How To Diagnose And Treat Subluxing Peroneal Tendons In The Athlete
Commonly misdiagnosed as lateral ankle sprains, peroneal tendon subluxation can be a challenging dilemma for skiers, basketball players and football players among other athletes. With this in mind, these authors review a grading system for these injuries, discuss common diagnostic findings and offer keys to effective treatment.
 Subluxations or dislocations of the peroneal tendons, although not rare, are a relatively uncommon phenomenon in the realm of the foot and ankle. However, particularly in the athlete population, injury to the superior peroneal retinaculum and/or acute peroneal tendon dislocations often go unrecognized or misdiagnosed as “lateral ankle sprains.”1 Consequently, this can potentially result in chronic instability, which requires surgical correction.
Subluxations or dislocations of the peroneal tendons, although not rare, are a relatively uncommon phenomenon in the realm of the foot and ankle. However, particularly in the athlete population, injury to the superior peroneal retinaculum and/or acute peroneal tendon dislocations often go unrecognized or misdiagnosed as “lateral ankle sprains.”1 Consequently, this can potentially result in chronic instability, which requires surgical correction.
The peroneal tendons run along the lateral aspect of the leg where the peroneus brevis tendon courses medially and anteriorly to the peroneus longus tendon. At the distal portion of the fibula, the peroneal tendons run through a sulcus on the posterior aspect of the bone. In a cadaveric anatomical study, Edwards found that 82 percent of the cadavers had a concave sulcus, 11 percent had a flat sulcus and 7 percent had a convex sulcus.2
The depth of the groove is variable (2 to 4 mm) while the width normally ranges from 5 to 10 mm. The groove itself is accentuated by an osseous ridge that is covered by a fibrocartilaginous cap, thereby adding 2 to 4 mm to the overall depth of the sulcus. Anatomically, in addition to the fibular groove, another restraint against subluxation or dislocation of the peroneal tendons is the superior peroneal retinaculum. This courses from the tip of the lateral malleolus and attaches to the calcaneus and fascia along the Achilles tendon.2
Peroneal tendon injuries secondary to lower extremity trauma have been well recognized and studied. The three primary peroneal tendon disorders are tendinopathy (tendinitis and tendinosis), tendon subluxation and tendon tears.
Peroneal tendon subluxation typically occurs in athletes with a sudden forceful dorsiflexion and inversion of the ankle. This causes rapid contraction of the peroneus longus and brevis muscles, potentially leading to further damage of the superior peroneal retinaculum. In the past, the sport most associated with this injury was alpine skiing, which correlates with the premise of forced dorsiflexion and acute muscle contraction against a fixed ankle in a ski boot.3 However, recent literature does suggest that peroneal tendon subluxation can occur with those in several other sports, including football, soccer, basketball, baseball, softball and tennis.4
Furthermore, chronic subluxations can occur in patients with recurrent ankle sprains. In these cases, the chronic stretching of the superior peroneal retinaculum can allow expansion of the retrofibular ligamentous structures, which predisposes the tendons to roll around each other without any constraints. Over time, this can predispose the tendons to longitudinal splits and worsening of the subluxation.5
Differentiating The Grades Of Peroneal Tendon Subluxation
We can first distinguish peroneal tendon subluxations as either acute or chronic. Subsequently, we can differentiate the injury into grades based on the Eckert and Davis classification.6
 Grade I. The retinaculum is elevated from the lateral malleolus with the tendons lying between the bone and periosteum.
Grade I. The retinaculum is elevated from the lateral malleolus with the tendons lying between the bone and periosteum.
Grade II. The fibrocartilaginous ridge is elevated with the retinaculum attached and the tendons displaced beneath the ridge.
Grade III. A thin cortical fragment is avulsed from the fibula with the tendons displaced beneath the fibular fragment.
Grade IV. The retinaculum is avulsed or ruptured from the posterior attachment, causing the retinaculum to be deep to the dislocating tendons.
What You Should Know About Intrasheath Subluxations
In the literature, there have also been documented cases of intrasheath subluxations in which the peroneus brevis rises atop of the peroneus longus within the tendon sheath.7 These subluxations tend to be associated with a history of chronic ankle sprains or chronic lateral ankle pain. Thomas and colleagues noted that this intrasheath subluxation was associated with either a low-lying peroneal muscle belly or a peroneus quartus tendon.7
A low lying muscle belly is an unusual anomaly, most commonly associated with the peroneus brevis tendon.8 In the case of the peroneus brevis muscle, it is expected that the muscle would end an average of 1.6 to 2.0 cm above the distal tip of the fibula.2
 A few published studies have supported the presence of a low-lying muscle belly as an etiology for a peroneal tendon tear. Recently, Mirmiran and coworkers explored the association between a low lying peroneus brevis muscle belly and peroneal tendon subluxation.9 Although the presence of a low lying peroneus brevis muscle belly did not show a statistically significant association with peroneus brevis tendon subluxation, of the 10 patients with an intraoperatively observed tendon subluxation, nine had a concomitant low lying peroneus brevis muscle belly. Furthermore, a low lying peroneus brevis muscle belly was present intraoperatively in 62 percent of the patients with chronic lateral ankle pain.
A few published studies have supported the presence of a low-lying muscle belly as an etiology for a peroneal tendon tear. Recently, Mirmiran and coworkers explored the association between a low lying peroneus brevis muscle belly and peroneal tendon subluxation.9 Although the presence of a low lying peroneus brevis muscle belly did not show a statistically significant association with peroneus brevis tendon subluxation, of the 10 patients with an intraoperatively observed tendon subluxation, nine had a concomitant low lying peroneus brevis muscle belly. Furthermore, a low lying peroneus brevis muscle belly was present intraoperatively in 62 percent of the patients with chronic lateral ankle pain.
The senior author has found this to be the case as well. Any patient with magnetic resonance image (MRI) findings of a low lying muscle belly and pain in this region receives counseling on excision.
Essential Diagnostic Insights
In terms of diagnosis, the athlete often recalls a significant episode of trauma with an acute subluxation. The athlete may feel a painful snapping sensation with pain localized to the retromalleolar area. Unlike an ankle sprain, the mechanism of injury as the patient tells it is often vague. With chronic instability, patients elicit a generalized history of “recurrent sprains.” The athlete might complain of snapping or popping, or instability on uneven ground.
When it comes to the physical examination, physicians often miss peroneal tendon subluxation unless they specifically evaluate it. Acutely, a variable amount of edema and ecchymosis may be present in the retrofibular region, which can obscure the dislocated peroneal tendons. In contrast to an ankle sprain, pain is localized to the posterior aspect of the fibula more proximally and posteriorly. Furthermore, with passive circumduction of the ankle, one may identify subluxation. The clinician may elicit pain posterior to the fibula with tensing of the peroneals when asking the athlete to dorsiflex and evert the foot and ankle.
Imaging modalities of the injured ankle can be helpful in determining the diagnosis of peroneal tendon instability. Routine AP, lateral and mortise radiographs tend to be negative, but can demonstrate a small fleck of fibular cortex, correlating to a grade III injury, which is pathognomonic of a peroneal tendon subluxation or dislocation. Ankle stress views may be beneficial to evaluate for instability, especially in cases of chronic peroneal tendon subluxations. Moreover, ultrasound evaluation can be confirmatory when the foot is dorsiflexed and everted. However, this requires the skilled hands of an experienced sonologist.
In most cases, one should obtain an MRI as it is beneficial in assessing a concomitant peroneal tendon injury. In a study by Park and colleagues, MRI was 83.9 percent sensitive and 74.5 percent specific for identifying peroneal tendon pathologic entities, such as peroneus brevis tenosynovitis, tendon tear and a low lying muscle belly.10
However, MRI still remains a poor imaging study for the presence of a tendon subluxation since it is a static imaging tool while peroneus tendon subluxation is a dynamic finding. Recently, VanPelt and coworkers used kinematic MRI to evaluate for peroneal tendon subluxation during unconstrained foot and ankle motion in the scanner using a T2-weighted pulse sequence.11 With circumduction, lateral dislocation of the peroneal tendons from the groove with a discontinuous and retracted superior peroneal retinaculum may be present.
Although an MRI with added kinematic evaluation can aid in diagnosing peroneal tendon subluxation, do not solely rely on MRI as a source to determine the necessity of surgical intervention.
 Pertinent Pointers On Treating Peroneal Subluxation
Pertinent Pointers On Treating Peroneal Subluxation
Although non-surgical treatment is always an option, it has a high failure rate, with patients requiring eventual surgery at a rate ranging from 44 to 74 percent.12 Since these injuries tend to occur in young adults and athletes who generally want a speedy recovery, surgical reconstruction has a much higher success rate in comparison to non-surgical treatment.
In terms of surgery for an acute peroneal tendon dislocation, the treatment of choice is direct reattachment of the superior peroneal retinaculum to the posterior periosteum of the fibula. With this technique, the surgeon places multiple drill holes vertically through the fibular cortex. Pass non-absorbable braided sutures through the superior peroneal retinaculum, thereby securing the retinaculum to the ridge. McCarvey and colleagues noted an approximately 96 percent success rate with this technique.13
Postoperatively, the athlete is to be non-weightbearing in slight equinus and eversion in a splint for the first two weeks and then transitions to weightbearing as tolerated in a controlled ankle motion (CAM) boot for the following four weeks. Finally, the athlete transitions into a stirrup ankle brace and begins physical therapy at six weeks.
For athletes with chronic peroneal tendon subluxation, researchers have advocated multiple surgical methods, including superior peroneal retinaculum reinforcement and repair, tendon rerouting techniques, and groove deepening procedures.13
Tendon rerouting or tissue transfer techniques aim to reinforce the incompetent superior peroneal retinaculum and aid in retaining the peroneal tendons. These are often revision procedures with a significant amount of fibrosis and atypical anatomy. Authors have described multiple options, including repairs with Achilles tendon slips, calcaneofibular ligament slips, calcaneofibular flap transpositions and peroneus brevis tendon slips.14–17 Bone block or fibular osteotomies may help prevent further subluxation and dislocation.18 However, these are salvage procedures that require osseous union, which can consequently delay postoperative physiotherapy and the athlete’s return to sport. Additionally, the senior author has seen impingement with these procedures.
 Groove deepening has become a well integrated technique to indirectly reduce the tendency of the peroneal tendons to sublux in a shallower retromalleolar groove. Not only it is an excellent option to correct peroneal tendon subluxation, groove deepening is also a viable option in patients with chronic retrofibular peroneal pain without obvious tendon or groove pathology. Biomechanically, Title and colleagues noted that the pressures over the distal 2 cm of the posterior fibula just proximal to the calcaneofibular ligament decreased significantly after the procedure.19
Groove deepening has become a well integrated technique to indirectly reduce the tendency of the peroneal tendons to sublux in a shallower retromalleolar groove. Not only it is an excellent option to correct peroneal tendon subluxation, groove deepening is also a viable option in patients with chronic retrofibular peroneal pain without obvious tendon or groove pathology. Biomechanically, Title and colleagues noted that the pressures over the distal 2 cm of the posterior fibula just proximal to the calcaneofibular ligament decreased significantly after the procedure.19
In another study, Saxena and coworkers retrospectively analyzed 31 patients who had either an isolated subluxation repair, subluxation repair plus peroneus brevis repair or subluxation repair plus lateral ankle stabilization.20 Overall, the athletes had an average American Orthopedic Foot and Ankle Society (AOFAS) score of 97.0 postoperatively and were able to return to athletic activity in their sport in approximately three months. However, they did note that those with concomitant tendon tears took longer to recover.
Furthermore, Porter and colleagues studied results of groove deepening and retinaculum repair in 13 athletes. They also noted an average time to return to sports of approximately three months. Overall, eight of the patients were able to return to their pre-injury level of activity whereas the other five patients resumed at a level lower than desired. They concluded that groove deepening with retinaculum repair prevented instability and enabled nearly normal ankle range of motion.21 Furthermore, for patients with a low lying peroneus brevis muscle belly, the authors noted it was imperative to resect any muscle tissue that extends distally into the peroneal groove as this muscle tissue tends to be present in those with a flat or convex posterior margin of the fibula.
A Guide To The Authors’ Surgical Technique
Our preferred treatment for peroneal tendon subluxation in athletes is to deepen the fibular groove, remove the low lying muscle belly (if necessary) and tighten the superior peroneal retinaculum. Specifically, this involves sharp excision of the superior peroneal retinaculum from the posterolateral border of the fibula.
At this time, inspect the peroneal tendons for any tears or thickening. Furthermore, if a low lying muscle belly is present, debride and resect it. If tendon pathology is present, address the pathology with debridement and retubularization with non-absorbable sutures buried within the substance of the tendon. Do not leave sutures proud or in contact with the adjacent tendon. The senior author advocates a “less is more” approach to repairing tendons and prefers to utilize less suture in the tendon for repair. The feeling is that this prevents the potential for intratendinous xanthoma/foreign body reaction and reduces future tendinosis.
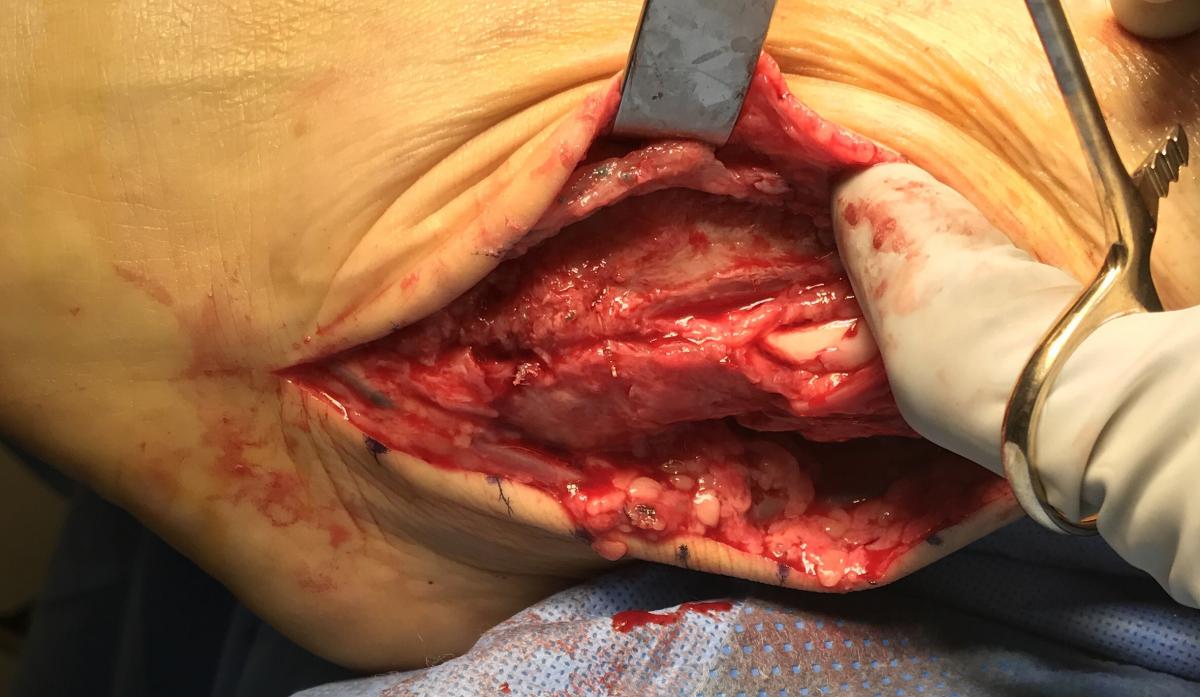 Next, inspect and deepen the retromalleolar groove. With the tendons retracted, make a sharp periosteal incision at the tip of the fibula and insert a 4.0 to 5.5 mm solid drill into the fibula under fluoroscopic guidance. Then ream the distal 2 to 3.5 cm of the fibular just deep to the desired groove. Use a rounded or blunted end of a bone tamp to gently impact and deepen the posterior aspect of the fibula approximately 6 to 8 mm to prevent dislocation. Take care not to fracture the area, which may require multiple light taps in the same area. The surgeon should avoid “dimple fracturing” the area. We prefer to invaginate the area smoothly and evenly so as to leave the area free of osseous ridges that may impinge or abrade the peroneals.
Next, inspect and deepen the retromalleolar groove. With the tendons retracted, make a sharp periosteal incision at the tip of the fibula and insert a 4.0 to 5.5 mm solid drill into the fibula under fluoroscopic guidance. Then ream the distal 2 to 3.5 cm of the fibular just deep to the desired groove. Use a rounded or blunted end of a bone tamp to gently impact and deepen the posterior aspect of the fibula approximately 6 to 8 mm to prevent dislocation. Take care not to fracture the area, which may require multiple light taps in the same area. The surgeon should avoid “dimple fracturing” the area. We prefer to invaginate the area smoothly and evenly so as to leave the area free of osseous ridges that may impinge or abrade the peroneals.
At this point, the retinaculum is amenable to direct repair. In most cases, elevate a periosteal flap from the fibula to assist in suture repair with the superior peroneal retinaculum as this allows for stronger reinforcement. Pay close attention to avoid inadvertently suturing the tendons when repairing the retinaculum. Postoperatively, if the peroneal tendons did not require significant repair, permit the patient to bear weight early in a boot at two weeks and perform passive range of motion (ROM) at seven to 10 days as tolerated. If significant repair of the tendons is required, passive ROM may begin at two weeks as tolerated with a return to full weightbearing at four weeks instead.
The most common complication for peroneal subluxation in the athletic population is redislocation, which tends to be higher in the non-surgical group. Other reported complications include decreased ankle range of motion, degenerative tendon tears, friction on the tendon (after repair) and sural nerve injury.5
In Summary
Management of subluxing or dislocating peroneals in an acute or chronic situation in an athlete or highly active patient involves prompt diagnosis and surgical intervention. We recommend performing a thorough physical examination and analyzing advanced imaging. Although more prospective studies need to occur, we have noted reasonable success with operative correction in the method of direct repair of the superior peroneal retinaculum, removal of the low lying muscle belly (if present) and a deepening of the fibular groove.
Dr. Chauhan is a Fellow with the Pennsylvania Intensive Lower Extremity Fellowship at Premier Orthopaedic and Sports Medicine in Malvern, Pa.
Dr. Miller is the Residency Director of Phoenixville Hospital Podiatric Medicine and Surgery Residency/Reconstructive Rearfoot/Ankle Surgery Program in Phoenixville, Pa. He is an Adjunct Associate Professor in the Department of Surgery at the Temple University School of Podiatric Medicine. Dr. Miller is the Director of the Pennsylvania Intensive Lower Extremity Fellowship Program at Pennsylvania Orthopaedic Center in Malvern, Pa.
References
- Arrowsmith SR, Fleming LL, Allman FL. Traumatic dislocations of the peroneal tendons. Am J Sports Med. 1983; 11(3):142-146.
- Edwards M. The relations of the peroneal tendons to the fibula, calcaneus, and cuboideum. Am J Anat. 1928; 42:213-253.
- Oden RR. Tendon injuries about the ankle resulting from skiing. Clin Orthop Relat Res. 1987; 216:63-69.
- Safran MR, O’Malley D Jr, Fu FH. Peroneal tendon subluxation in athletes: new exam technique, case reports, and review. Med Sci Sports Exerc. 1999; 31(7 Suppl):S487-S492.
- Coughlin MJ, Mann R. Surgery of the Foot and Ankle, Seventh Edition, volume 2. Mosby, St. Louis, 1999, pp. 818-826.
- Eckert W, Davis E. Acute rupture of the peroneal retinaculum. J Bone Joint Surg. 1976; 58(5):670-673.
- Thomas JL, Lopez-Ben R, Maddox J. A preliminary report on intra-sheath peroneal tendon subluxation: a prospective review of seven patients with ultrasound verification. J Bone Joint Surg Am. 1989; 71:293-295.
- Geller J, Lin S, Cordas D, Vieira P. Relationship of a low-lying muscle belly to tears of the peroneus brevis tendon. Am J Orthop. 2003; 32(11):541-544.
- Mirmiran R, Squire C, Wassell D. Prevalence and role of a low-lying peroneus brevis muscle belly in patients with peroneal tendon pathologic features: a potential source of tendon subluxation. J Foot Ankle Surg. 2015; 54(5):872-875.
- Park HJ, Cha SD, Kim HS, Chung ST, Park NH, Yoo JH, Park JH, Kim JH, Lee TW, Lee CH, Oh SM. Reliability of MRI findings of peroneal tendinopathy in patients with chronic ankle instability. Clin Orthop Surg. 2010; 2(4):237-243.
- VanPelt MD, Landrum MR, Igbinigie M, Wadhwa V, Chhabra A. Kinematic magnetic resonance imaging of peroneal tendon subluxation with intraoperative correlation. J Foot Ankle Surg. 2017; 56(2):395-397.
- Escalas F, Figueras JM, Merino JA. Dislocation of the peroneal tendons. Long-term results of surgical treatment. J Bone Joint Surg Am. 1980; 62(3):451-453.
- McGarvey W, Clanton T. Peroneal tendon dislocations. Foot Ankle Clin. 1996; 1(2):325-342.
- Jones E. Operative treatment of chronic dislocation of the peroneal tendons. J Bone Joint Surg Am. 1932; 14:574-576.
- Platzgummer H. [On a simple procedure for the operative therapy of habitual peroneal tendon luxation]. Arch Orthop Unfallchir. 1967; 61(2):144-150.
- Pozo JL, Jackson AM. A rerouting operation for dislocation of peroneal tendons: operative technique and case report. Foot Ankle. 1984; 5(1):42-44.
- Martens MA, Noyez JF, Mulier JC. Recurrent dislocation of the peroneal tendons. Results of rerouting the tendons under the calcaneofibular ligament. Am J Sports Med. 1986; 14(2):148-150.
- Larsen E, Flink-Olsen M, Seerup K. Surgery for recurrent dislocation of the peroneal tendons. Acta Orthop Scand. 1984; 55(5):554-555.
- Title CI, Jung HG, Parks BG, Schon LC. The peroneal groove deepening procedure: a biomechanical study of pressure reduction. Foot Ankle Int. 2005; 26(6):442-446.
- Saxena A, Ewen B. Peroneal subluxation: surgical results in 31 athletic patients. J Foot Ankle Surg. 2010; 49(3):238-241.
- Porter D, McCarroll J, Knapp E, Torma J. Peroneal tendon subluxation in athletes: fibular groove deepening and retinacular reconstruction. Foot Ankle Int. 2005; 26(6):436-441.
For further reading, see “How To Manage Peroneal Tendon Subluxation” in the September 2013 issue of Podiatry Today or “Keys To Diagnosing And Treating Peroneal Tendon Dysfunction” in the March 2017 issue.
For other related articles, visit the archives at www.podiatrytoday.com











