Emerging Insights On The Trephine Arthrodesis
Trephine arthrodesis can be an effective procedure for tarsometatarsal joint fusions and other indications. Sharing pertinent insights from his experience, this author discusses the procedure’s numerous advantages, ranging from ease of use to reduced risk of non-unions, and offers a compelling case study.
 Trephine arthrodesis in foot surgery is nothing new but for some reason, foot surgeons rarely consider it. Surgeons can utilize trephine arthrodesis for many of the joints in the foot, including but not limited to the subtalar joint, tarsometatarsal joints, intercuneiform joints and the naviculocuneiform joint. In my experience, arthrodesis of the second and third tarsometatarsal joints is the primary procedure for which I will choose a trephine arthrodesis technique. While the main focus of this article will be the use of the trephine arthrodesis for tarsometatarsal joint arthrodesis, the concepts and techniques with the trephine arthrodesis are similar regardless of the joint(s) you are fusing.
Trephine arthrodesis in foot surgery is nothing new but for some reason, foot surgeons rarely consider it. Surgeons can utilize trephine arthrodesis for many of the joints in the foot, including but not limited to the subtalar joint, tarsometatarsal joints, intercuneiform joints and the naviculocuneiform joint. In my experience, arthrodesis of the second and third tarsometatarsal joints is the primary procedure for which I will choose a trephine arthrodesis technique. While the main focus of this article will be the use of the trephine arthrodesis for tarsometatarsal joint arthrodesis, the concepts and techniques with the trephine arthrodesis are similar regardless of the joint(s) you are fusing.
There are distinct advantages to a trephine arthrodesis. These advantages include:
• quicker fusion time with decreased incidence of non-union;
• less likelihood of shortening the bone segments;
• less instrumentation and time:
• avoidance of sagittal plane deformity of the metatarsal in a tarsometatarsal joint fusion; and
• the ability to easily fuse intercuneiform and/or intermetatarsal joints if necessary.
When performing an arthrodesis in which manipulation of position is necessary for correction, traditional joint preparation and fusion are necessary. Consider naviculocuneiform joint arthrodesis as an example. A trephine arthrodesis would be a good choice in the case of arthritis without faulting (sag) in the joint. However, in the adult-acquired flatfoot deformity, a traditional arthrodesis is preferable for fusing the naviculocuneiform joint. Flat joints without deformity are typically amenable to trephine arthrodesis but the procedure is not typically recommended for ball and socket joints and triplanar joints.
What Advantages Does The Trephine Arthrodesis Offer?
Let us take a closer look at the advantages of trephine arthrodesis. As I noted previously, while tarsometatarsal fusion is by far the most common indication for the trephine arthrodesis in my experience, this procedure is not limited to tarsometatarsal fusion.
 Quicker fusion time/fewer non-unions. We know that the best healing potential in long bones will be in the metaphysis. The subchondral bone plate often remains intact for stability in fusions. Healing time increases when bone has to bridge the subchondral bone plate. When there is arthrosis of the tarsometatarsal joints, for example, there is typically significant sclerosis of this bone. With a trephine arthrodesis, one removes the entire subchondral bone and leaves healthy metaphyseal bone for autogenous bone filling of the defect. This should allow for quicker incorporation of bone and no need for bridging of bone across sclerotic bone plates.
Quicker fusion time/fewer non-unions. We know that the best healing potential in long bones will be in the metaphysis. The subchondral bone plate often remains intact for stability in fusions. Healing time increases when bone has to bridge the subchondral bone plate. When there is arthrosis of the tarsometatarsal joints, for example, there is typically significant sclerosis of this bone. With a trephine arthrodesis, one removes the entire subchondral bone and leaves healthy metaphyseal bone for autogenous bone filling of the defect. This should allow for quicker incorporation of bone and no need for bridging of bone across sclerotic bone plates.
Avoid shortening of the ray. When surgeons perform a traditional end-to-end arthrodesis of the tarsometatarsal joint, they typically remove cartilage and subchondral bone, which can leave a 5 mm gap between the bones. If one takes a sagittal saw and passes it up and down the joint, there is little chance of removing the subchondral bone with that technique. There is also the potential for thermal necrosis. I have found this can lead to prolonged healing times and more non-unions.
Saving time with less instrumentation. The most common method of joint preparation would be to expose the joint with a mini-joint distractor and use a hand curette, rongeur, rotary burr and/or a saw to prepare the joint. Extensive soft tissue/ligament release is necessary to open the joint enough to get exposure, which tends to destabilize the joint. Without a joint distractor, one cannot really appreciate the plantar aspect of the joint and will leave cartilage or subchondral bone. This will lead to a delay in healing. It wastes time to handle so many instruments. Additionally, one is typically fiddling with a joint distractor and working around that. By the time one drills a couple of K-wires, puts on the distractor and opens the joint, the trephine would have already cored the recipient site.
 Avoidance of sagittal plane deformity. As I discussed earlier, the plantar aspect of the fusion is the most difficult area to prepare and surgeons often do not adequately address it. When this happens, dorsiflexion of the metatarsal will occur when the two ends of bone come together. Moreover, if there is a significant gap between the bones after saw resection of subchondral bone plates, a sagittal plane deformity is more likely to occur as one is trying to counteract soft tissue constraints to make a tight fit.
Avoidance of sagittal plane deformity. As I discussed earlier, the plantar aspect of the fusion is the most difficult area to prepare and surgeons often do not adequately address it. When this happens, dorsiflexion of the metatarsal will occur when the two ends of bone come together. Moreover, if there is a significant gap between the bones after saw resection of subchondral bone plates, a sagittal plane deformity is more likely to occur as one is trying to counteract soft tissue constraints to make a tight fit.
Other Considerations With The Trephine Arthrodesis
Another benefit of the trephine arthrodesis is that the procedure can not only encompass the tarsometatarsal joints for fusion but it can also enable you to orient the plug to catch an intermetatarsal joint or even an intercuneiform joint if you suspect pain may be coming from those sites.
I have found the high arch and curved foot type (metatarsus adductus) is one of the most challenging foot conditions to treat. We know this foot type tends to stress the lateral part of the foot and as a result, premature, non-traumatic arthrosis occurs in the second and third tarsometatarsal joints.1 In addition to the arthrosis, there is typically a large exostosis in the area, causing pain to the dorsal foot when the patient wears shoes.
From a non-surgical standpoint, for those with a high arch and cavus foot type, I recommend oral and/or topical anti-inflammatory medication, occasional cortisone injections in a periarticular fashion to the tarsometatarsal joints, alternating shoe lace patterns, and using a valgus orthotic device to prevent lateral foot overload. For many patients, these conservative treatments are not adequate to resolve pain and surgery is indicated.
 For the most part, surgery will involve an exostectomy with or without a tarsometatarsal joint arthrodesis of the affected joints. It is important to try to elucidate the origin of the patient’s pain. The exostosis will typically cause nerve irritation to the dorsal foot. When the primary symptom is from arthritis, one would have morning stiffness with post-static dyskinesia. Certainly, the patient can have both nerve irritation and arthritis. Diagnostic anesthetic injections can be very helpful in differentiating the two conditions.
For the most part, surgery will involve an exostectomy with or without a tarsometatarsal joint arthrodesis of the affected joints. It is important to try to elucidate the origin of the patient’s pain. The exostosis will typically cause nerve irritation to the dorsal foot. When the primary symptom is from arthritis, one would have morning stiffness with post-static dyskinesia. Certainly, the patient can have both nerve irritation and arthritis. Diagnostic anesthetic injections can be very helpful in differentiating the two conditions.
When there is arthritis pain, then an arthrodesis is necessary in addition to the exostectomy to resolve pain. A computed tomography (CT) scan or magnetic resonance image (MRI) can be helpful to ascertain the amount of arthrosis. The CT will give you the best picture of the amount of damage to the joints whereas the MRI will determine how much bone marrow edema and inflammation are associated with each joint.
Case Study: Performing A Trephine Arthrodesis To Address Dorsal Midfoot Pain From Severe Tarsometatarsal Joint Arthritis
For an example of the trephine arthrodesis technique, consider the following case report.
A 66-year-old female presented to my office with dorsal midfoot pain. She had prior foot surgery, which included a dorsal tarsometatarsal joint exostectomy and a bunionectomy. Her X-rays were remarkable for second and third tarsometatarsal joint arthritis, and a CT scan confirmed severe arthrosis.
 Upon examining the patient, she had some residual abduction of the great toe with some undermining of the second toe. Pain was present with palpation of the second and third tarsometatarsal joints, and with sagittal plane motion of the second and third metatarsals. In addition to arthritis of the tarsometatarsal joints, X-rays revealed a short first ray and residual exostosis in the midfoot.
Upon examining the patient, she had some residual abduction of the great toe with some undermining of the second toe. Pain was present with palpation of the second and third tarsometatarsal joints, and with sagittal plane motion of the second and third metatarsals. In addition to arthritis of the tarsometatarsal joints, X-rays revealed a short first ray and residual exostosis in the midfoot.
Therefore, my surgical plan was to perform a modified McBride bunionectomy with an Akin osteotomy to help straighten the big toe without any more shortening of the first ray as well as a trephine arthrodesis of the second and third tarsometatarsal joints with autogenous bone graft from the ipsilateral heel.
Focusing on the trephine arthrodesis, I made a linear incision over the second and third tarsometatarsal joints. One should carry dissection down through the soft tissues with care to avoid the artery and nerve in the area. Reflect the capsule and periosteum from the joint, and use a Freer elevator to find the joint.
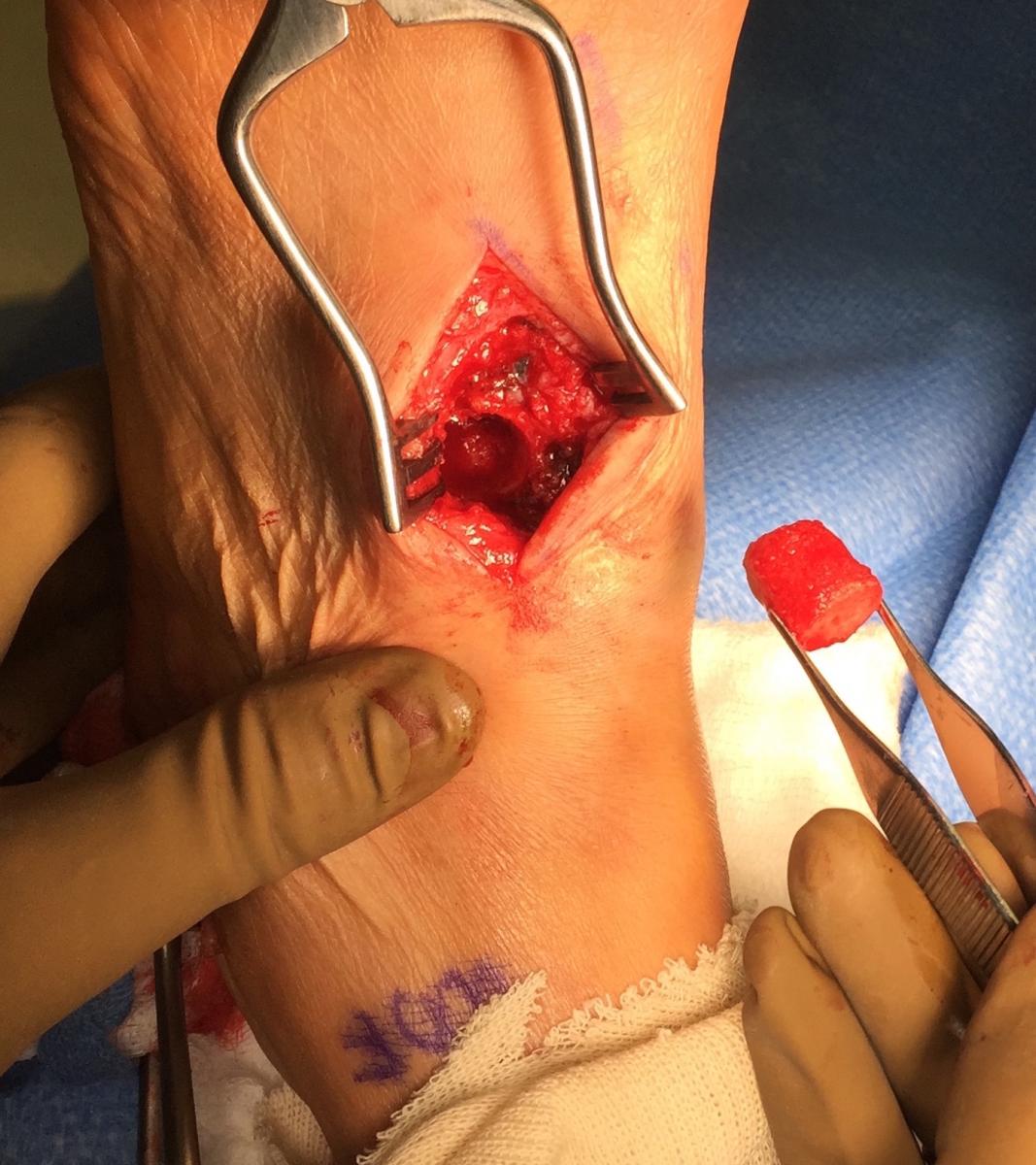
Using a 10 mm trephine, I proceeded to remove three-quarters of the joint, leaving a plantar shelf of bone to serve as the floor. Generally, 20 mm in depth is adequate. Ryan and colleagues reported the average depth of the second and third tarsometatarsal joints were 26.9 mm and 23.6 mm respectively.2 Typically, one discards the removed bone plug.
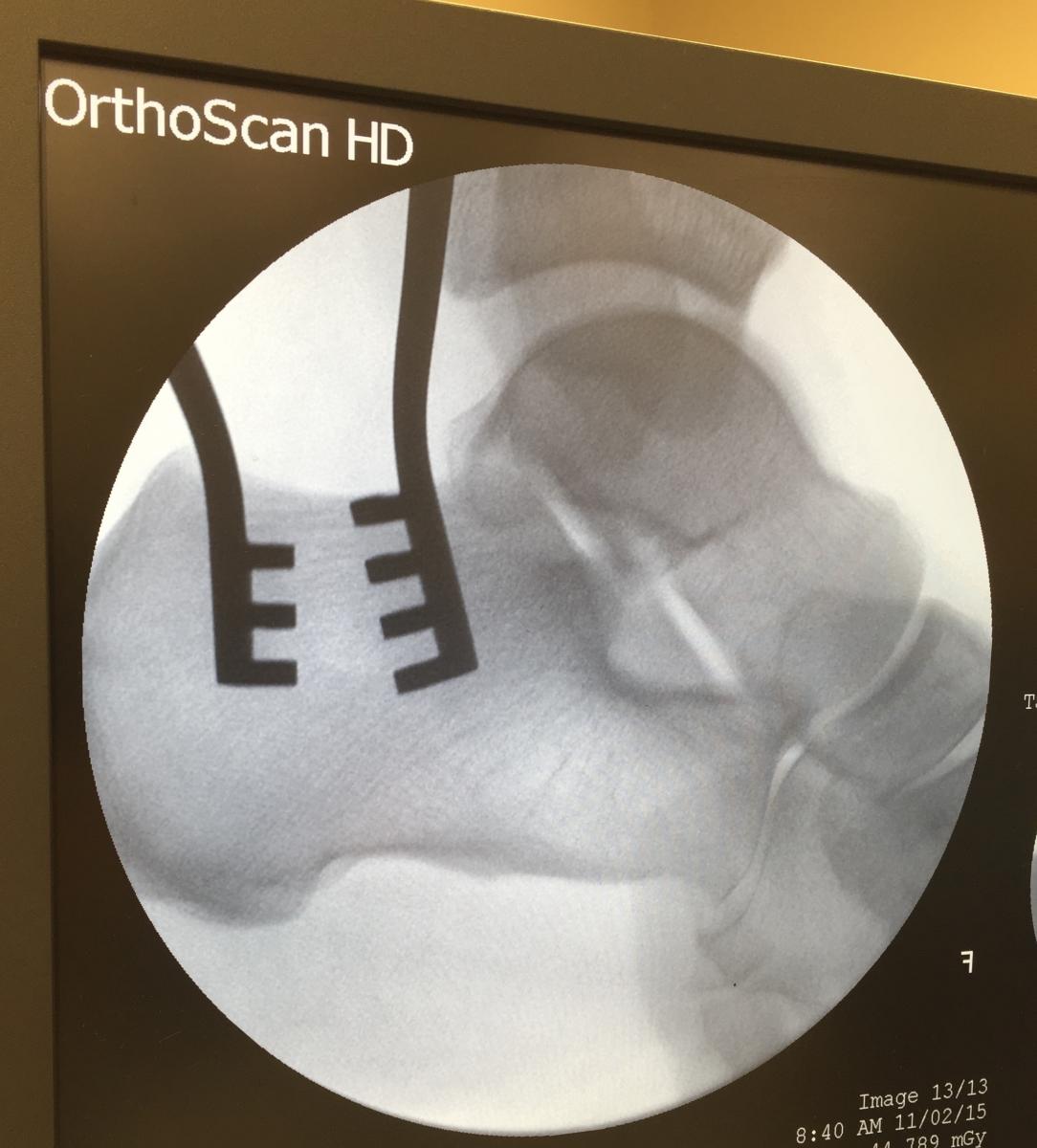
Then the surgeon can harvest the autogenous bone from the ipsilateral heel. Make an oblique incision over the lateral heel, similar to a Dwyer incision. Carry dissection down to the periosteum of the heel, which one then reflects with a Freer elevator. A Weitlaner retractor aids in retraction and also helps confirm where the plug will originate. A fluoroscopy image with the retractor in place allows you to cut the plug between the teeth of the retractor and you will always take the plug from the precise area you want. Use a 12 mm trephine so there will be a tight fit of the graft. Then tamp the autogenous bone into the recipient site and make it flush to the surrounding bone.
 For the third joint, perform the same process. Since you are only taking about 20 mm of bone, you can get another plug from the same site where you obtained the first plug. After grafts are in place, I will typically place a staple over the graft to prevent any dorsal migration of the graft. It is perfectly acceptable not to use fixation if you feel the graft had a very tight fit. Typically, you cannot press fit the graft and need to tamp it in with a mallet. Backfill allograft bone to the calcaneus. Cancellous chips work well and I will use the plunger/tamp from the trephine to really pack the bone in the deficit. Close tissues in layers and apply a dressing with a below-knee posterior splint.
For the third joint, perform the same process. Since you are only taking about 20 mm of bone, you can get another plug from the same site where you obtained the first plug. After grafts are in place, I will typically place a staple over the graft to prevent any dorsal migration of the graft. It is perfectly acceptable not to use fixation if you feel the graft had a very tight fit. Typically, you cannot press fit the graft and need to tamp it in with a mallet. Backfill allograft bone to the calcaneus. Cancellous chips work well and I will use the plunger/tamp from the trephine to really pack the bone in the deficit. Close tissues in layers and apply a dressing with a below-knee posterior splint.
The postoperative protocol includes X-rays at week one. I will usually use a fracture boot as a removable cast for six to eight weeks of non-weightbearing until X-rays confirm healing. I then recommend gradual protected ambulation in the fracture boot for two to four weeks. Once they ambulate in the fracture boot without pain, patients have a gradual return to shoes.
In Summary
A trephine arthrodesis can be another technique that works very well for tarsometatarsal joints. While surgeons can certainly use the trephine arthrodesis for other fusions in the foot, tarsometatarsal joint fusion seems to be the most common scenario in which I employ this technique. Advantages of the trephine arthrodesis include simplicity for joint preparation; avoidance of shortening or angulation deformities of the metatarsal; rapid incorporation, especially when using an autograft; and generally quicker preparation and fixation than a traditional end-to-end arthrodesis.
Here are some simple pearls to remember.
1. Trephine arthrodesis is ideal when there is no need for adjustment of the position of the bones (i.e. shortening, angulation, etc.).
2. Make sure you use a 2 mm larger trephine for your bone graft procurement to allow for a tight fit in the recipient site.
3. Leave a plantar shelf at the arthrodesis site to allow for a floor of the graft as well as maintaining ligamentous stability.
4. A fluoroscopic image with placement of a Weitlaner retractor in the heel will ensure you obtain your graft in the desired location.
5. Always consider this technique for a non-union repair as there is typically a lot of fibrotic bone that needs debridement and this will prevent shortening of the bone segments and/or the need of a structural graft to fill the defect.
Dr. Fishco is board-certified in foot surgery and reconstructive rearfoot and ankle surgery by the American Board of Podiatric Surgery. He is a Fellow of the American College of Foot and Ankle Surgeons, and a faculty member of the Podiatry Institute. Dr. Fishco is in private practice in Phoenix.
References
- Fishco WD, Ellis MB, Cornwall MW. Influence of a metatarsus adductus foot type on plantar pressures during walking in adults using a pedobarograph. J Foot Ankle Surg. 2015; 54(3):449-453.
- Ryan JD, Timpano ED, Brosky TA. Average depth of tarsometatarsal joint for trephine arthrodesis. J Foot Ankle Surg. 2012; 51(2):168-171.











