A Guide To Posterior Ankle Arthroscopy In Athletes
In September 2019, Theodoulou presented an article on posterior ankle arthroscopy in Podiatry Today.1 He focused primarily on the harvest of the flexor hallucis longus tendon for other purposes but nicely highlighted posterior ankle arthroscopy in general. My goal in this column is to focus more on the posterior ankle pathology that athletes often experience and the benefits of posterior ankle arthroscopy in those cases.
Posterior ankle arthroscopy is something that we read about and teach, but I question how often podiatrists perform this procedure. It seems that we see a significant amount of posterior ankle pathology on imaging but rarely see patients who have posterior ankle pain exclusively. I performed a review of all my posterior ankle scope cases as well as my ankle magnetic resonance imaging (MRI) exams over the past few years. I found myself amazed at the volume of posterior ankle pathology but shocked that the pathology did not correlate with patient symptoms. Based on these findings, I think we need to ask a key question: Are we simply missing pathology or are we avoiding posterior ankle arthroscopy?
Many authors have looked at combined anterior and posterior ankle arthroscopy with Lui being one of the most prolific authors on foot and ankle arthroscopy. He actually performs his posterior ankle arthroscopy with the patient in a supine position so he can easily move back and forth to the anterior ankle.2 Obviously, he utilizes a different approach than the traditional two-portal posterior Achilles technique.2,3 Lui also describes a lateral portal technique, which lends itself to supine positioning.3 After 27 years, I can’t recall ever combining anterior and posterior ankle arthroscopy during the same case. However, I have performed posterior ankle and subtalar or endoscopy cases together.
What Are The Indications For Posterior Ankle Arthroscopy?
More and more surgeons are advocating for the use of posterior ankle arthroscopy to address posterolateral and posteromedial talar dome lesions or posterior tibial pathology.4 While I have never needed to take a posterior approach for posteromedial talar dome lesions, I have utilized posterior arthroscopy for better access to posterolateral lesions that are classically more posterior lesions. For many surgeons accustomed to performing medial malleolar osteotomies, posterior ankle arthroscopy, in my opinion, presents far less issues and complications. I would think a patient, given the choice of a tibial osteotomy and large open incisions versus a posterior ankle arthroscopy, would easily opt for this less invasive method.
Indications for posterior ankle arthroscopy are no different than what we covered in each of our last four “Sports Medicine” columns on arthroscopy. The majority of pathology we see in our athletes and soldiers are the classic soft tissue impingement issues related to synovitis and osseous impingement related to a posterior talar process, os trigonum or posterior tibial osteophytes.1-14 It is a rarity to see pathology posteriorly related to the posterior facet unless it is post-traumatic or something rare like pigmented villonodular synovitis (PVNS) or synovial chondromatosis. Our focus in this column includes the routine issues like impingement.
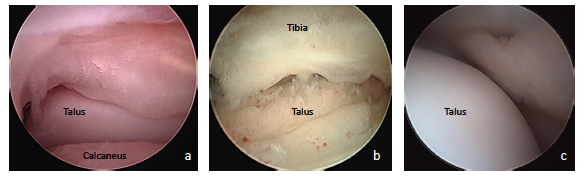
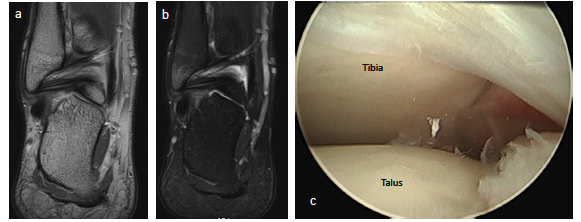
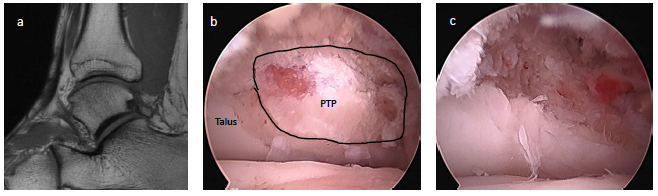
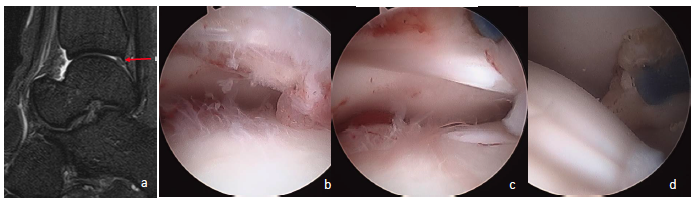
Posterior ankle impingement in athletes is often related to a previous sprain.7,11,12,15,16 Many times, soldiers who sustained syndesmosis injuries can develop a combination of soft tissue impingement lesions not only anteriorly but posteriorly as well (see first photo set above). We also see clicking, popping and snapping of the posterior tibiofibular ligament and posterior talofibular ligament in these cases. In a sense, we can see a posterior pseudo-version of Bassett’s ligament although this is not named as such. Whether this is a fraying of the ligament which now impinges on the posterior tibial lip or a true accessory ligament is not well-defined. Regardless, the imaging is often clear on MRI and intra-operatively (see second image set above). Almost every author states that symptoms always or only occur with plantarflexion, but I tend to see far more soldiers and athletes complaining of pain with dorsiflexion. To me, pain with stretching of the posterior capsule and distraction of the offending tissue makes far more sense that hurting with only plantarflexion.
Many authors focus much of their attention on os trigonums and posterior talar process fractures that do tend to hurt more with plantarflexion.8,10,13,15 However, in my long history of studying accessory bones, the number of huge, truly symptomatic os trigonums is very low in our community in comparison to the number of os tibiale externums and os peroneums that we excise. Regardless, posterior ankle arthroscopy or posterolateral arthroscopy is ideal for removing these fragments. Numerous authors discuss performing these in a supine or lateral position versus prone. I rarely choose supine or lateral unless I also plan on performing subtalar or anterior ankle arthroscopy. I am much more comfortable utilizing the posterior Achilles portals from a prone position. As with anything, you will find an assortment of techniques and positions that surgeons utilize, with the same goal of attempting to remove the fragment.
Pertinent Pearls On Intraoperative Technique
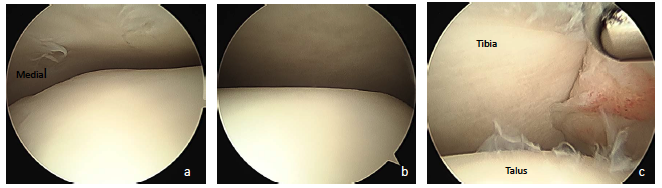
Surgeons may utilize a multitude of scope sizes from 2.7 to 4.0 mm.4 Whether it is a zero, 30 or 70 degree apparatus depends on your comfort level. Goals are very simple once you are in the joint. Just like we do for the anterior ankle, we need to identify our landmarks and work systematically from one side to the next. I tend to utilize the posterolateral portal for the camera first prior to proceeding medially. I prefer to use a spinal needle and attempt to put the needle on the lateral side of the flexor hallucis longus tendon. I figure as long as I stay lateral to this tendon, I cannot hurt anything medially like the neurovascular bundle (see third photo above).
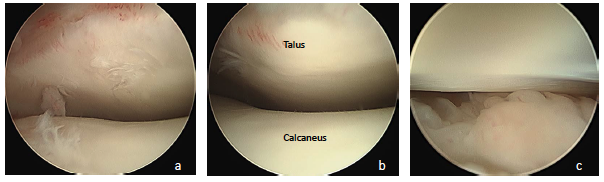
Once I am in the posterior space I can inspect the ankle laterally and centrally. Simply dorsiflexing the ankle widens the space. By switching the scope to the medial portal, you can inspect the medial joint and easily visualize the deep deltoid ligament. Just like one would do with the anterior ankle, surgeons can divide the joint into medial, central and lateral quadrants (see fourth photo set above). Once the surgeon is done with the ankle joint, proceed inferiorly to inspect the posterior talar process/os trigonum and, if necessary, the posterior facet (see fifth photo set above).
Key Examples Of Application Of Posterior Ankle Arthroscopy
In one case, a 17-year-old football player sustained a posterior talar process fracture when another player rolled on top of his ankle from behind. Despite conservative treatment with four weeks of casting and six weeks of non-weightbearing, he continued to have pain and missed the rest of the season. Magnetic resonance imaging (MRI) showed that the fracture was failing to heal and the patient remained symptomatic. I subsequently performed posterior arthroscopic excision of the fracture fragment. The patient was able to resume sports the next season.
A 25-year-old Army specialist injured her ankle while she was deployed in Iraq. The soldier developed a posterior ankle contracture as a result of low-grade complex regional pain syndrome (CRPS). She was sent back to the United States for treatment. She was unable to walk with a plantarflexed ankle. The MRI findings suggested she had a classic posterior impingement lesion and more than likely developed arthrofibrosis. I opted for posterior ankle arthroscopy versus an open debridement to minimize trauma since she exhibited low-grade CRPS. Arthroscopy confirmed posterior ankle impingement tissue and significant cartilage damage, which wasn’t discernable on the MRI. The soldier was medically discharged due to failure to return to full duty.
Concluding Thoughts
While there is a significant learning curve with posterior ankle arthroscopy, all surgeons should be able to abort this and convert to an open procedure if necessary. Again, this is why I prefer to do these cases prone. I know there are surgeons who have no concern for flipping patients like pancakes but I would rather be prepared in the right position at the start. After 27 years in practice, I have rarely aborted a scope for an open procedure anteriorly or posteriorly, but I am always prepared.
I would encourage surgeons to start performing posterior ankle arthroscopy with cases that are primarily soft tissue in nature. As you gain confidence with this procedure, you can progress to removing os trigonums, taking down posterior tibial spurs, fixing posterolateral talar dome lesions, harvesting the flexor hallucis longus (as described by Theodoulou in his 2019 article) and the most difficult challenge, performing an arthroscopic posterior ankle fusion.1 As with any procedure, scope wisely and judiciously.
Dr. Spitalny is a staff podiatrist at the General Leonard Wood Army Community Hospital in Ft. Leonard Wood, MO, and adjunct faculty with the DePaul Podiatric Surgical Residency Program in St. Louis.
- Theodoulou M. Current perspectives on posterior ankle endoscopy/arthroscopy. Podiatry Today. 2019;32(9):18-23.
- Lui TH. Decompression of posterior ankle impingement with concomitant anterior ankle pathology by posterior ankle arthroscopy in the supine position. Arthrosc Tech. 2016;5(5):e1191–e1196.
- Mak SY, Lui TH. Endoscopic approach to posterior ankle via lateral portals. Arthrosc Tech. 2020;9(4):e559–e563.
- Yasui Y, Hannon CP, Hurley E, Kennedy JG. Posterior ankle impingement syndrome: a systematic four-stage approach. World J Orthop. 2016;7(10):657–663.
- van Dijk CN, Scholten PE, Krips R. A 2-portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy. 2000;16(8):871–876.
- van Dijk CN, van Bergen CJ. Advancements in ankle arthroscopy. J Am Acad Orthop Surg. 2008;16(11):635–646.
- Coetzee JC, Seybold JD, Moser BR, Stone RM. Management of posterior impingement in the ankle in athletes and dancers. Foot Ankle Int. 2015;36(8):988–994.
- Nault ML, Kocher MS, Micheli LJ. Os trigonum syndrome. J Am Acad Orthop Surg. 2014;22(9):545–553.
- Sofka CM. Posterior ankle impingement: clarification and confirmation of the pathoanatomy. HSS J. 2010;6(1):99–101.
- Wiegerinck JI, Vroemen JC, van Dongen TH, Sierevelt IN, Maas M, van Dijk CN. The posterior impingement view: an alternative conventional projection to detect bony posterior ankle impingement. Arthroscopy. 2014;30(10):1311–1316.
- Hayashi D, Roemer FW, D’Hooghe P, Guermazi A. Posterior ankle impingement in athletes: Pathogenesis, imaging features and differential diagnoses. Eur J Radiol. 2015;84(11):2231–2241.
- Hamilton WG, Geppert MJ, Thompson FM. Pain in the posterior aspect of the ankle in dancers. Differential diagnosis and operative treatment. J Bone Joint Surg Am. 1996;78(10):1491–1500.
- Zwiers R, Wiegerinck JI, Murawski CD, Smyth NA, Kennedy JG, van Dijk CN. Surgical treatment for posterior ankle impingement. Arthroscopy. 2013;29(7):1263–1270.
- Maquirriain J. Posterior ankle impingement syndrome. J Am Acad Orthop Surg. 2005;13(6):365–371.
- López Valerio V, Seijas R, Alvarez P, et al. Endoscopic repair of posterior ankle impingement syndrome due to os trigonum in soccer players. Foot Ankle Int. 2015;36(1):70–74.
- Dinato MC, Luques IU, Freitas Mde F, Pereira Filho MV, Ninomiya AF, Pagnano RG, Etchebehere M. Endoscopic treatment of the posterior ankle impingement syndrome on amateur and professional athletes. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1396–1401.