Essential Keys To Managing Non-Unions
 Given the challenges of non-unions, these authors offer pertinent diagnostic insights, emphasize appropriate patient selection and discuss principles to sound conservative and surgical management.
Given the challenges of non-unions, these authors offer pertinent diagnostic insights, emphasize appropriate patient selection and discuss principles to sound conservative and surgical management.
Despite substantial advances in foot and ankle surgery, non-unions remain a challenging pathology. Beyond the personal discouragement to the surgeon, there may be unexpected and life-changing ramifications for the patient, such as loss of normal function, loss of ability to work, increased financial burden, and even psychological distress from the prospect of further surgical intervention.
However, as our depth of knowledge on the nature of this condition increases, along with advances in biologics, hardware and perioperative management of high-risk patients, we are entering a new era in which the management of non-unions is possible with a multitude of preventative measures and treatments that have support in the literature.
Complicating the already intricate nature of non-unions is the absence of an accepted definition of the condition. For example, the Food and Drug Administration’s definition of non-union requires a minimum of nine months of elapsed time from the date of an injury with no clear signs of healing for three months.1 Short of open exploration and direct visual confirmation of bone healing, an op tion that is not usually reasonable in practice, there is no universally standardized way to diagnose non-unions.
tion that is not usually reasonable in practice, there is no universally standardized way to diagnose non-unions.
Therefore, most surgeons use common radiographic signs to rule out primary delay and eventual non-union. Some of these signs include the presence of a bridging callus, three of four cortices being bridged by callus formation and the resorption of fracture lines.2 Evaluation of the hardware across the proposed fusion site is also a good indicator. Hardware failure often indicates motion across the site with a lack of bony union, which places more force on the hardware, resulting in failure. Radiographic assessment is limited to the rate at which bony changes are visible in radiographs, which can take months.
A computed tomography (CT) scan is also beneficial in determining the extent of bone healing across the fusion site but even this has its limitations. The presence of hardware and artifact make it difficult to evaluate the union site adequately in CT scans. The thickness, density, size and shape of the metal hardware also affect the quality of information that one can derive from a CT scan. Fortunately, promising new research suggests that imaging techniques such as specific and sensitive bone density scans, 3D CT reconstructions and transcutaneous ultrasound could enable physicians to diagnose non-unions at a much earlier stage, justifying the use of interventional methods sooner than physicians have traditionally practiced in the past.3
Recognizin g Common Risk Factors And Ensuring Prudent Patient Selection
g Common Risk Factors And Ensuring Prudent Patient Selection
Ideally, prudent timing of treatment is essential for the best outcomes. Therefore, the best way to address this difficult complication begins in the preoperative setting. Foot and ankle surgeons encounter an incredibly diverse patient population and there are many ailments and lifestyle choices that contribute to patient risks for non-union. Understanding those risks, communicating them with the patient and preparing for them is essential.
In our preoperative planning, we should be mindful of the “diamond concept” proposed by Giannoudis and colleagues.4 They propose the notion of a four pillar standard to bone healing: the presence of osteogenic cells, an osteoconductive scaffold, mechanical stability and adequate growth factors. We strive to make sure all four of these allocations are present to ensure the most positive potential outcomes for our patients. We can infer deficiency of any one of these four factors from mitigating factors that cause increased risk for non-union, such as diabetes, obesity, age, sex, inflammatory conditions, current medications, vitamin deficiencies, thyroid abnormalities and many others.
One of the biggest patient-controlled risk factors against a favorable union is smoking. Researchers have shown that smoking increases the risk of a non-union by up to 3.2 times that of a non-smoker.5 Even former smokers have a much higher risk of non-union than patients who have never regularly smoked. In spite of substantial evidence that bone healing is at risk in smokers, note that osteogenic progenitor cells in bone marrow are still equally present and viable, allowing bone marrow aspirate to remain a viable augmentation to fusion procedures in these patients.
Aside from smoking, many other risk factors exist and are important not to overlook. For instance, research has shown that regular non-steroidal anti-inflammatory drug (NSAID) use increases the prevalence of nonunion by 2.2 times in comparison to an individual not regularly taking NSAIDs.6
Another factor to consider is the role of vitamin D in bone healing. Vitamin D is required for bone mineralization and bone quality. Multiple studies, however, have failed to show with statistical significance a direct correlation between low vitamin D levels and non-unions.7 Despite the lack of statistical significance, patients should still optimize vitamin D levels to aid in quality bone reconstruction. Tailoring a patient’s medical, social or dietary habits is an important step to avoid problems down the road. There are many opportunities for both the patient and the surgeon to address these factors, and yield the best chances of a successful union.
Lastly, non-unions secondary to infection are potentially catastrophic and exponentially more difficult to treat. Rule out this etiology with a clinical exam and advanced imaging, and address infection urgently when it is present.
Essential Perioperative Principles
The best  treatment of a non-union continues to be prevention. For us, this begins with meticulous surgical technique. After addressing the preoperative hurdles, one must employ certain perioperative principles.
treatment of a non-union continues to be prevention. For us, this begins with meticulous surgical technique. After addressing the preoperative hurdles, one must employ certain perioperative principles.
During the preparation of joint arthrodesis, one should completely remove the articular cartilage. Paying special attention to the preservation of the subchondral plate will facilitate a structurally sound and anatomically aligned fusion. We utilize subchondral drilling with a 2.0 mm drill into opposing joint surfaces to promote active bleeding at the joint, creating a segue for the migration of stem cells and bone stimulating growth factors that augment the fusion process. Additional time spent on joint preparation is time well spent.
Of course, problems with joint fusion make up just one facet of the potential etiologies for non-union. When it comes to extra-articular portions of bone or known non-union sites, one should perform debridement to bleeding bone, removing prior callus formation. Additionally, close anatomic reduction of opposing bony ends is essential for the best results. With complicated comminuted fractures, the surgeon can fill large deficits with osteoconductive preparations and use additive osteoinductive/osteogenic components when appropriate.
When Conservative Modalities Come Into Play
Sometimes, the best pre- and intraoperative methods of prevention are not enough to ensure a union. One of the most important considerations when considering invasive or non-invasive correction is that patient’s quality of life. Not all non-unions need surgical intervention.
One aspect that is just as important as patient selection is understanding when surgical treatment is not in the patient’s best interest. For example, if the patient has no loss of function, no pain and no foreseeable risk for compensatory injury, close monitoring of the patient is preferable.
Discussion of the risks and benefits of the initial procedure should always include a thorough and open dialogue about the potential for non-union. This includes thoroughly preparing the patient for the possibility, however undesired, of additional procedures. We begin to suspect non-union after 10 to 12 weeks with lagging or no signs of bone healing on radiograph. When facing this possibility, the cornerstone of adequate bone healing is mechanical stability. In the appropriate setting, the addition of biologic, physical and extracorporeal stimulation is warranted.
In our practice, patients with high risk or signs pointing to non-union will be immobile with or without a brace, depending on the ambulatory competency, neurologic status and degree of fixation in the patient’s circumstances. If possible, we often apply a bone stimulator. We have utilized internal and external devices with success in both. However, this can sometimes be a difficult financial proposition as we navigate the hurdles of specific criteria for coverage. In addition, other methods, such as variable direct ultrasound modalities, hyperbaric oxygen therapy, platelet rich plasma and various biological stimulators, have shown promising results.
What You Should Know About Surgical Management
Planning the specific technique for a revision of a non-union is best suited to the surgeon who is knowledgeable in a vast variety of options, including internal plating and external fixation, and is able to hone in on patient-specific criteria to execute the most effective outcome. In the event that surgery is inevitable, one must address key factors that may have initially contributed to the complication.
Patients should correct behaviors such as diet, nutritional status and vitamin D levels, as well as smoking and alcohol habits. Make the risks associated with non-adherence of these changes exceedingly clear.
Conversely, surgeons should also attend to the factors they can control. Ensure a stable rigid construct; augmentation of osteogenic, osteoinductive or osteoconductive properties; and establishment and maintenance of a normal anatomic alignment when possible. With the development of more anatomic contouring for internal and more “user-friendly” external devices, there are a variety of options available to choose from when determining how to obtain stable and rigid alignment. A combination of both plates and screws is often indicated to prevent any micromotion across the fusion site.
Again, it i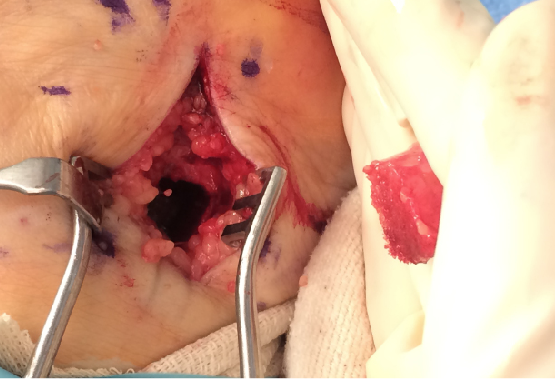 s important to emphasize the importance of joint or fusion site preparation. Any callus formation and nonviable bone needs resection. One should properly debride joint surfaces down to healthy, bleeding bone. Structural bone graft is often necessary to restore anatomic alignment. Autogenous graft remains the “gold standard” and is readily available from multiple locations. Researchers have shown that the use of allograft bone in select situations with osteobiologics provides adequate growth factors for healing.8 As we noted above, subchondral drilling is recommended in joint preparation to stimulate bone growth and healing.
s important to emphasize the importance of joint or fusion site preparation. Any callus formation and nonviable bone needs resection. One should properly debride joint surfaces down to healthy, bleeding bone. Structural bone graft is often necessary to restore anatomic alignment. Autogenous graft remains the “gold standard” and is readily available from multiple locations. Researchers have shown that the use of allograft bone in select situations with osteobiologics provides adequate growth factors for healing.8 As we noted above, subchondral drilling is recommended in joint preparation to stimulate bone growth and healing.
A Closer Look At Products That Can Help Facilitate Bone Healing
There are multiple products on the market that can aid in bone healing although the mechanism of these products can be elusive. Accordingly, we will discuss and attempt to clarify some of the most common therapies clinicians employ to facilitate bone healing.
Bone morphogenetic protein (BMP). These proteins have excellent osteoinductive potential. Specifically, BMP-2 and BMP-7 are clinically available for the treatment of non-unions. They are particularly applicable for atrophic non-union and hypertrophic non-union due to mechanical instability. Bone morphogenetic proteins are a great option in addition to allografts when autograft harvesting is contraindicated.9
Bone marrow aspirate. This solution contains hematopoietic stem cells, which are osteogenic by nature and are capable of differentiating into bone, cartilage and fibrous tissue. The success of these stem cells has been well documented for the treatment of non-unions.9 There are multiple options for application from direct aspiration to the non-union site to population of bone marrow aspirate directly to allografts before implantation.9,10
 When one combines bone marrow aspirate with an allograft, the resultant regenerative properties can approach that of an autograft. However, not all allografts are beneficial in this method. Some studies suggest that cancellous bone chips, beta-tricalcium hydroxyapatite and porous hydroxyapatite are optimal graft materials for bone marrow aspirate implantation.8 Researchers have also shown that the concentration of stem cells delivered to the non-union site is directly relevant to bone healing potential.11
When one combines bone marrow aspirate with an allograft, the resultant regenerative properties can approach that of an autograft. However, not all allografts are beneficial in this method. Some studies suggest that cancellous bone chips, beta-tricalcium hydroxyapatite and porous hydroxyapatite are optimal graft materials for bone marrow aspirate implantation.8 Researchers have also shown that the concentration of stem cells delivered to the non-union site is directly relevant to bone healing potential.11
The gold standard for stem cell extraction in the body is the anterior iliac crest, which, as foot and ankle surgeons know, is not always feasible. Harvesting from the calcaneus, distal or proximal tibia can be the province of the same surgeon who is treating the non-union, alleviating the necessity to coordinate with other doctors to harvest bone marrow. Researchers recently compared the concentration of osteoblastic progenitors in the iliac crest, tibia and calcaneus. They concluded that there is a higher concentration of stem cells in the iliac crest in comparison to the distal tibia and calcaneus, but negligible differences between the latter two. To overcome this, surgeons should obtain a higher stem cell volume of aspirate from the lower concentration locations.12-14
Teriparatide (Forteo, Lilly). This modality was originally developed for the treatment of osteoporosis. However, one may use this preparation of recombinant human parathyroid hormone off-label to treat non-unions in place of surgical intervention. The drug is a non-invasive anabolic osteoblast stimulator that increases bone production. Research on this drug for the treatment of non-unions is in the early stages. Further and deeper investigation into this drug will help provide yet another option for the podiatric physician when treating non-unions.15
In Conclusion
There are many possible approaches for patients who develop a non-union. One of the best methods of treatment is prevention.
However, if a non-union does occur, there are multiple conservative and surgical options available. Early diagnosis is very important to allow for the initiation of conservative treatment methods. Clinical, radiographic and advanced imaging are available to help in early diagnosis. Patient selection and preparation for surgery are very important to limit risk factors and optimize the possibility of fusion.
Good surgical technique to provide a stable construct and maintaining immobility are keys, not only of prevention, but also of surgical treatment of a non-union. External products are often indicated to aid in the basic principles of bone healing and one can often mix these products with bone marrow to provide an even higher probability of success.
Dr. Reeves is a Fellow of the American College of Foot and Ankle Surgeons. He is affiliated with the Orlando Foot and Ankle Clinic.
Dr. Shane is a Fellow of the American College of Foot and Ankle Surgeons. She is affiliated with the Orlando Foot and Ankle Clinic.
Dr. Payne is a second-year surgical resident with the Florida Hospital East Orlando Podiatric Surgical Residency Program.
Dr. Cameron is a second-year surgical resident with the Florida Hospital East Orlando Podiatric Surgical Residency Program.
References
- U.S. Food and Drug Administration. Guidance document for the preparation of investigational device exemptions and pre-market approval applications for bone growth stimulator devices, 1998. Available at www.fda.gov/ohrms/dockets/98fr/98d0238.pdf .
- Hak DJ, Fitzpatrick D, Bishop JA, et al. Delayed union and nonunions: Epidemiology, clinical issues, and financial aspects. Injury. 2014; 45(Suppl2):S3-7.
- Calisir C, Fayad LM, Carrino JA, Fishman EK. Recognition, assessment, and treatment of non-union after surgical fixation of fractures: emphasis on 3D CT. Jpn J Radiol. 2012; 30(1):1-9.
- Giannoudis PV, Einhorn TA, Marsh D. Fracture healing: the diamond concept. Injury. 2007; 38(Suppl4):S3-6.
- Patel R, Wilson R, Patel P, Palmer R. The effect of smoking on bone healing: a systematic review. J Bone Joint Res. 2013; 2(6):102-111.
- Jeffcoach D, Sams V, Enderson B, et al. Nonsteroidal anti-inflammatory drugs’ impact on nonunion and infection rates in long-bone fractures. J Trauma Acute Care Surg. 2014; 76(3):779-783.
- Gorter EA, Hamdy NA, Appelman-Dijkstra NM, Schipper IB. The role of vitamin D in human fracture healing: a systematic review of the literature. Bone. 2014; 64:288-297.
- Murphy MB, Suzuki RK, Sand TT, Chaput CD, Gregory CA. Short term culture of human mesenchymal stem cells with commercial osteoconductive carriers provides unique insights into biocompatibility. J Clin Med. 2013; 2(3):49-66.
- Schmidmaier G, Schwabe P, Wildemann B, Haas N. Use of bone morphogenetic proteins for treatment of non-unions and future perspectives. Injury. 2007; 38(Suppl4):S35-41.
- Kassem MS. Percutaneous autogenous bone marrow injection for delayed union or non union of fractures after internal fixation. Acta Orthop Belg. 2013;79(6):711-7.
- Hernigou P, Poignard A, Beaujean F, Rouard H. Treatment of non-unions with percutaneus autologous bone marrow grafting: Influence of the number and concentration of progenitor cells. J Bone Joint Surg Am. 2005; 87(7):1430-7.
- Mahendra A, Maclean A. Available biological treatments for complex non-unions. Injury. 2007; 38(Suppl4):7-12.
- Pountos I, Corscadden D, Emery P, Giannoudis PV. Mesenchymal stem cell tissue engineering: Techniques for isolation, expansion and application. Injury. 2007; 38(Suppl4):23-33.
- Hyer C, Berlet GC, Bussewitz BW, et al. Quantitative assesment of the yield of osteoblastic connective tissue progenitors in bone marrow aspirate from the iliac crest, tibia, and calcaneus. J Bone Joint Surg. 2013; 95(14):1312-16.
- Pietrogrande L, Raimondo E. Teriparatide in the treatment of non-unions: Scientific and clinical evidences. Injury. 2013; 44(Suppl1):S54-57.











