Emerging Insights On The Collapsible Cavus
 Asserting that most pathologic flexible flatfoot deformities are higher arched cavus feet that have collapsed and become misshapen, the author says having an understanding of this concept can help guide conservative and surgical treatments.
Asserting that most pathologic flexible flatfoot deformities are higher arched cavus feet that have collapsed and become misshapen, the author says having an understanding of this concept can help guide conservative and surgical treatments.
Most flat feet are actually cavus feet in disguise. In the strict sense, a true flatfoot is low to flat when the patient is seated and does not change much when the patient is standing. Except for the rocker bottom flatfoot, peroneal spastic flatfoot and a few other isolated pathologies, most of these off-weightbearing and weightbearing flat feet function well since that is their particular characteristic architecture.
These feet act much like a low-arched bridge that is designed to operate smoothly in that position. Problems arise when you have a “bridge” that is designed to be high-arched and starts to collapse when the patient places weight on it. This is true of the foot that exhibits a high arch with the patient seated and no arch when standing.
So when patients say “I have flat feet” but present with significant elevation of the medial longitudinal arch seated and a complete absence when they stand, that is not truly a flatfoot but rather a “flattening” foot. In this instance, the foot should not be flat but due to some inherent or acquired mechanical or systemic imperfection, it is flat.
Depending upon its attendant etiology, this abnormally collapsing foot results in a myriad of problems for the individual, including not only foot and ankle pain/deformity but also knee, hip and back symptomatology. Furthermore, these pathologic superstructural manifestations due to abnormalities in the weightbearing foot posture are not always linked together as cause and effect by the patient or practitioner.
Understanding The Impact Of Medial Longitudinal Arch Height On Foot Function And Stability
The height of the arch is a variable and unreliable indicator of foot and limb function. Both the high and the low arched foot may function well.1 According to Tax in an article on the health hazards of developing children, there is a serious misconception on the part of the public as well as a great number of professionals in equating the problem of flat feet with excessively pronated feet.2 This is a matter of grave concern since flatness of the arch can be a normal or abnormal finding in foot posture whereas the excessively pronated foot is flattened as part of a structural malposition that is present at birth.2
Stability of the medial longitudinal arch is an integral segment of the structural framework, allowing the body to move forward over the supporting limb freely and efficiently.3 Increasing or decreasing medial longitudinal arch height may positively or negatively affect foot function and stability, as well as improve or disrupt mechanical alignment of the lower extremity.4
 Authors have linked a decrease in medial longitudinal arch height to abnormal pronation.5,6 When the medial longitudinal arch functions properly, it allows activation of the windlass effect of the plantar fascia, enabling the foot to provide a rigid lever for propulsion. Etiologic factors implicated in the medial longitudinal arch’s collapse have included: hereditary or acquired structural imperfections, delayed ontogenesis, evolutionary “scars,” ligamentous laxity, obesity, systemic disease, inflammatory arthridities, equinus influences, compensation for limb length discrepancy, trauma, etc.7-10
Authors have linked a decrease in medial longitudinal arch height to abnormal pronation.5,6 When the medial longitudinal arch functions properly, it allows activation of the windlass effect of the plantar fascia, enabling the foot to provide a rigid lever for propulsion. Etiologic factors implicated in the medial longitudinal arch’s collapse have included: hereditary or acquired structural imperfections, delayed ontogenesis, evolutionary “scars,” ligamentous laxity, obesity, systemic disease, inflammatory arthridities, equinus influences, compensation for limb length discrepancy, trauma, etc.7-10
In his lectures in the 1920s and publications in the 1930s and 1940s, Morton ascribed collapse of the medial longitudinal arch upon weightbearing to pathologic bony alignment, the first and foremost being an atavistic short first metatarsal in conjunction with lax ligaments.11,12 Basmajian and Stecko studied musculature activity in the foot through electromyography.13 They concluded that it is the bony structure and alignment of the foot, along with its ligamentous attachments, that are the primary restraints in maintenance of the longitudinal arch. The musculature only comes into play with excessive loads. Mann and Inman noted that these muscles do play an active role in stabilization of the foot during propulsion.14
Researchers describe the flexible flatfoot as a reduction in the height of the medial longitudinal arch upon weightbearing, often in conjunction with rearfoot eversion and/or medial lower leg displacement and abduction of the forefoot (“too many toes” sign).15-17 Jack’s test (or the Hubscher maneuver) or forefoot supination are able to restore the arch.17 The flexible flatfoot may be symptomatic or asymptomatic. Symptomatic flexible flatfoot may be associated with postural pain, Achilles tendinopathy, plantar fasciitis, lower limb cramping, fatigue, etc.16,18-23
The adult-acquired flatfoot has been associated with posterior tibial tendon dysfunction or insufficiency.24 Numerous articles stress the influence of equinus in the manifestation of flatfoot.24-32 In fact, there is a separate classification for the development of foot deformities associated with equinus compensation.25 Harris and Beath, in the classic Ottawa Foot Survey of almost 4,000 Canadian soldiers, were the first to describe pes equinovalgus using the term “hypermobile flatfoot.”32 Characteristics of this flexible foot type include “correction” when unloaded, a contracted tendo-Achilles, an abnormal relationship of the tarsal osseous segments and presence of the hypermobile flatfoot since childhood.3
 The incidence reported in the literature of flexible flatfoot in the adult population is approximately 20 percent.32,34,35 According to Taha and colleagues, most patients with flat feet do not present with acute symptomatology but rather with problems related to cosmesis or shoe wear.17 Those with symptomatic flat feet often complain of pain increasing with the type and amount of activity they perform, and rest usually relieves the pain. Depending upon severity and duration, patients may describe the pain as an aching or gnawing pain affecting the forefoot, midfoot or medial and/or ankle regions. Gait may be antalgic, apropulsive and exhibit forefoot abduction. Talar protrusion is obvious as is an absent medial longitudinal arch. The rearfoot is in valgus with medial displacement of the line of gravity and lower third of the tibia.17
The incidence reported in the literature of flexible flatfoot in the adult population is approximately 20 percent.32,34,35 According to Taha and colleagues, most patients with flat feet do not present with acute symptomatology but rather with problems related to cosmesis or shoe wear.17 Those with symptomatic flat feet often complain of pain increasing with the type and amount of activity they perform, and rest usually relieves the pain. Depending upon severity and duration, patients may describe the pain as an aching or gnawing pain affecting the forefoot, midfoot or medial and/or ankle regions. Gait may be antalgic, apropulsive and exhibit forefoot abduction. Talar protrusion is obvious as is an absent medial longitudinal arch. The rearfoot is in valgus with medial displacement of the line of gravity and lower third of the tibia.17
Keys To Measuring Medial Longitudinal Arch Height
The measurement of arch height is a method of characterizing foot shape and structure. It also allows comparison between the off-weightbearing and weightbearing foot. First described by Williams and McClay, the arch height index is the ratio of the standing or sitting dorsal arch height measurement at 50 percent of foot length divided by 50 percent of the truncated foot length.36 For example, the measurement is the distance from the calcaneus to the first metatarsophalangeal (MPJ) articulation. Arch height index values less than 0.31 mm indicate a low arch, 0.31 to 37 mm indicates a neutral arch and more than 0.37 mm indicates high arched feet.37
The arch rigidity index is the standing arch height index divided by the sitting arch height index. The arch drop is the arch height at 50 percent of foot length with the patient sitting subtracted by the arch height at 50 percent of foot length with the patient standing.37
Pertinent Insights On Pes Cavus
 We typically think of the classic cavus foot and the literature typically refers to it as an abnormal elevation of the medial longitudinal arch upon weightbearing. It is a high-arched, rigid foot type with the posterior tibial and peroneus longus tendons consistently stronger than the anterior and the brevis. The etiology of the cavus foot, if not the idiopathic variety, is often linked to neuromotor disease processes such a muscular dystrophy, Charcot-Marie-Tooth, poliomyelitis, syringomyelia, peroneal nerve trauma, Friedreich’s ataxia, or post-cerebrovascular accident.38
We typically think of the classic cavus foot and the literature typically refers to it as an abnormal elevation of the medial longitudinal arch upon weightbearing. It is a high-arched, rigid foot type with the posterior tibial and peroneus longus tendons consistently stronger than the anterior and the brevis. The etiology of the cavus foot, if not the idiopathic variety, is often linked to neuromotor disease processes such a muscular dystrophy, Charcot-Marie-Tooth, poliomyelitis, syringomyelia, peroneal nerve trauma, Friedreich’s ataxia, or post-cerebrovascular accident.38
Shaffer first described the cavus foot in 1885 and researchers have sometimes referred to it as a “Shaffer foot.”39 Characteristically, this is essentially a semi-rigid to rigid foot type that exhibits a varus rearfoot, a plantarflexed and adducted forefoot, and calcaneal inclination of 30 degrees or higher. There is a marked reduction in the available weightbearing surface contact area. In essence, the higher the arch, the lower the surface contact area.
The incidence of cavus foot is reportedly 8 to 15 percent although in a clinical and radiographic study of 2,047 skeletally mature adult patients with diabetes, the incidence of pes cavus was 24 percent.40 Surprisingly, in this same study, the incidence of flatfoot was only 19 percent.40
A Closer Look At The Types And Pathomechanics Of The Cavus Foot
Manoli in 2005 and Chilvers and Manoli in 2007 discuss a “subtle” cavus foot type in which there is a higher arch than normal, but one that is not associated with neuromuscular disease. This less severe form of pes cavus occurs more commonly in the normal population but researchers offer no rate of occurrence.41,42
The authors go on to describe forefoot- and hindfoot-driven cavus foot types. The forefoot-driven type is due to plantarflexion of the first ray resulting in a supinated longitudinal axis of the midtarsal joint during midstance throughout propulsion. The hindfoot-driven cavus occurs as a result of severe varus alignment and function of the rearfoot exerting an excessive repetitive supinatory moment beginning at heel contact and continuing throughout the stance phase of gait. This foot type may begin as forefoot-driven and then progress to hindfoot-driven.41,42
Like most classic cavus feet, there is a preponderance of supinatory motion and diminished, if any, adaptive phase, shock-absorbing subtalar joint pronation. Therefore, this foot type is frequently associated with chronic lateral ankle instability, peroneal tendinitis and overuse syndromes, lateral knee, hip and back pain, postural instability, lateral fascial band strain, etc. Upon weightbearing, this foot retains its high-arched appearance with a varus-directed hindfoot, which, when viewing this anterior to posterior, exhibits the pathognomonic “peek-a-boo” heel sign.42
These forefoot- and hindfoot-driven cavus foot types are in essence analogous to the anterior and posterior classification schematic for cavus feet. The anterior type represents plantarflexion of the first ray and/or entire forefoot either at the tarsometatarsal articulation or midtarsal joint. The posterior type has a significant calcaneal inclination angle but no forefoot equinus.38 Additionally, there can be a combination of the two types, which is referred to as a global cavus.
 We may simply classify cavus feet as either flexible or rigid. The flexible type possesses enough ankle joint or, if necessary, midtarsal joint dorsiflexion to allow anterior equinus deficiencies to be compensated for upon weightbearing. The uncompensated type of cavus foot has a higher incidence of genu recurvatum and an inability of the anterior tibial musculature to negate the plantigrade position of the foot during static stance and gait.43
We may simply classify cavus feet as either flexible or rigid. The flexible type possesses enough ankle joint or, if necessary, midtarsal joint dorsiflexion to allow anterior equinus deficiencies to be compensated for upon weightbearing. The uncompensated type of cavus foot has a higher incidence of genu recurvatum and an inability of the anterior tibial musculature to negate the plantigrade position of the foot during static stance and gait.43
Whitney and Greene first described and categorized the anterior cavus foot in 1982 in their classic article entitled “Pseudoequinus.”44 They described the entity of pseudoequinus as a functional dorsiflexion deficit of the ankle joint caused by an inherent or acquired sagittal plane structural deficiency. Since the forefoot is plantarflexed on the rearfoot, additional dorsiflexion at the ankle is required to allow the calcaneus to reach the supporting surface, thereby employing most if not all available dorsiflexion. The remaining required dorsiflexion is acquired via subtalar and oblique midtarsal joint compensation, thereby collapsing the foot.
Whitney and Green divided anterior equinus into four categories depending upon which segment of the forefoot exhibited sagittal plane plantarflexion deformity.44 Metatarsus cavus deformity occurs at Lisfranc’s articulation and primarily affects the first metatarsal. Lesser tarsus cavus exhibits plantarflexion of the forefoot on the rearfoot over the lesser tarsal bones. Forefoot cavus occurs at the midtarsal joint with pathognomonic talar head prominence when the patient is off-weightbearing. Finally, a combined type of any of the preceding types may occur. Whitney and Green go on to state if the lesser tarsal area can completely absorb the anterior cavus (equinus) deformity, the foot may appear relatively normal in its weightbearing state.
Why The Collapsible Cavus Is Not A Flexible Flatfoot
The collapsible cavus foot, like the “subtle” cavus, is not associated with neuromotor disease and has an abnormally high-arched appearance when the foot is off weightbearing. However, unlike the subtle cavus, it completely flattens upon weightbearing. Additionally, unlike the more rigid subtle cavus foot, which presents with a propensity for excessive supination, the collapsible cavus belies its off-weightbearing architecture and excessively pronates with loading.
Yes, it is a flexible flatfoot in appearance but in its elemental form, it is actually a cavus foot gone astray. This collapsible cavus foot more closely resembles the compensated anterior equinus foot with increased tri-planar compensatory mechanisms taking place in a flexible system.
In a retrospective review that I conducted in my practice of the arch morphology, I observed off-weightbearing and weightbearing in 100 randomly selected patients with a high-arched foot off weightbearing.44 My review revealed that upon weightbearing, 65 percent of patients had flat feet, 28 percent had low arches and 7 percent had medium arch morphology. None of the randomly sampled patient population retained the high arched morphology observed when they were off-weightbearing.
 What You Should Know About The Etiology Of The Cavus Foot
What You Should Know About The Etiology Of The Cavus Foot
The evolution of the human foot is still incomplete. Our three-dimensional pedal architecture is still better suited for grasping and climbing in a semi-arboreal habitat than it is for walking on hard, flat two-dimensional surfaces. As part of this transition process, the heel has not yet fully come down to meet the supporting surface. Equinus influences in the foot and ankle represent atavistic characteristics that present a destructive force into the foot of modern man. These evolutionary “scars” create inherent biomechanical defects that are present in the feet of most newborns and, as Tax has repeatedly stated, are responsible for most postural pathology of the lower extremity.2
Most flexible flat feet are only flat upon weightbearing. Due to a host of etiologic factors, the intended inherited anatomic higher-arched architecture is disrupted by an inability to maintain its shape upon loading. In essence and in the vast majority of instances, underlying the observed weightbearing flexible flatfoot is a flexible cavus foot in need of realignment. This is not a flat foot but a “flattening” foot.
A significant percentage of these flat feet are not fundamentally flat feet at all but actually higher arched feet that fail to maintain their structure in function. For the most part, the flexible flatfoot is a flexible cavus foot type that collapses upon weightbearing.
The incidence of truly flexible flatfooted individuals (i.e. both weightbearing and off-weightbearing) is smaller than clinicians have commonly thought. In fact, many of these true low- to no-arch foot types are asymptomatic and function quite well. I believe the reason for this lies in the fact that the degree of collapse upon weightbearing does not differ greatly from what we observe in the examination chair. There are some exceptions, one of which is the compensated gastrocnemius equinus foot type, which results in a rocker bottom flatfoot with attendant symptomatology and deformity that is obviously present with weightbearing and off-weightbearing.
Identifying The Collapsible Cavus
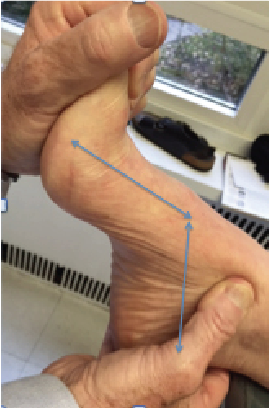
With the patient in the off-weightbearing position with the subtalar joint in neutral position, load the forefoot to resistance at the ankle (see photo 3). Note the level of sagittal plane forefoot deviation on the rearfoot as well as the level at which it occurs (see photo 4). One can also suggest recommendations on appropriate heel height based on this measurement (see photo 5). Proceed to classify arch height into categories such as flat, low, medium or high. I further grade high-arched feet from +1 to +6 in ascending severity. Alternately, you can break it up into mild, moderate and severe, or use the arch rigidity index and/or arch drop measurements depending upon your personal preference.
 Have the patient stand and note whether the arch height has been maintained, lowered or flattened (see photo 6). If arch height is significantly lowered or flattened, observe talar head prominence, marked valgus rearfoot position, medial displacement of the line of gravity, the “too many toes” sign, convexity to the medial border of the medial longitudinal arch, convex lateral border with shortening, etc. (see photo 7). Palpate the foot in subtalar joint neutral position and note the difference between ideal alignment and foot posture upon weightbearing.
Have the patient stand and note whether the arch height has been maintained, lowered or flattened (see photo 6). If arch height is significantly lowered or flattened, observe talar head prominence, marked valgus rearfoot position, medial displacement of the line of gravity, the “too many toes” sign, convexity to the medial border of the medial longitudinal arch, convex lateral border with shortening, etc. (see photo 7). Palpate the foot in subtalar joint neutral position and note the difference between ideal alignment and foot posture upon weightbearing.
A historical method of determining arch collapse is the measurement of “scaphoid or navicular differential” or “navicular drop.” Depression or lowering of the navicular from a subtalar neutral position of more than 3/8 inches or 9 mm with or without symptomatology is pathologic.45,46
First described and utilized by Schuster, another method to evaluate the degree of pathologic arch collapse is to use a free-swinging protractor or level finder to measure the plane of the forefoot at the first and fifth metatarsophalangeal articulations both in the relaxed stance and subtalar joint neutral position. The difference between the two is the measurement of the total varus influence on the foot. The higher the number, the more pathomechanically dysfunctional the foot.47,48
In Conclusion
Most pathologic flexible flatfoot deformities are actually cavus feet that have collapsed and become misshapen as a result of pathomechanical compensation for some specific phylogenic and ontogenic defect, deficiency or systemic disease process. They are not fundamentally flat feet but actually higher arched feet that have failed to maintain their structure in function. For the most part, the flexible flatfoot is a flexible anterior cavus foot type that collapses upon weightbearing.
Understanding and appreciating this fact will allow the astute practitioner to improve both conservative- and surgical-based management outcomes. Knowledge of the underlying etiology that has created the presenting complaint — be it pain, deformity or both — will allow the surgeon to select more appropriate procedures, thereby targeting the cause as well as its effect. Conservative management allows the clinician more efficient, precise and timely control of deforming forces, thereby reducing pain, improving function and stabilizing, and at times improving deformities. Conservative management may include prescription foot orthoses, muscle strengthening and/or stretching, fitness activity counseling, footwear counseling and modifications, local modalities, etc. In some cases, we may of necessity use surgical intervention to augment conservative management to correct the underlying deformity at the precise level of its occurrence.
Habbu and colleagues from the American Orthopaedic Foot and Ankle Society performed a retrospective review of 374 patients who had surgery to treat stage II adult-acquired flatfoot deformity.24 The procedures included a metatarsocuneiform fusion, a metatarsal shortening osteotomy, hallux valgus and hammertoe repair, and gastrocnemius recession. The authors concluded that a combination of all these procedures together produced the best results with the highest patient satisfaction rates. They further went on to state “restoration of normal foot and ankle mechanics by addressing the underlying etiology at the time of surgery is important in the prevention of deformity recurrence and also in patient satisfaction.”
Recognition of the fact that many of these pathologic flat feet are fundamentally higher arched feet that have collapsed with the likelihood of pseudoequinus-induced sagittal plane compensation as their etiology will undoubtedly improve patient outcomes. After all, isn’t this what Root, Weed, Sgarlato, Schuster, Tax, Ganley, McGlamry, Subotnick, Gerbert, Scherer, Schoenhaus, Kirby, LaPorta, Greene, Dananberg, Valmassy, Blake and other luminaries in the field of podiatric biomechanics and surgery have been advocating for the past 50 years?
 Dr. D’Amico is a Professor and former Chairman of the Department of Orthopedics and Pediatrics at the New York College of Podiatric Medicine. He is a Diplomate of the American Board of Podiatric Medicine, and a Diplomate of the National Academies of Practice. He is a Fellow of the American Academy of Podiatric Sports Medicine, and a Fellow of the American College of Foot and Ankle Orthopedics and Medicine. Dr. D’Amico is in private practice in New York City.
Dr. D’Amico is a Professor and former Chairman of the Department of Orthopedics and Pediatrics at the New York College of Podiatric Medicine. He is a Diplomate of the American Board of Podiatric Medicine, and a Diplomate of the National Academies of Practice. He is a Fellow of the American Academy of Podiatric Sports Medicine, and a Fellow of the American College of Foot and Ankle Orthopedics and Medicine. Dr. D’Amico is in private practice in New York City.
Dr. D’Amico expresses sincere appreciation to Loretta Cacace, DPM, for her assistance in the preparation, review and proper referencing of this article. The author also would like to thank Paul Tremblay, the Chief Medical Librarian at the New York College of Podiatric Medicine, for his assistance in obtaining articles for this project.
References
- Lobo M, Greisberg J. Adult acquired flatfoot. In: Digiovanni C, Greisberg J (eds.) Foot and Ankle: Core Knowledge in Orthopaedics, Volume 1. Elsevier Mosby, Philadelphia, 2007, pp. 38-57.
- Tax HR. Excessively pronated feet: A health hazard to developing children. Child Adolesc Soc Work J. 1993; 10(5):431–40.
- D’Amico JC. Understanding the First ray. Podiatr Manage. 2016;35(7):109-122.
- Queen RM, Mall NA, Hardaker WM, Nunley JA 2nd. Describing the medial longitudinal arch using footprint indices and a clinical grading system. Foot Ankle Int. 2007; 28(4):456-462.
- Leung AK, Mak AF, Evans JH. Biomedical gait evaluation of the immediate effect of orthotic treatment for flexible flat foot. Prosthet Orthot Int. 1998; 22(1):25-34.
- Razeghi M, Batt ME. Foot type classification: A critical review of current methods. Gait Posture. 2002;15(3):282-291.
- Shultz SP, Anner J, Hills AP. Paediatric obesity, physical activity and the musculoskeletal system. Obes Rev. 2009; 10(5):576-582.
- Dowling AM, Steele JR, Baur LA. Does obesity influence foot structure and plantar pressure patterns in prepubescent children? Int J Obes Relat Metab Disord. 2001; 25(6):845-852.
- Hills AP, Hennig EM, Byrne NM, Steele JR. The biomechanics of adiposity--structural and functional limitations of obesity and implications for movement. Obes Rev. 2002; 3(1):35-43.
- Bordin D, De Giorgi G, Mazzocco G, Rigon F. Flat and cavus foot, indexes of obesity and overweight in a population of primary-school children. Minerva Pediatr. 2001; 53(1):7-13.
- Morton DJ, Fuller DD. Human Locomotion and Body Form. A Study of Gravity and Man. Williams and Wilkins, Baltimore, 1952, p. 74.
- Morton DJ. The Human Foot. Columbia University Press, New York, 1935, p. 119.
- Basmajian JV, Stecko G. The role of muscles in arch support of the foot. J Bone Joint Surg Am. 1963; 45:1184–1190.
- Mann R, Inman VT. Phasic activity of intrinsic muscles of the foot. J Bone Joint Surg Am. 1964; 46:469–481.
- Sheykhi-Dolagh R, Saeedi H, Farahmand B, et al. The influence of foot orthoses on foot mobility magnitude and arch height index in adults with flexible flat feet. Prosthet Orthot Int. 2015; 39(3):190-196.
- Banwell HA, Thewlis D, Mackintosh S. Adults with flexible pes planus and the approach to the prescription of customised foot orthoses in clinical practice: A clinical records audit. Foot (Edinb). 2015; 25(2):101-109.
- Sheikh Taha AM, Feldman DS. Painful flexible flatfoot. Foot Ankle Clin. 2015; 20(4):693-704.
- Franco AH. Pes cavus and pes planus. analyses and treatment. Phys Ther. 1987; 67(5):688-694.
- Kosashvili Y, Fridman T, Backstein D, Safir O, Bar Ziv Y. The correlation between pes planus and anterior knee or intermittent low back pain. Foot Ankle Int. 2008; 29(9):910-913.
- Collins N, Bisset L, McPoil T, Vicenzino B. Foot orthoses in lower limb overuse conditions: A systematic review and meta-analysis. Foot Ankle Int. 2007; 28(3):396-412.
- Shibuya N, Jupiter DC, Ciliberti LJ, VanBuren V, La Fontaine J. Characteristics of adult flatfoot in the united states. J Foot Ankle Surg. 2010; 49(4):363-368.
- Van Boerum DH, Sangeorzan BJ. Biomechanics and pathophysiology of flat foot. Foot Ankle Clin. 2003; 8(3):419-430.
- Miller OL. A plastic flat foot operation. J Bone Joint Surg Am. 1927: 9:84-91.
- Habbu R, Holthusen SM, Anderson JG, Bohay DR. Operative correction of arch collapse with forefoot deformity: A retrospective analysis of outcomes. Foot Ankle Int. 2011; 32(8):764-773.
- DiGiovanni CW, Kuo R, Tejwani N, et al. Isolated gastrocnemius tightness. J Bone Joint Surg Am. 2002; 84-A(6):962-970.
- Downey MS, Banks AS. Gastrocnemius recession in the treatment of nonspastic ankle equinus. A retrospective study. J Am Podiatr Med Assoc. 1989; 79(4):159-174.
- Hill RS. Ankle equinus. Prevalence and linkage to common foot pathology. J Am Podiatr Med Assoc. 1995; 85(6):295-300.
- Hoke M. An operation for the correction of extremely relaxed flat feet. J Bone Joint Surg. 1931; 13-A: 773–784.
- Subotnick SI. Equinus deformity as it affects the forefoot. J Am Podiatry Assoc. 1971; 61(11):423-427
- Sgarlato TE, Morgan J, Shane HS, Frenkenberg A. Tendo achillis lengthening and its effect on foot disorders. J Am Podiatry Assoc. 1975; 65(9):849-871.
- Pinney SJ, Hansen ST,Jr, Sangeorzan BJ. The effect on ankle dorsiflexion of gastrocnemius recession. Foot Ankle Int. 2002; 23(1):26-29.
- Harris RI, Beath T. Hypermobile flat-foot with short tendo Achilles. J Bone Joint Surg Am. 1948; 30A(1):116-140.
- Bohay D, Anderson J, Gentchos C. Treatment of stage 2 posterior tibial tendon dysfunction. In: Coetzee, JC, Hurwitz, SR, ed. Arthritis and Arthroplasty: The Foot and Ankle. Saunders, Philadelphia, 2010, pp. 264-272.
- Halabchi F, Mazaheri R, Mirshahi M, Abbasian L. Pediatric flexible flatfoot; clinical aspects and algorithmic approach. Iran J Pediatr. 2013; 23(3):247-260.
- Tenenbaum S, Hershkovich O, Gordon B, et al. Flexible pes planus in adolescents: Body mass index, body height, and gender--an epidemiological study. Foot Ankle Int. 2013; 34(6):811-817.
- Williams DS 3rd, McClay IS, Hamill J. Arch structure and injury patterns in runners. Clin Biomech (Bristol, Avon). 2001; 16(4):341-347.
- Butler RJ, Hillstrom H, Song J, Richards CJ, Davis IS. Arch height index measurement system: Establishment of reliability and normative values. J Am Podiatr Med Assoc. 2008; 98(2):102-106.
- Scherer PR, Choate CC. Current concepts in orthotic therapy for pes cavus. Podiatry Today. 2008; 21(10):58-66.
- Shaffer, NM. Non-deforming clubfoot. With remarks on its pathology. Med Rec. 1885; 27:561
- Ledoux WR, Shofer JB, Ahroni JH, Smith DG, Sangeorzan BJ, Boyko EJ. Biomechanical differences among pes cavus, neutrally aligned, and pes planus feet in subjects with diabetes. Foot Ankle Int. 2003; 24(11):845-850.
- Manoli A 2nd, Graham B. The subtle cavus foot, “the underpronator.” Foot Ankle Int. 2005; 26(3):256-263.
- Chilvers M. Chapter 5: The neuromuscular cavus foot. In: DiGiovanni CW, Greisberg J (eds). Core Knowledge in Orthopedics Foot and Ankle, Mosby, St. Louis, 2007.
- Benedetti MG, Catani F, Ceccarelli F, et al. Gait analysis in pes cavus. Gait Posture. 1997; 5(2):169.
- Whitney AK, Green DR. Pseudoequinus. J Am Podiatry Assoc. 1982; 72(7):365 371.
- D’Amico JC, Richard O. Shuster: A biomechanical icon (part II). Podiatry Management. 2014; 129-137.
- D’Amico JC. Richard O. Shuster: A biomechanical icon (part I). Podiatry Management. 2013; 129-137
- Ross CF, Schuster RO. A preliminary report on predicting injuries in distance runners. J Am Podiatry Assoc. 1983; 73(5):275-277.
- Schuster RO. Origins and implications of frontal plane imbalances of the leg and foot. In Yearbook of Podiatric Medicine and Surgery, Futura, Mt. Kisco, NY, 1981.
For further reading, see “Keys To Correcting Cavus Foot Deformities” in the May 2016 issue of Podiatry Today or “Assessing And Treating The Subtle Cavus Foot Deformity” in the June 2015 issue.











