on the alignment of the foot and one needs to perform these procedures prior to a naviculocuneiform fusion to prevent the possibility of overcorrecting the medial column. The Evans lengthening is a triplanar correction that not only results in relative shortening of the medial column but also plantarflexes the medial column via tensioning of the plantar structures.
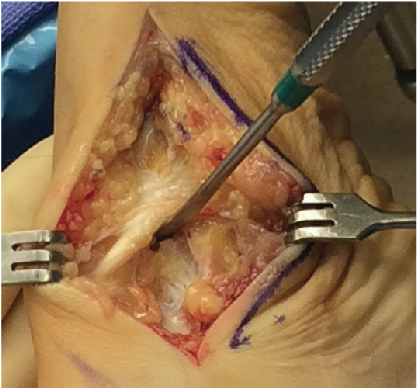
 For the approach to the medial column, one makes a medial midfoot incision originating anterior to the medial malleolus and extending to the first tarsometatarsal joint. Keep the incision below the medial venous structures to allow them to be easily retracted. Once there is adequate exposure, identify and retract the saphenous nerve with the venous vessels. In some patients, the medial origin of the naviculocuneiform joint may appear unclear and an easy guide is the insertion of the tibialis anterior tendon onto the medial cuneiform. The tibialis anterior tendon forms a firm veil to the medial naviculocuneiform joint and mobilization immediately proximal to the insertion with elevation of the tendon exposes the joint.
For the approach to the medial column, one makes a medial midfoot incision originating anterior to the medial malleolus and extending to the first tarsometatarsal joint. Keep the incision below the medial venous structures to allow them to be easily retracted. Once there is adequate exposure, identify and retract the saphenous nerve with the venous vessels. In some patients, the medial origin of the naviculocuneiform joint may appear unclear and an easy guide is the insertion of the tibialis anterior tendon onto the medial cuneiform. The tibialis anterior tendon forms a firm veil to the medial naviculocuneiform joint and mobilization immediately proximal to the insertion with elevation of the tendon exposes the joint.
Sharp release of the ligamentous structures dorsally and plantarly allows for enough exposure to see the first 5 mm of the medial cuneiform to allow for appropriate preparation of the resection of the joint. I am careful to avoid over-aggressive resection of the joint surfaces. Starting the resection too proximal on the navicular and/or too distal on the cuneiform may result in overcorrection of the foot. Performing a minimal initial resection allows for more aggressive resection or planing later if necessary. I attempt to remove 2 to 3 mm of cartilage, which includes both the articular cartilage and the calcified cartilage layer. One performs this resection on both sides of the joint, including the first and second cuneiform, and, if necessary, the third cuneiform. I do not believe an isolated first cuneiform-navicular fusion is adequate to provide a solid construct for fusion of the entire three-joint complex.8 When one performs an isolated medial cuneiform navicular fusion, there is less than 50 percent of the joint surface fused and the majority of the joint maintains motion, directly working against the goal of a solid fusion site.
Once you have exposed the cancellous bone of the fusion site, place a self-retaining bone retractor into the surgical site and prepare the joints for fusion with subchondral drilling and fish scaling. One can accomplish fusion reduction with a bone reduction forceps. Prior to placing hardware, evaluate the alignment of the foot. Ideally, the first ray should be parallel to the lesser rays and the heel bisection should exit through the second ray. Evaluate the fusion site for gapping and close apposition. If the dorsal margins of the fusion site have been inadequately resected, the presence of a bony bridge can prevent clear apposition, which requires feathering with a sagittal saw or bony resection.
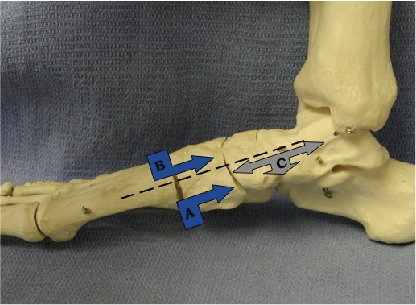 One can achieve fixation of the fusion with screws, plates (locking and non-locking) or staples. I commonly perform internal fixation with cannulated screws. Once I am confident in the alignment and temporary position of the fusion, I will place my guide wires. I will place three screws and the anatomy dictates whether it is two screws proximal and one screw distal or one screw proximal and two screws distal. The surgeons should place all these screws below the midline vertical bisection of the joint. The first screw I place is from the medial cuneiform to the lateral pole of the navicular. I am aiming from the distal-plantar medial cuneiform to the anterior process of the calcaneus. Place the second screw from the navicular to the lateral cuneiform and aim the guide wire from the inferior navicular tuberosity to the central fifth metatarsal. The last screw is distal or proximal depending on the available anatomy. I commonly place my third screw from the navicular to the intermediate cuneiform.
One can achieve fixation of the fusion with screws, plates (locking and non-locking) or staples. I commonly perform internal fixation with cannulated screws. Once I am confident in the alignment and temporary position of the fusion, I will place my guide wires. I will place three screws and the anatomy dictates whether it is two screws proximal and one screw distal or one screw proximal and two screws distal. The surgeons should place all these screws below the midline vertical bisection of the joint. The first screw I place is from the medial cuneiform to the lateral pole of the navicular. I am aiming from the distal-plantar medial cuneiform to the anterior process of the calcaneus. Place the second screw from the navicular to the lateral cuneiform and aim the guide wire from the inferior navicular tuberosity to the central fifth metatarsal. The last screw is distal or proximal depending on the available anatomy. I commonly place my third screw from the navicular to the intermediate cuneiform.
A Guide To Postoperative Care
Patients use a posterior splint postoperatively and I see them three to five days later for a dressing change and cast placement. At three weeks postoperatively, I remove the sutures and obtain radiographs. Then I perform a second cast application for six weeks. Once radiographic evidence of significant consolidation is present, I encourage the patient to begin progressive weightbearing in a fracture boot. The patients commonly begin physical therapy and progress to a gauntlet brace or custom orthotics to provide additional support to the foot during the first six months of the post-surgical recovery phase.
The surgical management of adult-acquired flatfoot deformities due to PTTD involves many different procedures. The naviculocuneiform fusion helps reestablish needed stability to the medial column in patients who show clinical and radiographic evidence of medial column instability. One may perform the procedure as a stand-alone procedure in isolated cases but it commonly requires adjunctive lateral column procedures to realign the malaligned foot appropriately. Radiographic analysis of the medial column stabilization procedures with or without a calcaneal osteotomy has shown marked improvement.9 With appropriate patient selection, proper surgical technique and a stable fixation construct, this technique should provide the patient and the surgeon with a successful outcome.
Dr. DiNucci is a Fellow of the American College of Foot and Ankle Surgeons. He is in private practice in Scottsdale, AZ. He is a past board member of the American College of Foot and Ankle Surgeons.
References
- Prachgosin T, Chong DY, Leelasamran W, Smithmaitrie P, Chatpun S. Medial longitudinal arch biomechanics evaluation during gait in subjects with flexible flatfoot. Acta Bioeng Biomech. 2015;17(4):121-30
- Johnson KA, Strom DE. Tibialis posterior tendon dysfunction. Clin Orthop. 1989;239:196-206.
- Myerson MS. Adult acquired flatfoot deformity. J Bone Joint Surg. 1996;78A:780-792.
- Rush SM, Jordan T. Naviculocuneiform arthrodesis for treatment of medial column instability associated with lateral peritalar subluxation. Clin Podiatr Med Surg. 2009;26(3):373-84.
- Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999-2000. JAMA. 2002;228(14):1723-7.
- Sheikh Taha AM, Feldman DS. Painful flexible flatfoot. Foot Ankle Clin. 2015;20(4):693-704.
- Baumann JU, Koch HG. Ventrale aponeurotische Verlangerung des Musculus gastrocnemius. Operative Orthop Traumatol. 1989;1:254-258.
- Lui TH. Arthroscopic revision arthrodesis for non-union of the naviculocuneifom joint: a case report. J Orthop Surg (Hong Kong). 2015;23(2):267-9.
- Jordan TH, Rush SM, Hamilton GA, Ford LA. Radiographic outcomes of adult acquired flatfoot corrected by medial column arthrodesis with or without a medializing calcaneal osteotomy. J Foot Ankle Surg. 2011;50(2):176-81.












