Emerging Insights On Gait Changes In Runners
 Could gait retraining have an impact in the treatment and prevention of common running-related injuries? In their review of the literature, these authors say step rate manipulation and changes in foot strike pattern may be beneficial in addressing injuries ranging from patellofemoral pain syndrome to plantar fasciitis.
Could gait retraining have an impact in the treatment and prevention of common running-related injuries? In their review of the literature, these authors say step rate manipulation and changes in foot strike pattern may be beneficial in addressing injuries ranging from patellofemoral pain syndrome to plantar fasciitis.
Running is an increasingly popular sport due to both its convenience and cardiovascular effects. While having extensive cardiovascular benefits, running does have a high rate of musculoskeletal injury. Authors have reported injury rates ranging from 19.4 to 79.3 percent for runners.1
Given this high rate of injury, physicians have proposed numerous modalities to both prevent and treat running-induced injuries. Change in gait is one modality that may help treat and prevent running-related injuries. Runners can achieve gait changes both passively by modification of the running environment and actively via gait retraining strategies.
Mechanics theoretically play a large role in the development of musculoskeletal injuries in runners and many mechanical gait alterations and abnormalities have been associated with the development of musculoskeletal injury. Some have proposed that gait changes with correction of abnormal mechanics may both lower injury risk and serve as a potential injury treatment modality. Researchers have used gait retraining, the concept of changing movement patterns by real-time feedback, to alter these abnormal mechanics related to injury.2
Many regard gait as a function that is primarily under the control of small neural networks, termed central pattern generators, which are located within the spinal cord. While researchers believe central pattern generator output is relatively fixed, studies have shown that kinematic gait changes are possible through neuromuscular reeducation.3-6
The concept of gait retraining was initially in use for stroke and spinal cord injury rehabilitation with the goal of restoring normal ambulation. When treating patients who have had surgery for musculoskeletal injuries, physicians have incorporated gait retraining to restore normal gait. Eventually, physicians started to assess the use of gait retraining for runners and have identified it as both a prevention and treatment modality for several running-related injuries. These injuries include patellofemoral pain syndrome, tibial stress fracture, Achilles tendinopathy and plantar fasciitis.
Assessing The Relationship Between Gait Mechanics And Musculoskeletal Injury
In order to develop gait retraining strategies to prevent and treat running-related musculoskeletal injuries, one must first identify mechanical gait alterations and abnormalities associated with the development of specific musculoskeletal injuries. Numerous studies have found biomechanical alterations associated with the development of patellofemoral pain syndrome, tibial stress fractures, Achilles tendinopathy and plantar fasciitis in runners.3-6
Patellofemoral pain syndrome is one of the most common running-related injuries. The development of patellofemoral pain syndrome is multifactorial and associated with alterations in both proximal and distal lower extremity gait mechanics.7,8 Specifically, researchers have linked patellofemoral pain syndrome with faulty hip mechanics including increased hip adduction and internal rotation.7,8 At the knee, studies have found patellofemoral pain syndrome to be associated with increased knee external rotation at the peak knee extension moment.9 Distally, patellofemoral pain syndrome is associated with a rearfoot strike pattern, increased rearfoot eversion at heel strike, delayed timing of peak rearfoot eversion and a reduced rearfoot eversion range.9-10
Tibial stress fractures are among the most common overuse injuries occurring in runners. When the foot strikes the ground during running, the runner is transmitting repetitive high magnitude forces to the musculoskeletal system.11 Research has shown that this repetitive loading along with bone geometry are associated with the development of tibial stress fractures.12,13 Several mechanical factors are associated with an increased risk of tibial stress fractures in runners. These factors include increased peak positive acceleration of the tibia, high vertical ground reaction forces, high loading rates and increased impact peak magnitude.14-16
Multiple anatomic and biomechanical risk factors have been associated with the development of Achilles tendinopathy in runners. An initial hypothesis was that Achilles tendinopathy resulted from hyperpronation with a more rapid transition to maximum pronation, creating a torsion effect on the tendon.17,18
 Subsequent studies have shown other biomechanical abnormalities associated with Achilles tendinopathy. For example, Lorimer and colleagues showed a close association of high braking forces with Achilles tendon injury risk.19 Further, Van Ginckel and coworkers found reduced anterior displacement of the center of force and laterally directed force distribution at forefoot contact to be risk factors for the development of Achilles tendonitis.20 Additionally, recent research has shown the role that proximal biomechanical abnormalities play in the development of lower limb injuries. Specifically, Franettovich and colleagues found runners with Achilles tendinopathy to have altered neuromotor control of the gluteal muscles.21
Subsequent studies have shown other biomechanical abnormalities associated with Achilles tendinopathy. For example, Lorimer and colleagues showed a close association of high braking forces with Achilles tendon injury risk.19 Further, Van Ginckel and coworkers found reduced anterior displacement of the center of force and laterally directed force distribution at forefoot contact to be risk factors for the development of Achilles tendonitis.20 Additionally, recent research has shown the role that proximal biomechanical abnormalities play in the development of lower limb injuries. Specifically, Franettovich and colleagues found runners with Achilles tendinopathy to have altered neuromotor control of the gluteal muscles.21
Similar to Achilles tendon injuries, multiple factors contribute to the development of plantar fasciitis in runners. These factors include foot structure, shoe gear, training regimens, gait mechanics, flexibility, running surface and body habitus. In terms of gait, research has linked the development of plantar fasciitis with increased load on the plantar fascia during ground contact. Pohl and colleagues found plantar fasciitis to be associated with greater vertical ground reaction force load rates.22 Wearing and colleagues found that regional loading of the plantar fascia was associated with increased plantar fascia thickness and pain.23
What You Should Know About Step Rate Manipulation And Changes In Foot Strike Patterns
Following the identification of alterations in gait mechanics that are related to musculoskeletal injuries, one can develop strategies for gait retraining to correct these movement patterns. Two of the most commonly used gait retraining strategies include changes in step rate and modification of the foot strike pattern.
The effect of step rate manipulation has been one of the most studied areas in gait change and running mechanics. Heiderscheit and coworkers examined the effect of increasing cadence to 5 and 10 percent above the individual runner’s preferred cadence on running mechanics and impact forces.24 They found this step rate increase resulted in numerous alterations in running mechanics that may be beneficial in terms of injury. These alterations include decreased heel strike, decreased braking impulse and decreased vertical excursion. Additionally, the authors found that the increased step rate to 5 or 10 percent above the preferred cadence resulted in significantly lower impact forces.
Hobara and colleagues support these findings, similarly showing that increasing step rate above a runner’s preferred rate resulted in decreased impact forces and peak vertical ground reaction forces.25
Change in foot strike pattern is another frequently studied area of gait change in runners. While runners can achieve changes in foot strike pattern through barefoot running or minimalist shoe gear, these changes can also occur through gait retraining strategies. Given that barefoot running presents obvious physical and environmental limitations, and research has shown it to provide no benefit in terms of energetic cost in comparison to wearing lightweight running shoes, gait retraining is often a superior modality to change foot strike pattern.26
Authors have proposed that the midfoot/forefoot strike gait pattern, which is characteristic of barefoot running, contributes to a lower risk of running-related injuries due to its ability to lower impact.27 Researchers have observed that rearfoot strike runners incur nearly twice as many repetitive stress-related injuries as forefoot strike runners.27 Gait change in runners from a rearfoot strike pattern to a midfoot/forefoot strike pattern results in decreased impact magnitude at the heel, lower step length, lower contact time, higher plantarflexion and lower activation of the tibialis anterior.28-35
Gait Retraining: Can It Be Beneficial In Addressing Patellofemoral Pain Syndrome?
Various researchers have demonstrated that gait retraining can be successful in the treatment and prevention of several lower extremity musculoskeletal injuries. Despite gait being primarily driven by central pattern generators located within the spinal cord, research has shown that conscious modification of movement patterns while running can lead to lasting changes in gait, reduced pain, improved function and reduced injury risk.2,8,10,19,21,22,25,36-40
 There are numerous reports of the use of gait retraining for the treatment of patellofemoral pain syndrome in runners. Cheung and colleagues modified foot strike pattern to treat patellofemoral pain syndrome in runners.10 In this study, the authors utilized gait retraining strategies to change the landing pattern from a rearfoot to a midfoot or forefoot strike pattern. This change in landing pattern resulted in decreased vertical impact peak magnitude and decreased loading rate as well as improvement in symptoms and reduction of the functional limitations associated with patellofemoral pain.
There are numerous reports of the use of gait retraining for the treatment of patellofemoral pain syndrome in runners. Cheung and colleagues modified foot strike pattern to treat patellofemoral pain syndrome in runners.10 In this study, the authors utilized gait retraining strategies to change the landing pattern from a rearfoot to a midfoot or forefoot strike pattern. This change in landing pattern resulted in decreased vertical impact peak magnitude and decreased loading rate as well as improvement in symptoms and reduction of the functional limitations associated with patellofemoral pain.
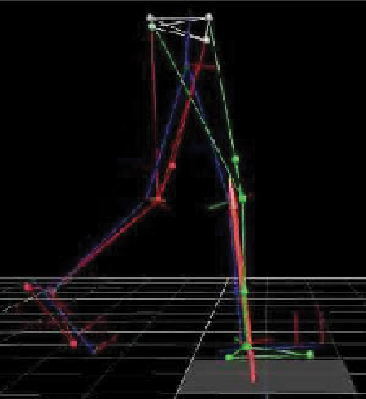
Noehren and coworkers also used gait retraining as a successful treatment modality for patellofemoral pain syndrome in runners.36 In this study, researchers corrected faulty hip mechanics by using real-time kinematic feedback from a motion capture system. By matching their hip angles to normal hip angles on a monitor, the study participants were able to obtain and maintain improved movement patterns as well as reduced pain and improved function scores.
Similarly, Willy and coworkers used gait retraining to correct faulty hip mechanics to address patellofemoral pain syndrome in runners.8 In this study, using a mirror rather than a more advanced and less clinically applicable motion capture system, runners were able to improve measures of abnormal hip mechanics during running, decrease reported pain and improve function.
What Studies Reveal About Gait Alterations And Reduced Risk For Tibial Stress Fractures
Numerous biomechanical and gait alterations are associated with tibial stress fracture and alteration of these running mechanics has the potential to decrease a runner’s risk of tibial stress fracture. Several studies using various forms of gait retraining have shown that gait changes can be successful in reducing tibial acceleration and vertical loading, potentially reducing stress fracture risk in runners.2
A recent study by Willy and colleagues used in-field gait retraining and mobile monitoring to address running biomechanics associated with tibial stress fractures.37 In this study, a group of healthy but at-risk runners exhibiting high impact forces had training to increase their step rate by 7.5 percent. The increased step rate was effective in reducing the impact forces that are associated with a higher risk of tibial stress fractures. Additionally, Edwards and colleagues used a probabilistic model of bone damage, repair and adaptation to show that a 10 percent reduction in stride length (corresponding to a 10 percent increase in step rate) resulted in a decreased risk of developing a tibial stress fracture.38
 Further research is needed to evaluate if these gait retraining modalities and resulting biomechanical modifications lead to a true reduction in injury rates.
Further research is needed to evaluate if these gait retraining modalities and resulting biomechanical modifications lead to a true reduction in injury rates.
Could Gait Retraining Help Reduce Achilles Tendon Injuries?
Multiple risk factors, including several gait abnormalities, have been associated with the development of Achilles tendon injuries. While studies examining the use of gait retraining for the treatment and prevention of Achilles tendon injury are lacking, some have suggested that gait retraining could be a potential treatment strategy to address underlying biomechanical abnormalities contributing to Achilles tendinopathy.
Lorimer and colleagues identified a high braking force to be clearly associated with Achilles tendon injury risk.19 They hypothesized that gait retraining to direct the center of mass forward and reduce braking force could be useful in decreasing the risk of Achilles tendon injury. Additionally, Franettovich and coworkers found altered neuromotor control of gluteal muscles in runners with Achilles tendinopathy and recommended assessing and retraining the gluteal muscles for the management of patients with Achilles tendinopathy.21
Assessing The Potential Of Gait Retraining In Runners With Plantar Fasciitis
 Multiple studies have identified modifiable gait alterations in runners that can contribute to plantar fasciitis. Recently, Wellenkotter and colleagues found that increasing cadence reduced plantar loading, which research has found to be associated with increased plantar fascia thickness and pain.23,39 In this study, a 5 percent increase in step rate reduced plantar fascia loading by 2.4 to 8 percent.39 While this reduction in loading was modest, for longer distance runners, the cumulative effect of this load reduction may be significant and larger increases in step rate may provide even larger reductions in plantar fascia loading. Additionally, Pohl and colleagues found plantar fasciitis to be associated with greater vertical loading rates.22
Multiple studies have identified modifiable gait alterations in runners that can contribute to plantar fasciitis. Recently, Wellenkotter and colleagues found that increasing cadence reduced plantar loading, which research has found to be associated with increased plantar fascia thickness and pain.23,39 In this study, a 5 percent increase in step rate reduced plantar fascia loading by 2.4 to 8 percent.39 While this reduction in loading was modest, for longer distance runners, the cumulative effect of this load reduction may be significant and larger increases in step rate may provide even larger reductions in plantar fascia loading. Additionally, Pohl and colleagues found plantar fasciitis to be associated with greater vertical loading rates.22
Alterations in step rate are associated with reductions in vertical loading rate and thus may be beneficial in reducing the risk of plantar fasciitis. Support for this notion comes from Hobara and coworkers, who found that runners can reduce vertical loading rate by increasing step rate, and from Crowell and Davis, who found that running with a soft, quiet footfall also reduced vertical loading rate.2,25
In a specific study examining the use of gait retraining to treat plantar fasciitis, Davis was able to use gait retraining in a runner with plantar fasciitis to correct abnormal internal hip rotation, knee valgus and a high degree of midfoot pronation.40 Following an eight-week gait retraining program using visual (mirror) and auditory cues, the runner was able to reduce hip internal rotation, hip adduction and knee abduction. These gait changes resulted in resolution of the runner’s plantar fascia pain and improvement in running function.
In Conclusion
Gait changes to correct abnormal running mechanics are a potential treatment and prevention modality for many running-related injuries. Before implementing a gait retraining program for a runner, Heiderscheit and coworkers recommended the clinicians consider a number of factors. These factors include individuals who are likely to benefit; gait parameters to change; the number of sessions and timeframe needed to achieve change; effective visual, verbal or auditory cues to facilitate desired changes; and the environment in which retraining should take place.41
In the future, gait retraining may be a more commonly prescribed modality for treating running-related injuries. Further research is needed to determine the effect of gait changes on injury prevention and treatment, and to ascertain optimal gait retraining programs.
Dr. Hoffman is in private practice in Boulder, Colo. She is the Chief of the Surgery Section at Boulder Community Hospital in Boulder, Colo. Dr. Hoffman is a Fellow of the American College of Foot and Ankle Surgeons.
Dr. Thompson is an Assistant Professor of Exercise Science at Fort Lewis College in Durango, Colo. Her research focuses on understanding the role of different types of sensory feedback in the biomechanics of locomotion.
References
- Van Gent RN, Siem D, van Middelkoop M, van Os AG, Bierma-Zeinstra SM, Koes BW. Incidence and determinants of lower extremity running injuries in long distance runners: a systematic review. Br J Sports Med. 2007;41(8):469-480; discussion 480.
- Crowell HP, Davis IS. Gait retraining to reduce lower extremity loading in runners. Clin Biomech. 2011;26(1):78-83.
- Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes. Decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24(6):765-773.
- Messier SP, Cirillo KJ. Effects of a verbal and visual feedback system on running technique, perceived exertion and running economy in female novice runners. J Sports Sciences. 1989;7(2):113-126.
- Burnside IG, Tobias HS, Bursill D. Electromyographic feedback in the remobilization of stroke patients: a controlled trial. Arch Phys Med Rehab. 1982;63(5):217-222.
- Intiso D, Santilli V, Grasso MG, Rossi R, Caruso I. Rehabilitation of walking with electromyographic biofeedback in foot-drop after stroke. Stroke. 1994;25(6):1189-1192.
- Noehren B, Hamill J, Davis I. Prospective evidence for a hip etiology in patellofemoral pain. Med Sci Sports Exerc. 2013;45(6):1120-1124.
- Willy RW, Scholz JP, Davis IS. Mirror gait retraining for the treatment of patellofemoral pain in female runners. Clin Biomech. 2012;27(10):1045-1051.
- Barton CJ, Levinger P, Menz HB, Webster KE. Kinematic gait characteristics associated with patellofemoral pain syndrome: a systematic review. Gait Posture. 2009;30(4):405-416.
- Cheung RT, Davis IS. Landing pattern modification to improve patellofemoral pain in runners: a case series. J Ortho Sports Phys Ther. 2011;41(12):914-919.
- Nigg BM, De Boer RW, Fisher V. A kinematic comparison of overground and treadmill running. Med Sci Sports Exerc. 1995;27(1):98-105.
- Giladi M, Milgrom C, Simkin A, et al. Stress fractures and tibial bone width. A risk factor. J Bone Joint Surg Br. 1987;69(2):326-329.
- Crossley K, Bennell KL, Wrigley T, Oakes BW. Ground reaction forces, bone characteristics, and tibial stress fracture in male runners. Med Sci Sports Exerc. 1999;31(8):1088-1093.
- Milner CE, Ferber R, Pollard CD, Hamill J, Davis IS. Biomechanical factors associated with tibial stress fracture in female runners. Med Sci Sports Exerc. 2006;38(2):323-328.
- Pohl MB, Mullineaux DR, Milner CE, Hamill J, Davis IS. Biomechanical predictors of retrospective tibial stress fractures in runners. J Biomech. 2008;41(6):1160-1165.
- Grimston SK, Kloiber R, Hanley DA. Bone mass, external loads and stress fractures in female runners. Int J Sports Biomech. 1991;7(3):292–302.
- Maffulli N, Wong J, Almekinders LC. Types and epidemiology of tendinopathy. Clin Sports Med. 2003;22(4):675-692.
- McCrory JL, Martin DF, Lowery RB, et al. Etiologic factors associated with Achilles tendinitis in runners. Med Sci Sports Exerc. 1999;31(10):1374-1381.
- Lorimer AV, Hume PA. Achilles tendon injury risk factors associated with running. Sports Med. 2014;44(10):1459-1472.
- Van Ginckel A, Thijs Y, Hesar NG, et al. Intrinsic gait-related risk factors for Achilles tendinopathy in novice runners: a prospective study. Gait Posture. 2009;29(3):387-391.
- Franettovich Smith MM, Honeywill C, Wyndow N, Crossley KM, Creaby MW. Neuromotor control of gluteal muscles in runners with achilles tendinopathy. Med Sci Sports Exerc. 2014;46(3):594-599.
- Pohl MB, Hamill J, Davis IS. Biomechanical and anatomic factors associated with a history of plantar fasciitis in female runners. Clin J Sport Medicine J Canad Acad Sport Med. 2009;19(5):372-376.
- Wearing SC, Smeathers JE, Sullivan PM, Yates B, Urry SR, Dubois P. Plantar fasciitis: are pain and fascial thickness associated with arch shape and loading? Phys Ther. 2007;87(8):1002-1008.
- Heiderscheit BC, Chumanov ES, Michalski MP, Wille CM, Ryan MB. Effects of step rate manipulation on joint mechanics during running. Med Sci Sports Exerc. 2011;43(2):296-302.
- Hobara H, Sato T, Sakaguchi M, Sato T, Nakazawa K. Step frequency and lower extremity loading during running. Int J Sports Med. 2012;33(4):310-313.
- Franz JR, Wierzbinski CM, Kram R. Metabolic cost of running barefoot versus shod: is lighter better? Med Sci Sports Exerc. 2012;44(8):1519-1525.
- Daoud AI, Geissler GJ, Wang F, Saretsky J, Daoud YA, Lieberman DE. Foot strike and injury rates in endurance runners: a retrospective study. Med Sci Sports Exerc. 2012;44(7):1325-1334.
- Squadrone R, Gallozzi C. Biomechanical and physiological comparison of barefoot and two shod conditions in experienced barefoot runners. J Sports Med Phys Fitness. 2009;49(1):6-13.
- Lieberman DE. What we can learn about running from barefoot running: an evolutionary medical perspective. Exerc Sport Sci Rev. 2012;40(2):63-72.
- Lieberman DE, Venkadesan M, Werbel WA, et al. Foot strike patterns and collision forces in habitually barefoot versus shod runners. Nature. 2010;463(7280):531-535.
- Goss DL, Gross MT. A review of mechanics and injury trends among various running styles. U.S. Army Med Dept J. 2012:62-71.
- Divert C, Baur H, Mornieux G, Mayer F, Belli A. Stiffness adaptations in shod running. J App Biomech. 2005;21(4):311-321.
- Divert C, Mornieux G, Baur H, Mayer F, Belli A. Mechanical comparison of barefoot and shod running. Int J Sports Med. 2005;26(7):593-598.
- Giandolini M, Arnal PJ, Millet GY, et al. Impact reduction during running: efficiency of simple acute interventions in recreational runners. Euro J App Phys. 2013;113(3):599-609.
- Thompson MA, Lee SS, Seegmiller J, McGowan CP. Kinematic and kinetic comparison of barefoot and shod running in mid/forefoot and rearfoot strike runners. Gait Posture. 2015; epub March 12.
- Noehren B, Scholz J, Davis I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. Brit J Sports Med. 2011;45(9):691-696.
- Willy RW, Buchenic L, Rogacki K, Ackerman J, Schmidt A, Willson JD. In-field gait retraining and mobile monitoring to address running biomechanics associated with tibial stress fracture. Scand J Med Sci Sports. 2015; epub Feb. 4.
- Edwards WB, Taylor D, Rudolphi TJ, Gillette JC, Derrick TR. Effects of stride length and running mileage on a probabilistic stress fracture model. Med Sci Sports Exerc. 2009;41(12):2177-2184.
- Wellenkotter J, Kernozek TW, Meardon S, Suchomel T. The effects of running cadence manipulation on plantar loading in healthy runners. Int J Sports Med. 2014;35(9):779-784.
- Davis I. Gait retraining in runners. Orthopaedic Practice. 2005;12(2):8-14.
- Heiderscheit BC. Gait retraining for runners: in search of the ideal. J Ortho Sports Phys Ther. 2011;41(12):909-910.











