Emerging Trends With Orthobiologics In Podiatric Surgery
Bone loss is a challenging aspect of foot and ankle reconstruction, but new developments in grafting technologies are opening doors for improved pathways. Accordingly, the author discusses the promise of emerging options along with indications, precautions and evidence from the literature.
We all want to do what is right the first time without complications and with high patient satisfaction. This goes without saying in any realm of orthopedics, let alone any surgical specialty. As surgeons, we aim high yet there are certain clinical circumstances that continue to challenge us daily. In the foot and ankle community, it is non-unions.
A non-union is a chronic condition characterized by pain and functional disability. Typically, a foot and ankle fracture heals without complication 90 to 95 percent of the time.1 The U.S. Food and Drug Administration (FDA) defines a non-union as a fracture that is at least nine months old and has not shown any signs of healing for three consecutive months.1 Foot and ankle fractures and fusions that go on to to non-unions are that small subset of cases that cannot overturn the stunted local biologic process and challenging mechanics of the bony injury repair cycle. Despite being uncommon, non-unions are often difficult cases to overcome and an uphill battle usually ensues. The current trend is to avoid catastrophe before it occurs by encouraging use of enhanced biologic therapies while maintaining sound mechanical fixation principles.2
One can simply break down the thought process into the perioperative phases: preoperative medical optimization, intraoperative orthobiologic strategies and postoperative patient rehabilitation.
Some questions come to mind when one starts discussing the goals of intraoperative treatment for a complicated foot and ankle non-union, whether it is a first metatarsophalangeal joint fusion revision or a tibiotalocalcaneal joint fusion in a patient with semi-controlled diabetes. What are the needs of the recipient site? Is structural support required? Is there a large void that one needs to fill? What is the size or volume requirement? Is this a staged approach? Is it infected?
Key Aspects Of Appropriate Patient Selection And Preoperative Planning
While preoperative medical optimization is beyond the scope of this discussion, I would like to quickly touch base on my preferred protocol for any complicated non-union repair. First and foremost, one needs to rule out infection. There are various protocols for total joint arthroplasty or periprosthetic joint infection, and some are specific to foot and ankle arthroplasty.3-6 Most of the literature follows the guidelines of our hip and knee colleagues. Basic understanding of infection workup is paramount and includes evaluation of the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) as well as a basic complete blood count (CBC). Typically, one will also draw blood cultures.
If the periprosthetic joint infection is more acute (less than four weeks post-op), then the surgeon will typically perform a formal incision and drainage with polyethylene exchange. If the infection occurs more than four weeks after the index procedure, then the concern is for deep infection and a formal explantation with antibiotic spacer becomes necessary with six weeks of suppression antibiotics until lab results trend down.
If bone stock is available, one may perform a formal second stage procedure with revisional total ankle arthroplasty versus an arthrodesis. The general thought process for these complex cases also applies to any joint replacement and warrants consideration for any foot and ankle revisional fusion, especially in cases involving implanted hardware.
After ruling out infection and/or removing the hardware, one can assess the patient for other pertinent risk factors. Risk factors that may elevate the risk of non-union include but are not limited to: diabetes, tobacco use, neuropathy, history of non-union at other sites, poor local vascularity and obesity. Thevendran and colleagues noted the highest perceived risk factors for non-union are smoking two packs of cigarettes per day, lack of fusion site stability, poor local vascularity and osteoporosis.7 Each of these cases are complex and deserves attention above and beyond the typical fusion or fracture revision. Multiple authors have shared insights about medical optimization prior to revisional fusion or open reduction and internal fixation.8-10
Now let us now turn our attention to intraoperative orthobiologic strategies.
Assessing The Roles Of New Orthobiologics In Foot And Ankle Surgery
The market of orthobiologics is constantly changing and becoming saturated. However, innovation is driving market values as technology improves, which ultimately helps our patients heal. Again, the idea is to prevent a non-union from occurring in the first place. With this in mind, I would encourage liberal use of these technologies albeit in as cost-effective manner as possible. One can divide these modalities into allograft and autograft categories. Instead of debating which modalities are better, I seek to highlight the instances when one is more beneficial than the other.
Allografts typically include recombinant human bone morphogenetic protein, demineralized bone matrix, bioactive glass, recombinant human platelet-derived growth factor, ceramic and non-ceramic structural allografts, and various combinations of custom and semi-custom metallic cages and wedges. When it comes to podiatric surgery, autografts typically include corticocancellous iliac crest bone graft, tibial or calcaneal cancellous graft, bone marrow aspirate and platelet-rich plasma. We can further break this down into structural versus biologic need. For instance, if there is a significant bone void, this may be a great opportunity to insert a custom metallic wedge to reduce the possibility of subsidence.
With this in mind, let us consider the various emerging orthobiologics that I view as a priority when it comes to managing non-unions in foot and ankle surgery.
A Closer Look At The Use Of Augment For Complex Ankle And Hindfoot Fusions
A combination of recombinant human platelet-derived growth factor (rhPDGF-BB) and beta-tricalcium phosphate (B-TCP), Augment® Bone Graft (Wright Medical) is increasingly popular for complex ankle and hindfoot fusions. The product is indicated for ankle and hindfoot arthrodesis procedures, and is a chemotactic agent for mesenchymal stem cells. Also, rhPDGF-BB is the most potent mitogen for mesenchymal stem cells. Platelet-derived growth factor also upregulates endothelial growth factor, which promotes angiogenesis at the fusion site. These various factors help proliferate the bone healing cascade and also stimulate the remodeling phase to help form mature, viable bone.
An injectable version of the Augment Bone Graft received FDA approval in the summer of 2018.11 Containing a flowable type I bovine collagen, the injectable form of Augment Bone Graft is user-friendly and allows the surgeon to spread the product into the far reaches of the joint site.
In a prospective, randomized study comparing autograft versus injectable Augment for hindfoot and ankle fusions, Daniels and colleagues found no significant difference in outcomes between the treatment groups on computed tomography (CT) scans at a 36-week follow-up.12 The researchers also noted no significant difference in the mean time to fusion. At a 52-week follow-up, there were also no significant differences between these treatment groups in clinical outcome measures including the Foot Function Index, weightbearing pain and the American Orthopedics Foot and Ankle Society (AOFAS) Ankle-Hindfoot Scale.
This study demonstrates that a synthetic graft can be non-inferior and safe in comparison to autograft.12 This study by Daniels and coworkers, among other studies, also highlights the importance of CT scans at regular intervals during the postoperative course for some of these advanced fusions.12,13 Multiple researchers have also confirmed clinical success of a fusion when approximately 40 to 50 percent of the joint is a solid fusion mass.14-16
With this in mind, I will typically order a CT scan at the four-month mark postoperatively to assess the fusion mass. In my operating room, I utilize the injectable Augment in combination with bone marrow aspirate to assist in patients with significant comorbidities and in those of advanced age. I typically do not propose the use of this product for a primary fusion due to associated health-care costs, especially in a healthier patient.
Can Recombinant Bone Morphogenetic Protein Have An Impact?
Another emerging osteoinductive biologic is the recombinant human bone morphogenetic protein-2 (rhBMP-2) modality Infuse™ Bone Graft (Medtronic). While this product has been the subject of level-V systematic reviews over the past several years and has promising capabilities, the Infuse Bone Graft is only indicated for acute open tibial shaft fractures stabilized with intramedullary nail fixation and various types of spinal fusions.17,18 With that being said, any use of the Infuse Bone Graft for foot or ankle fusion is off-label, and one should discuss the risks and alternatives with the patient in detail.
The overall role of bone morphogenetic protein and its mechanism of action are well understood in the healing of fractures and production of new bone.19
The ability of the Infuse Bone Graft to form bone depends on the concentration of the BMP within the absorbable collagen sponge carrier. I typically only reserve this product for specific Charcot neuroarthropathy cases in combination with bone marrow aspirate and structural allograft. I have a discussion with the patient in terms of the off-label use and will use the smallest amount of the product.
What About Alternatives To Femoral Head Allograft?
I would also like to discuss the use of metallic wedges and grafts, including cages, premade wedges and cobalt chromium custom implants. There are certainly cases that do well with structural bone allograft. For instance, there are studies showing success with femoral head allograft use in Charcot tibiotalar calcaneal fusions.20 Femoral head allograft is also a viable option for failed total ankle arthroplasty.21 In certain circumstances, this may be the only option based on cost and availability.
Again, femoral head was the standard for large segmental defects or bone voids but, over the past several years, the landscape has changed. With advances in three-dimensional (3D) printing and additive technologies, we are now seeing success stories for a subset of challenging cases that would have originally proceeded to a proximal amputation. The utility of these technologies spans not only the foot and ankle, but oral maxillofacial care and orthopedic oncology as well.
Why not use a structural femoral head allograft? One of the primary reasons is loss of structural integrity over time and lack of osteoinductive capabilities that can lead to devastating non-unions. This is where I find titanium femoral head or custom lattices very helpful in reducing subsidence. I have also been able to pack in autograft or high-density allograft to create the best of both worlds. This is a controversial topic and each case requires its own approval from a hospital standpoint.
There are several manufacturers capable of creating custom and semi-custom foot and ankle bone void lattices. These companies include Additive Orthopedics, 4WEB Medical and Restor3d. These wedges and cages are able to withstand large compressive forces and mimic osseous ingrowth.22 In regard to tibiotalar calcaneal fusions, it is frequently necessary to utilize a intercalary retrograde intramedullary nail for compression and stabilization. I typically will reach for a high volume of autograft in these cases from the ipsilateral proximal tibia.
On the subject of custom implants, I have had success employing custom cobalt-chromium articular foot and ankle components in a case involving a total talar replacement and ankle arthroplasty procedure.23
For the purposes of this article, I did not delve into specific details on the nuances of less popular ceramics, demineralized bone matrix and autografts. There are many articles and resources for how-to and technique tips for procurement of autograft.24 I base my decision point and preference for cancellous autograft on volume need: one to five cc for the calcaneus; five to 10 cc for the distal tibia; and 10 cc or greater for the proximal tibia.
Case Study: When A 72-Year-Old Female Presents With A Post-Traumatic Subtalar Joint Dislocation And Arthritis
In order to prepare for intraoperative success, it is important to have the appropriate hardware and team available for each of these cases.
I would like to present a case of a 72-year-old female with osteoporosis, a history of chemotherapy and previous tobacco use over 10 years ago. She previously sustained a closed trimalleolar ankle fracture, which I reduced and fixated appropriately with plates and screws. The patient diligently followed the postoperative course despite being a caretaker for her husband and the fracture had healed a year prior to her current presentation. However, she is now presenting with continued pain and disability.
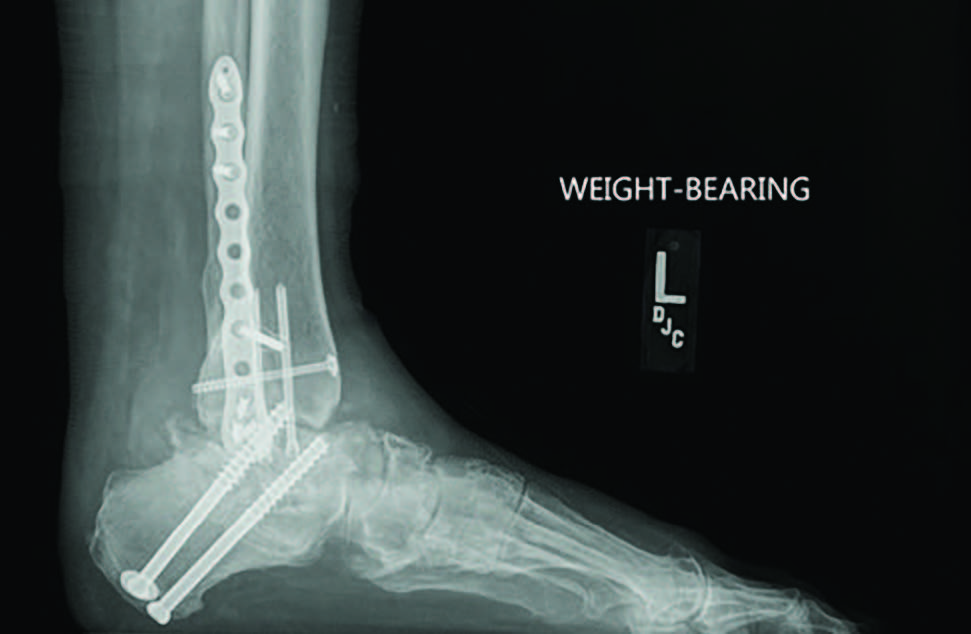
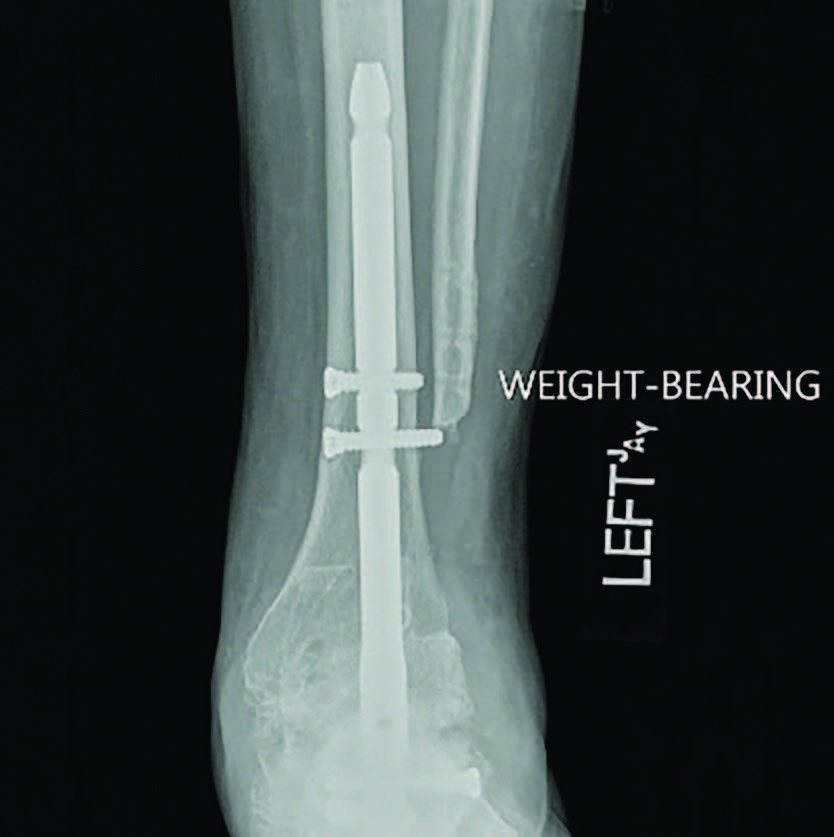
Radiographs demonstrated a subtalar joint dislocation with advanced degenerative changes (see first two images above). As we prepared for a subtalar joint fusion, we emphasized medical optimization of her vitamin D levels and made sure to rule out any metabolic weaknesses that would alter our techniques in the operating room. In my experience, it is best to perform these complex cases at facilities that can provide comprehensive patient care and possible admission if necessary.
For this patient, I ultimately performed a subtalar joint fusion with distal tibial autograft. She subsequently went on to develop a symptomatic non-union at six months postoperatively and collapse of her talus (see third image above). She again had medical optimization and we planned for a femoral head allograft reconstruction with Augment bone graft and intramedullary nail fixation. The patient went on to clinical success and there was demonstrated healing on a CT scan at four months post-op. She is now weightbearing in a shoe at two years post-op (see fourth and fifth images above).
Final Thoughts
Orthobiologics is an ever-changing field. We will continue to adapt and adopt new technologies that may improve our intraoperative strategies and solutions. Non-unions continue to play a role in all foot and ankle clinics, and we should take heed to the complexity each presents. Utilizing advanced techniques and orthobiologics when necessary can assist to optimize outcomes.
Dr. McAlister is a fellowship-trained foot and ankle surgeon, and founder of the Ankle Arthritis Center and the Phoenix Foot and Ankle Institute. He is also a Fellow of the American College of Foot and Ankle Surgeons. He can be reached at jeff.mcalister@ phoenixfai.com.
1. Calori GM, Mazza EL, Mazzola S, et al. Non-unions. Clin Cases Miner Bone Metab. 2017;14(2):186-188.
2. Yeoh JC, Taylor BA. Osseous healing in foot and ankle surgery with autograft, allograft, and other orthobiologics. Orthop Clin North Am. 2017;48(3):359–369.
3. Walley KC, Arena CB, Juliano PJ, Aynardi MC. Diagnostic criteria and treatment of acute and chronic periprosthetic joint infection of total ankle arthroplasty. Foot Ankle Orthop. 2019;4(2). Available at: https://journals.sagepub.com/ doi/full/10.1177/2473011419841000 . Accessed May 9, 2020.
4. Alrashidi Y, Galhoum AE, Wiewiorski M, et al. How to diagnose and treat infection in total ankle arthroplasty. Foot Ankle Clin. 2017;22(2):405–423.
5. Patton D, Kiewiet N, Brage M. Infected total ankle arthroplasty: risk factors and treatment options. Foot Ankle Int. 2015;36(6):626–634.
6. Shibuya N, Humphers JM, Fluhman BL, Jupiter DC. Factors associated with nonunion, delayed union, and malunion in foot and ankle surgery in diabetic patients. J Foot Ankle Surg. 2013;52(2):207–211.
7. Thevendran G, Shah K, Pinney SJ, Younger AS. Perceived risk factors for nonunion following foot and ankle arthrodesis. J Orthop Surg (Hong Kong). 2017;25(1):2309499017692703.
8. Moore KR, Howell MA, Saltrick KR, Catanzariti AR. Risk factors associated with nonunion after elective foot and ankle reconstruction: a case-control study. J Foot Ankle Surg. 2017;56(3):457–462.
9. Thevendran G, Wang C, Pinney SJ, Penner MJ, Wing KJ, Younger AS. Nonunion risk assessment in foot and ankle surgery: proposing a predictive risk assessment model. Foot Ankle Int. 2015;36(8):901–907.
10. DeFontes K 3rd, Smith JT. Surgical considerations for vitamin D deficiency in foot and ankle surgery. Orthop Clin North Am. 2019;50(2):259–267.
11. Augment injectable – P100006/S005. U.S. Food and Drug Administration. Available at: https://www.fda.gov/medical-devices/recently-approved-devices/augmentr-injectable-p100006s005 . Published June 12, 2018. Accessed May 12, 2020.
12. Daniels TR, Younger AS, Penner MJ, et al. Prospective randomized controlled trial of hindfoot and ankle fusions treated with rhPDGF-BB in combination with a ß-TCP-collagen matrix. Foot Ankle Int. 2015;36(7):739–748.
13. DiGiovanni CW, Lin SS, Daniels TR, et al. The importance of sufficient graft material in achieving foot or ankle fusion. J Bone Joint Surg Am. 2016;98(15):1260–1267.
14. Krause F, Younger AS, Baumhauer JF, et al. Clinical outcomes of nonunions of hindfoot and ankle fusions. J Bone Joint Surg Am. 2016;98(23):2006–2016.
15. Coughlin MJ, Grimes JS, Traughber PD, Jones CP. Comparison of radiographs and CT scans in the prospective evaluation of the fusion of hindfoot arthrodesis. Foot Ankle Int. 2006;27(10):780–787.
16. Glazebrook M, Beasley W, Daniels T, et al. Establishing the relationship between clinical outcome and extent of osseous bridging between computed tomography assessment in isolated hindfoot and ankle fusions. Foot Ankle Int. 2013;34(12):1612–1618.
17. Dai J, LiL, Jiang C, Wang C, Chen H, Chai Y. Bone morphogenic protein for the healing of tibial fracture; a meta-analysis of randomized controlled trials. PLoS One. 2015. Available at: https://journals.plos.org/plosone/ article?id=10.1371/journal.pone.0141670. Accessed May 15, 2020.
18. Indications, safety, and warnings: Infuse Bone Graft: spine and trauma. Medtronic. Available at: https://www.medtronic.com/us-en/ healthcare-professionals/products/spinal-orthopaedic/bone-grafting/infuse-bone-graft/ indications-safety-warnings.html . Accessed May 12, 2020.
19. Wozney JM, Rosen V. Bone morphogenetic protein and bone morphogenetic protein gene family in bone formation and repair. Clin Orthop Relat Res. 1998;(346):26–37.
20. Bussewitz B, DeVries JG, Dujela M, McAlister JE, Hyer CF, Berlet GC. Retrograde intramedullary nail with femoral head allograft for large deficit tibiotalocalcaneal arthrodesis. Foot Ankle Int. 2014;35(7):706–711.
21. Halverson AL, Goss DA Jr, Berlet GC. Ankle arthrodesis with structural grafts can work for the salvage of failed total ankle arthroplasty. Foot Ankle Spec. 2020;13(2):132-137.
22. Egan PF, Gonella VC, Engensperger M, Ferguson SJ, Shea K. Computationally designed lattices with tuned properties for tissue engineering using 3D printing. PLoS One. 2017;12(8):e0182902.
23. McAlister JE. A closer look at a total talar replacement and ankle arthroplasty. Podiatry Today. 2020;33(3). Available at: https://www. podiatrytoday.com/index.php/closer-look-total-talar-replacement-and-ankle-arthroplasty . Published March 30, 2020. Accessed May 9, 2020.
24. Miller CP, Chiodo CP. Autologous bone graft in foot and ankle surgery. Foot Ankle Clin. 2016;21(4):825-837.