ADVERTISEMENT
Does First Ray Hypermobility Exist With Hallux Valgus?
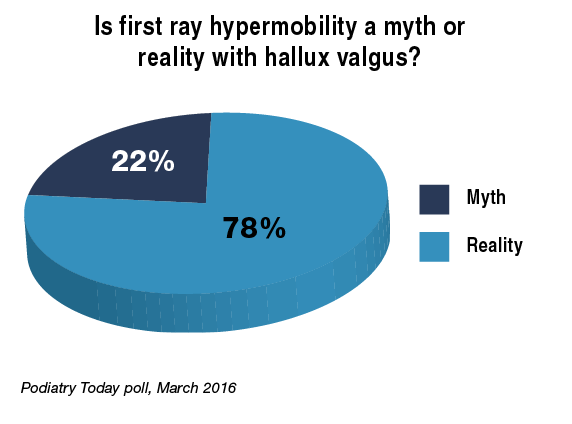 Is first ray hypermobility a legitimate factor in patients with bunions? In a recent Podiatry Today online poll, 78 percent of respondents agree hypermobility is real while 22 percent feel it is a myth.
Is first ray hypermobility a legitimate factor in patients with bunions? In a recent Podiatry Today online poll, 78 percent of respondents agree hypermobility is real while 22 percent feel it is a myth.
“I am convinced that hypermobility is a real clinical problem in approximately 80 percent of patients with first ray disorders, such as bunions, flat feet, hammertoes and forefoot overload,” says Neal Blitz, DPM, FACFAS.
Dr. Blitz, who is in private practice in New York City, thinks the reason there continues to be controversy regarding the existence of hypermobility is because not all hypermobility is pathologic. He says since foot and ankle surgeons see people with problematic feet, the implications of hypermobility on a foot without problems are unknown.
What the profession does know, says Dr. Blitz, is that treating hypermobility related disorders by addressing the hypermobility can result in resolution of the patient’s particular foot problem. He cites the example of patients with a large bunion, hypermobility and sub-second metatarsalgia. One would correct this problem with first ray surgery only (via a Lapidus procedure or realignment osteotomy) and the sub-second metatarsalgia resolves.
In regard to the literature, the incidence of hypermobility with hallux valgus is reportedly rare with Scher and colleagues estimating its prevalence at 0.06 per 1,000 person years in a study in Clinical Orthopedics and Related Research. In a study of 122 feet in 103 patients with moderate to severe hallux valgus in the Journal of Bone and Joint Surgery, Coughlin and Jones noted hypermobility in 23 feet preoperatively and this number reduced to two feet postoperatively. In their comparison of long-term results for the Hohmann procedure and the Lapidus bunionectomy for the treatment of hallux valgus in 101 feet, Faber and colleagues in the Bone and Joint Journal concluded that the presence or absence of first ray hypermobility makes no difference to the outcomes.
Although much research has focused on the definition, contribution to pathology and surgical correction of hypermobility, Thomas Roukis, DPM, PhD, FACFAS, in February told the attendees of the American College of Foot and Ankle Surgeons (ACFAS) Scientific Conference that it remains a poorly understood condition. In his ACFAS lecture, “Hypermobility: Let’s Put this Controversy to Rest,” Dr. Roukis noted there is no consensus for hypermobility’s definition or clinical evaluation, no proven causation with pathology and no meaningful influence on surgical procedure selection. To date, Dr. Roukis, a Past President of the ACFAS, says research has proven little about hypermobility and its role in first ray pathology.
For further reading, download the supplement “Highlights From The 2016 Scientific Conference of the American College of Foot and Ankle Surgeons” at https://tinyurl.com/z5nllne or check out the article “Emerging Insights On First Ray Hypermobility” in the December 2015 issue of Podiatry Today.
What A Recent Study Reveals About Drug-Drug Interactions
By Brian McCurdy, Managing Editor
About 15 percent of older adults are at risk for a drug-drug interaction, according to a recent study in the Journal of the American Medical Association Internal Medicine.
In the study, researchers looked at a longitudinal, nationally representative sample of community-dwelling older adults ages 62 to 85. The study focused on 2,351 participants in 2005-2006 and 2,206 people in 2010-2011. The study notes the use of at least one prescription medication slightly increased from 84.1 percent in 2005-2006 to 87.7 percent in 2010-2011. In addition, the concurrent use of at least five prescription medications increased from 30.6 percent to 35.8 percent. Improving safety with the use of multiple medications has the potential to reduce preventable adverse drug events associated with medications in common use among the elderly, according to the study.
 Robert Smith, DPM, MSc, RPh, CPed, outlines several strategies for avoiding drug-drug interactions. First, he emphasizes obtaining a detailed history of patient medication history before choosing a pharmacologic intervention. Dr. Smith advises not adding a drug with a potential for interaction or an agent associated with serious adverse events. If possible, clinicians should delaying initiation of potentially interacting drugs until the patient’s primary therapy is complete, advises Dr. Smith, who is in private practice at Shoe String Podiatry in Ormond Beach, Fla., and is currently deployed in Iraq.
Robert Smith, DPM, MSc, RPh, CPed, outlines several strategies for avoiding drug-drug interactions. First, he emphasizes obtaining a detailed history of patient medication history before choosing a pharmacologic intervention. Dr. Smith advises not adding a drug with a potential for interaction or an agent associated with serious adverse events. If possible, clinicians should delaying initiation of potentially interacting drugs until the patient’s primary therapy is complete, advises Dr. Smith, who is in private practice at Shoe String Podiatry in Ormond Beach, Fla., and is currently deployed in Iraq.
Dr. Smith suggests considering concomitant disease states like organ dysfunction, liver or kidney disease. He also advises using the smallest effective drug dose and not overestimating the ability of patients to adhere to recommended dosing schedules.
Citing information from the World Health Organization, Dr. Smith suggests choosing an appropriate medication for a given clinical situation while considering individual patient factors like allergies; selecting an appropriate administration route, dosing and regimen; and ensuring communication of the plan with the patient’s primary care provider and his or her other relevant healthcare providers.
Is An Emerging Allograft Effective In Diabetic Foot Ulcers?
By Brian McCurdy, Managing Editor
Recent data suggests that cryopreserved amniotic membrane and umbilical cord may facilitate quicker healing of chronic DFUs.
 The study, presented at Superbones Superwounds East 2016, was a retrospective review of 29 patients with 32 diabetic foot ulcers. All wounds had debridement prior to the application of Neox Wound Allograft (Amniox Medical). The study noted complete healing of 28 wounds for an 87.5 percent average healing rate. According to the study results, the initial wound area was an average of 10.6 cm2 and the average time to healing was 13.79 weeks.
The study, presented at Superbones Superwounds East 2016, was a retrospective review of 29 patients with 32 diabetic foot ulcers. All wounds had debridement prior to the application of Neox Wound Allograft (Amniox Medical). The study noted complete healing of 28 wounds for an 87.5 percent average healing rate. According to the study results, the initial wound area was an average of 10.6 cm2 and the average time to healing was 13.79 weeks.
Allen Raphael, DPM, the lead author of the study, has found Neox to be advantageous when the faulty biology of a chronic wound has created a lack of progression in the healing cascade. When one applies the graft to chronically injured tissues, he notes the graft has the capacity to regenerate better quality granulation while modulating inflammation.
Typically, Dr. Raphael will intervene and graft a wound with Neox fairly early in the process. After about four weeks, if a wound does not show greater than 50 percent healing, it is time to move to an advanced treatment modality, notes Dr. Raphael, who is in private practice at Village Podiatry Centers in Smyrna, Ga.
Dr. Raphael says one can use the graft in conjunction with negative pressure wound therapy to accelerate wound healing. In addition, he has found that subcutaneous implantation in wounds is an effective option for tissue augmentation.











