ADVERTISEMENT
Does Nerve Decompression Improve Static Balance In Patients With Painful Diabetic Neuropathy?
By Brian McCurdy, Managing Editor
A recent s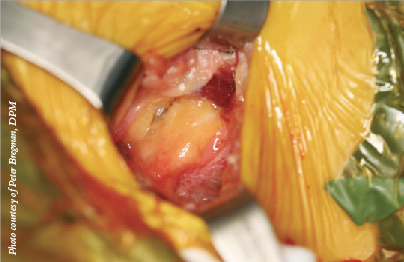 tudy questions whether nerve decompression will improve static balance in patients with diabetic neuropathy.
tudy questions whether nerve decompression will improve static balance in patients with diabetic neuropathy.
The study, recently published in Clinical Rehabilitation, focused on 39 patients with painful diabetic polyneuropathy. Patients had unilateral surgical nerve decompression at four sites in the lower extremity and the study used the contralateral limb as control. Researchers measured weightbearing and five variables of sway of the center of pressure with a pressure mat both with the patients’ eyes open and their eyes closed. The study authors obtained measurements preoperatively and at six and 12 months postoperatively, using the T-test for evaluation of postoperative results.
The authors concluded that there is no evidence that surgical decompression of nerves of the lower extremity in patients with painful diabetic polyneuropathy influences stability.
Stephen Barrett, DPM, FACFAS, has noted significant improvements in balance in many nerve decompression patients, but has not specifically correlated both findings over the last decade that he has performed the surgery. He notes the study focused on unilateral decompressions with the contralateral limb as a control. However, Dr. Barrett cites a 2006 study in the Annals of Plastic Surgery concluding that there was statistically significant improvement in static balance after bilateral decompression both with eyes open and eyes closed in unilaterally decompressed patients.
Dr. Barrett has found that if a patient demonstrates a positive Tinel’s sign or a positive provocation test, the success rate is up to 90 percent for a reduction in pain and 75 to 80 percent for restoration of sensation.
“In properly selected patients, peripheral nerve surgery is highly successful and more than 85 percent of my patients return to have nerve decompression done on their other extremity,” says Dr. Barrett, a Fellow and the President of the Association of Extremity Nerve Surgeons.
Although he has not studied stability after nerve decompression, Peter Bregman, DPM, says his patients have said they can walk better after the surgery due to less pain. If the pain is gone, he says the patients should have more stability in their gait if they are not fighting pain.
Dr. Bregman notes nerve decompression is only effective in patients with a diagnosed nerve compression and adds that the procedure would be contraindicated in patients with renal failure, leg edema or any active ulcers. Dr. Barrett adds that peripheral nerve decompression surgery in patients with diabetes is contraindicated in a patient who does not have adequate vascular supply or has some other comorbidity that would preclude safe surgery.
One year after nerve decompression surgery, Dr. Barrett has found patients have done very well and many relate an increased benefit from pain reduction and the restoration of sensation after 24 months. He says only a few have had to have another decompression surgery due to scar tissue formation.
Dr. Bregman concurs. “They do very well if (decompression is) successful, which is around 85 percent (pain relief). After one year, they have only gotten better, if anything, as far as sensation is concerned, thus reducing risk for ulcer or amputation,” says Dr. Bregman, a Past President of the Association of Extremity Nerve Surgeons.
Study Examines Impact Of Modular Stem, Fixed-Bearing TARs
By Brian McCurdy, Managing Editor
Modular stem fixed-bearing total ankle replacements (TARs) can improve pain, function and disability in patients, according to a recent study in the Journal of Foot and Ankle Surgery.
The study authors looked at three-year outcomes for 23 consecutive patients who received a modular stem, fixed-bearing total ankle replacement. The study noted significant improvements in pain, functional impairment and disability with patients maintaining improvements between years two and three. The surgeons encountered nine complications: one deep infection, two pulmonary embolisms, three wounds, one ectopic bone formation, one stiff joint and one talar subsidence. In the three-year follow-up period, the study notes three patients required additional procedures after the immediate postoperative phase.
Study lead author Stephen Brigido, DPM, notes that the modular fixed bearing prosthetic allows for stable fixation of the tibial component in lesser quality bone, such as periarticular subchondral cysts that often present in end-stage arthritic joints. As he says, the modular stem allows for vertical fixation of that tibial component and permits the surgeon to customize the length and diameter of the stem to meet the patient’s needs.
Generally, Dr. Brigido says patients who are not obese, do not have diabetes and have a well aligned hindfoot are preferred candidates not only for modular stem fixed-bearing total ankle replacements but all ankle replacement systems. For patients with a limb or hindfoot deformity, he advises performing deformity correction in either a staged or concomitant procedure.
Dr. Brigido, a Fellow of the American College of Foot and Ankle Surgeons, says the study’s ankle replacement technique is contraindicated in morbidly obese people, those with uncontrolled diabetes and patients who have a history of Charcot arthropathy. He does not perform ankle arthroplasty in patients who have a significant valgus deformity of the ankle joint.
Of the nine complications in the study, Dr. Brigido says only the deep infection impeded prosthetic survival and patient satisfaction while all other complications were either resolved or a non-issue.
Dr. Brigido, the Fellowship Director of Foot and Ankle Reconstruction at Coordinated Health in Bethlehem, Pa., does advise surgeons that there is a learning curve with ankle replacement systems. He says one must pick an appropriate system, address the deformity and handle any potential complications.
“As instrumentation and alignment/targeting systems improve, implanting the prosthetic has become more reproducible,” says Dr. Brigido.











