How Does Culture Compare With PCR In Identifying Wound Infection?
 A recent retrospective study, presented as a scientific poster, compares the ability of conventional cultures and polymerase chain reactions (PCR) to identify infections in lower extremity wounds.
A recent retrospective study, presented as a scientific poster, compares the ability of conventional cultures and polymerase chain reactions (PCR) to identify infections in lower extremity wounds.
The poster, which won first place at the American College of Foot and Ankle Surgeons (ACFAS) Scientific Conference, focused on 124 deep tissue specimens from 34 inpatients. The poster authors note that culture identified Enterococcus more frequently than PCR while there was no difference in identification by either method of coagulase-negative Staphylococcus aureus, S. aureus, S. agalactiae and Pseudomonas aeruginosa. The authors conclude that PCR may quickly detect bacterial species during the first debridement in the OR while cultures may help evaluate wound biodiversity with serial debridement.
“Both (PCR and culture) are able to depict quantitative reduction of bacterial load, but only culture was able to show reduction of bacterial species, notes poster coauthor Kevin Ragothaman, DPM. “This is important as species identification is what drives clinical decision making with regard to antibiotic selection.”
Dr. Ragothaman cites advantages of PCR such as its faster approach and increased sensitivity in identifying bacteria in chronic wounds in comparison to culture. Additionally, he says PCR is theoretically able to identify bacteria despite treatment with antibiotic therapy. One could see the sensitivity of PCR as a disadvantage as not all identified bacteria may be clinically pathologic, according to Dr. Ragothaman, a second-year resident within the Division of Podiatric Surgery at MedStar Washington Hospital Center in Washington, DC.
Poster coauthor Tammer Elmarsafi, DPM, AACFAS, says an advantage to PCR is that its quantification is numerical rather than semi-quantitative. He notes that PCR had more “noise” in the study in the sense that each specimen contained a plethora of bacteria, which complicates clinical management algorithms. As the wound gets “cleaner,” PCR becomes less apt at picking up smaller changes, which may be because of the constant background noise of irrelevant, dead bacterial DNA, according to Dr. Elmarsafi, an Attending Physician in the Division of Podiatric Surgery at MedStar Washington Hospital Center.
Culture is advantageous as it is widely accessible and commonly used in clinical settings, notes Dr. Ragothaman, who cautions that prior antibiotic treatment can inhibit the growth of bacteria on agar plates. He adds there may be pre-selection bias with culture because clinicians must employ different culture methods to grow certain types of bacteria, noting identification of acid-fast bacteria as one example. Growth of bacteria takes days to reveal itself and Dr. Ragothaman notes this can be problematic in cases of severe infection, which prompts the use of empiric antibiotic therapy and contributes to antibiotic resistance.
Poster coauthor Paul Kim, DPM, MS, FACFAS, emphasizes putting the use of any bacterial detection method in context. As he says, infection detection and eradication depends on a combination of factors including cultures, laboratory values, radiographic findings, and history and physical examination. “Thus a gestalt approach is needed (as opposed to relying on) a single method,” says Dr. Kim, an Associate Professor in the Department of Plastic Surgery at MedStar Georgetown University Hospital in Washington, DC.
Are Patients With Diabetes More At Risk Of TAR Complications?
By Brian McCurdy, Managing Editor
 Patients with diabetes had similar complications to those without diabetes who had total ankle replacement (TAR), according to a recent study.
Patients with diabetes had similar complications to those without diabetes who had total ankle replacement (TAR), according to a recent study.
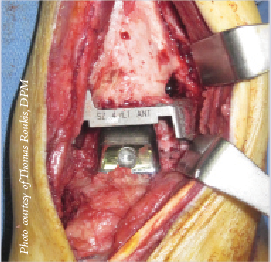
The poster study, presented at the ACFAS Scientific Conference, focused on 13 patients with diabetes who received TAR as well as 15 TAR patients without diabetes. Among patients with diabetes, the authors noted two complications of wound dehiscence. The poster notes two patients without diabetes had complications, namely deep infection.
James Cottom, DPM, FACFAS, the lead author of the poster study, says when considering TAR in patients with diabetes, surgeons should be wary if such patients have uncontrolled diabetes (HbA1c above 6), peripheral neuropathy, a history of ulceration or Charcot.
Dr. Cottom cites technological advances in TAR that have led to the lower level of complications. These include streamlining of the procedure, facilitating less tourniquet time and less invasive procedures, notes Dr. Cottom, the Fellowship Director of Florida Orthopedic Foot and Ankle Center in Sarasota, Fla.
Dr. Cottom proposes future studies of TAR complications on several patient populations. He notes these studies could include a comparison of complication rates between specific implants or complication rates of surgeons performing a high volume of TAR in comparison with a low volume. Dr. Cottom also proposes research into TAR for tobacco users. He says his data shows a complication rate of over 45 percent in 11 active smokers as well as a 24 percent complication rate in patients with a smoking history in comparison with a 20 percent complication rate in non-smokers.
Study: Dialysis Does Not Increase Ulcer Or Amputation Risk
By Brian McCurdy, Managing Editor
 Although hemodialysis can be associated with a higher risk of lower extremity ulcers and amputations, a recent study notes that after patients with diabetes start dialysis, there is no increase in the risk of lower extremity ulcers or amputations.
Although hemodialysis can be associated with a higher risk of lower extremity ulcers and amputations, a recent study notes that after patients with diabetes start dialysis, there is no increase in the risk of lower extremity ulcers or amputations.
The study, published in the Journal of the American Podiatric Medical Association, focused on 150 consecutive patients with diabetes on dialysis. Researchers compared the incidence of foot complications 30 months before and after patients started dialysis. To account for multiple events in the same patient over time, researchers contrasted the initial and cumulative incidence of ulcers and amputation.
The study authors found no significant difference in the incidence of first foot ulcers before and after patients started dialysis, but did note the incidence of cumulative ulcers was significantly higher before dialysis. The authors noted no difference in the incidence of first amputation and no difference in the cumulative incidence of amputations before and after dialysis.
Khurram Khan, DPM, notes that as the study found no increased incidence of ulcers in patients with diabetes before and after starting dialysis, the study results should have no impact on treatment decisions by podiatric physicians.
However, Dr. Khan does note podiatric physicians may need to take special consideration when patients on dialysis need antibiotics as antibiotic treatment in this population may depend on their dialysis days and number of hours. Therefore, patients with diabetic foot ulcers undergoing dialysis who need antibiotics would require input from the nephrologist in charge of the patient’s care, according to Dr. Khan, an Associate Professor in the Department of Podiatric Medicine at the Temple University School of Podiatric Medicine.











