How To Attest To Meaningful Use In 2016
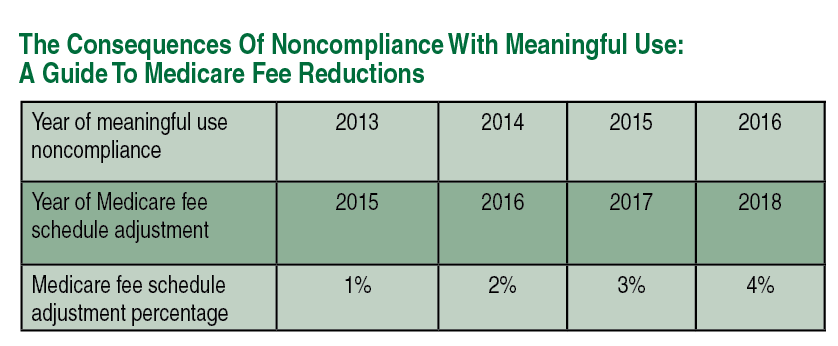
Failure to successfully attest to meaningful use in 2016 will result in a 4 percent reduction of your Medicare Part B Physician Fee Schedule in 2018. The meaningful use program is currently scheduled to end January 1, 2017 but is still in effect for 2016.
Some providers are still eligible for incentive payments based on compliance with the meaningful use program. If 2012, 2013 or 2014 was your first year participating in the meaningful use program, you are eligible for incentive payments for demonstrating 2016 compliance. If your first year reporting was any year other than these three years, you are not eligible for incentive payments based on 2016 participation.
As this issue went to press, the reporting period for 2016 meaningful use for all eligible providers (other than those for whom 2016 is their first year reporting) is still one full calendar year. The reporting period for providers for whom 2016 is their first year reporting meaningful use is any consecutive 90-day period. On July 6, 2016, the Centers for Medicare and Medicaid Services (CMS) issued a proposed rule that would shorten the reporting period to 90 consecutive days for all eligible providers. This will be subject to a 60-day comment period and CMS will then release a final rule some time after that. If you have done nothing for meaningful use thus far and the reporting period does get shortened to 90 days, it is not too late for you to report and avoid the payment reduction in 2018. For a multitude of reasons, it is easier to meet the criteria for a 90-day reporting period than it is for a full-year reporting period.
All eligible providers are in modified stage 2 for 2016. The modified stage 2 objectives are easier to achieve than the objectives in stage 2 in its original description. Measures are no longer broken down into “core” and “menu set.” There are no elective measures.
 A Closer Look At Ten Key Objectives
A Closer Look At Ten Key Objectives
Let us take a closer look at the 10 objectives necessary to achieve meaningful use in 2016.
Objective 1: protect electronic health information. This requires a security risk analysis. Whoever performs the risk analysis needs to ensure that it meets the stringent requirements of this measure’s description. Provide documentation of what you did, what risks you identified and the steps you took to address identified risks.
Objective 2: clinical decision support. There are two measures to this objective. The first is to implement five clinical decision support interventions related to four or more clinical quality measures at a relevant point in patient care. There are many clinical quality measures relevant to podiatry from which you can choose. If you are unsure how to develop these clinical decision support rules using your electronic health records (EHR), you can get assistance with this from your EHR vendor. The second requirement of objective 2 is to enable and implement the functionality for checking potential drug-drug and drug-allergy interactions.
Objective 3: computerized physician order entry (CPOE). There are three measures to this objective. The first is that you must record more than 60 percent of medication orders using CPOE. E-prescribing a medication is an example of CPOE. Another example would be creating the medication order within the EHR and printing out the prescription onto paper. The second measure of this objective is that the provider must create more than 30 percent of her laboratory orders using CPOE. Examples of this would be entering an order for HgA1c through the EHR and then transmitting that order electronically to the lab or having the EHR print out the order. The final measure of this objective is that you must record more than 30 percent of radiology orders using CPOE. Examples of this are similar to those described above for the laboratory orders.
There are potential exclusions to each of these measures and one should consider each separately. A provider who prescribes fewer than 100 medications during the reporting period is exempt from the first measure of objective 3. A provider who writes for fewer than 100 laboratory orders during the reporting period is exempt from the second measure of objective 3. A provider who orders fewer than 100 radiology exams during the reporting period is exempt from the third measure of this objective. At the end of the reporting period, if you find you were exempt from any of these measures, you will have the opportunity to indicate that when it is time to attest. It is more likely you will qualify for these exclusions in a 90-day reporting period than in a full-year reporting period.
Objective 4: electronic prescribing. This objective requires that the provider consult a drug formulary for more than 50 percent of all permissible prescriptions and transmit these prescriptions electronically, using certified EHR technology, to the patient’s pharmacy. You qualify for an exclusion to this requirement if you write fewer than 100 permissible prescriptions during the EHR reporting period or if you do not have a pharmacy within your organization, and there are no pharmacies that accept electronic prescriptions within 10 miles of your practice location at the start of the EHR reporting period. Similar to objective 3, it is more likely you will qualify for this exclusion in a 90-day reporting period than in a full-year reporting period.
Objective 5: summary of care record. This objective requires that 10 percent of the times a provider transitions or refers a patient to another setting or provider of care, he or she must utilize the EHR to create a summary of care record and electronically transmit this summary of care record to the receiving provider. The summary of care record should contain the following items:
 • Patient name
• Patient name
• Provider’s name and office contact info
• Current problem list
• Past medical history
• Procedures
• Laboratory test results
• Current medication list and medication history
• Current medication allergy list and medication allergy history
• Vital signs (height, weight, blood pressure, body mass index, growth charts)
• Smoking status
• Demographic information (preferred language, sex, race, ethnicity, date of birth)
• Care plan field(s), including goals and instructions, and any known care team members including the primary care provider of record.
The second measure of this objective is the provider must electronically transmit this summary of care record to the receiving provider for more than 10 percent of all transitions of care and referrals that occur. Providers who transfer a patient to another setting or another provider less than 100 times during the EHR reporting period will be able to claim an exclusion from this objective. This is another exception you are more likely to qualify for in a 90-day reporting period than in a full-year reporting period.
Objective 6: patient-specific education. In order to meet this objective, the provider must supply patient-specific education resources — identified by certified EHR technology — to more than 10 percent of all unique patients. Ideally, this is set up for the EHR to “know” when one should provide the educational resource. Different ways of accomplishing this objective include using a certain key word within the body of a note, using a certain template or perhaps using a certain ICD code.
Objective 7: medication reconciliation. To meet this objective, the provider must perform medication reconciliation for more than 50 percent of patients who transition into the care of the provider. Your EHR should give you the ability to track how many patients transition into the practice and when medication reconciliation occurs.
Objective 8: patient electronic access. The first component of this measure is that at least 50 percent of all unique patients the provider sees during the EHR reporting period receive online access to their health information within four business days after the information is available to the provider. “Health information” refers to the same list that you needed for the summary of care record in objective 5. (Note that the provider may choose to withhold certain information if she or he feels it is not safe or appropriate to share with the patient.) The provider merely needs to make the information available to access it online. The provider does not need to send it directly to the patient.
The second component of this measure is at least one patient seeing the provider during the EHR reporting period must view, download or transmit his or her health information to a third party. Having just one patient access and view health information available online as part of the first component of this objective will satisfy this requirement.
Objective 9: secure electronic messaging. This requires having the capability for patients to exchange secure electronic messages with the provider fully enabled throughout the EHR reporting period. No message actually needs to be exchanged.
Objective 10: public health reporting. This objective has three measures. Podiatrists are exempt from the first two measures because these measures deal with situations podiatrists do not encounter. Measure three requires the provider to be in active engagement to submit data to a specialized registry. Podiatrists are not exempt from this measure in 2016 as there are multiple registries for conditions we treat.
There are multiple registries to which you may choose to submit data. Submitting a Physician Quality Reporting System (PQRS) measure group through a registry does not satisfy the requirements of meaningful use objective 10, measure 3. Submitting data to a registry to satisfy the requirements of objective 10, measure 3 usually involves uploading and sharing a large volume of summary of care documents and/or continuity of care documents from your EHR to the registry. The American Podiatric Medical Association (APMA) is collaborating with the US Wound Registry and MedXpress Specialty Registry so both registries offer a discounted price to APMA members. Submitting data to a registry that collaborates with the APMA may help provide the APMA with information that can be helpful for public policy efforts.
The final step to achieving meaningful use in 2016 is to report clinical quality measures (CQMs). You must report nine CQMs covering at least three National Quality Strategy (NQS) domains. This is something your EHR should be tracking for you. Differing from all of the aforementioned requirements, there are no thresholds for these, meaning there is no percentage “cutoff” you have to meet.
In Summary
Meaningful use as we know it is scheduled to end January 1, 2017. It will be replaced with Advancing Care Information, which will incorporate components of meaningful use and account for 25 percent of your 2017 Merit-Based Incentive Payment System score. It is still imperative to meet the requirements of meaningful use in 2016 if you want to avoid a 4 percent reduction to your Medicare Part B Physician Fee Schedule in 2018.
Dr. Lehrman is a Fellow of the American Academy of Podiatric Practice Management (AAPPM), serves as an expert panelist on Codingline.com and is on the APMA Coding Committee. Follow him on Twitter @DrLehrman .
Dr. Lehrman has no conflict of interest or financial relationship with the US Wound Registry or MedXpress Specialty Registry.
References
1. American Podiatric Medical Association. EHR incentive programs: what’s next? APMA News. Available at https://www.apma.org/WorkingForYou/NewsDetail.cfm?ItemNumber=19610 .
2. Slavitt A, DeSalvo K. EHR incentive programs: where we go next. The CMS Blog. Available at https://blog.cms.gov/2016/01/19/ehr-incentive-programs-where-we-go-next/ . Published Jan. 19, 2016.











