Does The Evidence Support Traditional Concepts Of Achilles Tendon Rupture Etiology And Repair?
 The approach to the evaluation and management of acute Achilles tendon rupture has experienced a constant evolution over the past five decades. Both surgical and non-surgical treatments have had extensive study, and a wealth of new evidence is available that has changed the most basic tenets of management of this common injury.
The approach to the evaluation and management of acute Achilles tendon rupture has experienced a constant evolution over the past five decades. Both surgical and non-surgical treatments have had extensive study, and a wealth of new evidence is available that has changed the most basic tenets of management of this common injury.
Despite the availability of very good studies that clarify and challenge our traditional thoughts, many traditions and misconceptions persist among foot and ankle surgeons. We will explore several aspects of acute Achilles tendon rupture including: whether repair is needed for good outcomes, current concepts of tendon hemodynamics and ischemia, and which steps in the repair algorithm are necessary.
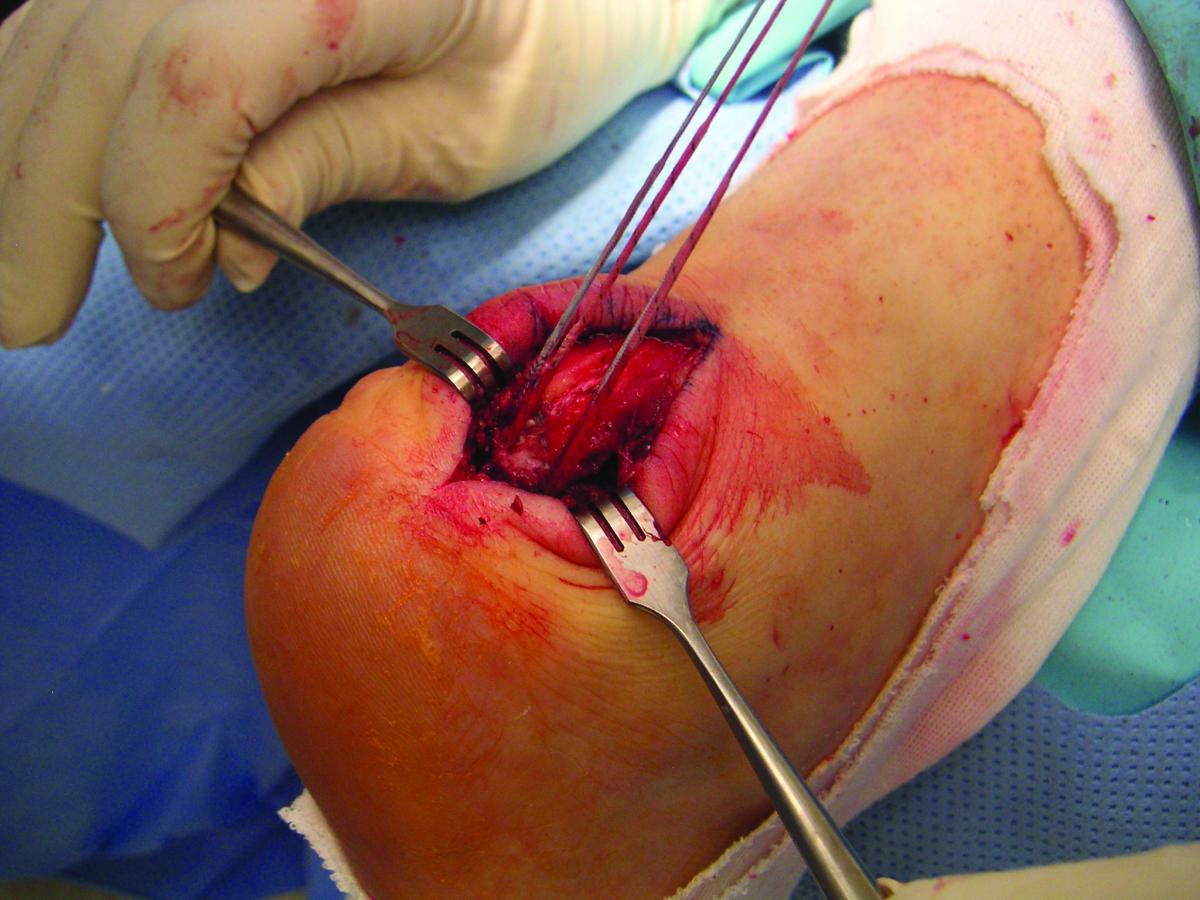
To start the discussion, we will first explore the concept of tendon debridement during repair. This commonly recommended step highlights how historic evidence can create a bias in our approach to a common medical problem and how this bias can persist for decades despite the emergence of new evidence. The surgical repair of acute Achilles tendon ruptures commonly includes debridement of damaged tendon fibrils or “mop ends” at the rupture site.
Although we have historically seen debridement as necessary in the repair algorithm, we question whether it is necessary or prudent to resect any portion of the ruptured tendon. Removal of even a small segment of the midportion of the Achilles tendon results in shortening of the muscle-tendon unit and subsequent iatrogenic equinus.
In order to critically assess the common practice of tendon debridement in Achilles tendon ruptures, we must first answer the following questions:
1. What evidence supports the surgical resection of any portion of the damaged tendon?
2. How do we determine which portion of the tendon is beyond the capability for natural biologic repair?
3. Is ischemia the proximate cause of Achilles tendon rupture?
4. Has this notion of midsubstance ischemia of the Achilles led to the recommendation of debridement because we think this section of tendon is necrotic?
Addressing Ischemia And Vascularity In Achilles Tendon Ruptures
Although the notion of ischemia as the main etiology of Achilles rupture is ubiquitous in the discussion of the condition, there is little to no experimental evidence to support this conclusion.
The original study by Lagergren and Lindholm in 1959 used a cadaver model and mapped the blood supply with standard anatomic latex injection technique.1 The authors ascribed the term “watershed” to the vascular anatomy of the tendon because there were vascular components that came from both proximal and distal portions of the tendon, similar to the geographic term of a river watershed. They concluded that this anatomic distribution and orientation of blood supply leads to ischemia in the midsubstance of the tendon. Carr and Norris duplicated this experiment with the same conclusion in 1989.2
It is interesting that this notion of avascularity has persisted for many decades based on mapping of the static arterial anatomy in cadavers alone and not hemodynamic flow studies in live patients. Recent literature questions the concept of avascularity as a significant or sole factor for Achilles tendon tears.3 With the use of quantitative laser Doppler flowmetry, Astrom in 2000 and Astrom and Westlin in 1994 found that the midsection and origin are the areas of the Achilles tendon that are the most vascularized uniformly along the tendon, and that only the distal insertion has noticeably lower blood flow.4,5
 Using a sodium washout, Hastad and colleagues showed there is a decrease in blood flow in all zones as we age, but the blood flow is consistent along the longitudinal course of the tendon.6 Astrom confirmed the uniformity of blood flow.4 Further evidence highlights a uniform increase in tendon blood flow to the Achilles tendon throughout its length.7–10
Using a sodium washout, Hastad and colleagues showed there is a decrease in blood flow in all zones as we age, but the blood flow is consistent along the longitudinal course of the tendon.6 Astrom confirmed the uniformity of blood flow.4 Further evidence highlights a uniform increase in tendon blood flow to the Achilles tendon throughout its length.7–10
We wonder if this notion of ischemia, which began with non-hemodynamic cadaver studies, coupled with the visual cues we see during exposure for acute repair, including hematoma and tendon fragmentation, has led us down the path of resection of a portion of the tendon without scientific cause. Let’s face it. The tendon at the rupture site looks bad when we directly visualize it. If we are biased by what we learned about “watershed ischemia,” debridement seems reasonable.
What The Literature Says About Non-Operative Achilles Care
A somewhat less direct approach to answer the question of whether the tendon is ischemic is to examine the results of non-surgical care for Achilles tendon ruptures. A growing number of recent studies indicate that the functional outcomes and re-rupture rates for non-surgical management using early functional rehabilitation are equivalent to surgical repair.
A 2017 Canadian study by Sheth and colleagues detailed that, although there has been a rise in acute Achilles tendon ruptures in recent years, there has been a significant decrease in the incidence of surgical repairs since 2009.11 The authors found that the rate of surgical repairs in Ontario, Canada dropped from 20.1 percent in 2003 to 9.2 percent in 2013.
This drop in surgical repairs in Canada could have contributed to recent literature that supports non-operative treatment. In a 2017 systematic review and meta-analysis, Deng and coworkers found no statistically significant difference in the incidence of deep vein thrombosis (DVT), functional scores or ankle range of motion (ROM) between the surgical and non-surgical groups.12 The authors also showed that the re-rupture rate for surgical patients of 3.7 percent was statistically lower than that of the non-surgical group (9.8 percent).
Twaddle and Poon previously explained the prevention of this increased rate of re-rupture in non-surgical patients in 2007.13 The authors observed surgical and non-operative patients who both partook in early range of motion, and found no significant difference in complications, re-rupture rates, dorsiflexion, plantarflexion, calf size or the Musculoskeletal Function Assessment index between the two groups. Lim and Gwynne-Jones also found no significant difference in Achilles tendon total rupture scores between operative and non-operative treatment groups that followed the same functional bracing protocol.14 Thus, Twaddle, Lim and and their respective colleagues concluded, as did Barfod and colleagues in 2014, that early active rehabilitation is more important for tendon healing than surgery.13–15
 Comparing Achilles tendon repair patients in early weightbearing and six-week delayed weightbearing groups, Suchak and colleagues found the early weightbearing group had better RAND-36 and ROM outcomes at six weeks.16 At six months, there was no longer this difference between the two groups and patients had the same complication rate. Young and coworkers achieved this early active rehabilitation by allowing non-operative patients to use weightbearing casts, and these patients had outcomes equivalent to non-operative patients who were non-weightbearing.17
Comparing Achilles tendon repair patients in early weightbearing and six-week delayed weightbearing groups, Suchak and colleagues found the early weightbearing group had better RAND-36 and ROM outcomes at six weeks.16 At six months, there was no longer this difference between the two groups and patients had the same complication rate. Young and coworkers achieved this early active rehabilitation by allowing non-operative patients to use weightbearing casts, and these patients had outcomes equivalent to non-operative patients who were non-weightbearing.17
Hutchison and colleagues noted low re-rupture rates (1.1 percent) and satisfactory Achilles Tendon Total Rupture Score, Achilles Tendon Repair Score and functional outcomes when using the Swansea Morriston Achilles Rupture Treatment program (SMART), which includes early weightbearing.18 A Level I study by Willits and coworkers “supports accelerated functional rehabilitation and nonoperative treatment for acute Achilles tendon ruptures” due to the patients having similar clinical outcomes as operative patients while avoiding the complications associated with surgery.19 Bergkvist and colleagues agreed that non-operative treatment is the preferred protocol in most patients with acute Achilles tendon rupture due to a low re-rupture rate (6.6 percent) in non-surgical patients and the nonexistent chance of infection.20
It would stand to reason that if the tendon can heal without surgery, it must not be significantly ischemic and is certainly not dead. In fact, the Achilles is just injured and experiences the normal physiologic reparative process as with any similar tissue failure. Additionally, limited exposure or percutaneous techniques for repair are now available and provide encouraging results.21–23 These techniques do not include any form of tendon debridement, further supporting the concept that the damaged, but not necessarily ischemic, tendon can heal through normal physiologic processes.
Final Words
While open surgical debridement may have been the standard treatment of acute Achilles tendon ruptures in the past, that does not mean that it is the gold standard of patient care now. Numerous studies have shown there is sufficient blood flow along the length of the tendon. Therefore, there is no ischemia and no need to debride the tendon. This point is further supported by the knowledge that Achilles ruptures may heal non-operatively with excellent functional results and low complications. As the research shows, the new standard in care is setting down the blade, taking a break from the OR and having your patients with Achilles tendon ruptures start early weightbearing and ROM.
Dr. Dayton is affiliated with UnityPoint Clinic Foot and Ankle in Fort Dodge, Iowa. He is an Assistant Professor in the College of Podiatric Medicine and Surgery at Des Moines University. Dr. Dayton is a Fellow of the American College of Foot and Ankle Surgeons.
Dr. Harper is affiliated with UnityPoint Clinic Foot and Ankle in Fort Dodge, Iowa.
Ms. Egdorf is a third-year podiatric medical student with the College of Podiatric Medicine and Surgery at Des Moines University.
Ms. Cifaldi is a third-year podiatric medical student with the College of Podiatric Medicine and Surgery at Des Moines University.
References
- Lagergren C, Lindholm A. Vascular distribution in the Achilles tendon; an angiographic and microangiographic study. Acta Chir Scand. 1959;116(5-6):491-495.
- Carr AJ, Norris SH. The blood supply of the calcaneal tendon. J Bone Joint Surg Br. 1989;71(1):100-101.
- Theobald P, Benjamin M, Nokes L, Pugh N. Review of the vascularisation of the human Achilles tendon. Injury. 2005;36(11):1267-1272.
- Aström M. Laser Doppler flowmetry in the assessment of tendon blood flow. Scand J Med Sci Sports. 2000;10(6):365-367.
- Aström M, Westlin N. Blood flow in chronic Achilles tendinopathy. Clin Orthop Relat Res. 1994(308):166-172.
- Hastad K, Larsson LG, Lindholm A. Clearance of radiosodium after local deposit in the Achilles tendon. Acta Chir Scand. 1959;116(3):251-255.
- Langberg H, Olesen J, Skovgaard D, Kjaer M. Age related blood flow around the Achilles tendon during exercise in humans. Eur J Appl Physiol. 2001;84(3):246-248.
- Langberg H, Bülow J, Kjaer M. Blood flow in the peritendinous space of the human Achilles tendon during exercise. Acta Physiol Scand. 1998;163(2):149-153.
- Boushel R, Langberg H, Green S, Skovgaard D, Bulow J, Kjaer M. Blood flow and oxygenation in peritendinous tissue and calf muscle during dynamic exercise in humans. J Physiol (Lond). 2000;524 Pt 1:305-313.
- Kubo K, Ikebukuro T, Tsunoda N, Kanehisa H. Changes in oxygen consumption of human muscle and tendon following repeat muscle contractions. Eur J Appl Physiol. 2008;104(5):859-866.
- Sheth U, Wasserstein D, Jenkinson R, Moineddin R, Kreder H, Jaglal SB. The epidemiology and trends in management of acute Achilles tendon ruptures in Ontario, Canada: a population-based study of 27,607 patients. Bone Joint J. 2017;99-B(1):78-86.
- Deng S, Sun Z, Zhang C, Chen G, Li J. Surgical treatment versus conservative management for acute Achilles tendon rupture: a systematic review and meta-analysis of randomized controlled trials. J Foot Ankle Surg. 2017;56(6):1236-1243.
- Twaddle BC, Poon P. Early motion for Achilles tendon ruptures: is surgery important? A randomized, prospective study. Am J Sports Med. 2007;35(12):2033-2038.
- Lim CS, Lees D, Gwynne-Jones DP. Functional outcome of acute Achilles tendon rupture with and without operative treatment using identical functional bracing protocol. Foot Ankle Int. 2017;38(12):1331-1336.
- Barfod KW, Bencke J, Lauridsen HB, Ban I, Ebskov L, Troelsen A. Nonoperative dynamic treatment of acute Achilles tendon rupture: the influence of early weight-bearing on clinical outcome: a blinded, randomized controlled trial. J Bone Joint Surg Am. 2014;96(18):1497-1503.
- Suchak AA, Bostick GP, Beaupre LA, Durand DC, Jomha NM. The influence of early weightbearing compared with non-weightbearing after surgical repair of the Achilles tendon. J Bone Joint Surg Am. 2008; 90(9):1876–83.
- Young SW, Patel A, Zhu M, et al. Weight-bearing in the nonoperative treatment of acute Achilles tendon ruptures: a randomized controlled trial. J Bone Joint Surg Am. 2014;96(13):1073-1079. Accessed Feb 11, 2018.
- Hutchison AM, Topliss C, Beard D, Evans RM, Williams P. The treatment of a rupture of the Achilles tendon using a dedicated management programme. Bone Joint J. 2015;97-B(4):510-515.
- Willits K, Amendola A, Bryant D, et al. Operative versus nonoperative treatment of acute Achilles tendon ruptures: a multicenter randomized trial using accelerated functional rehabilitation. J Bone Joint Surg Am. 2010;92(17):2767-2775.
- Bergkvist D, Astrom I, Josefsson PO, Dahlberg LE. Acute Achilles tendon rupture: a questionnaire follow-up of 487 patients. J Bone Joint Surg Am. 2012; 94(13):1229–33.
- Chiu C, Yeh W, Tsai M, Chang S, Hsu K, Chan Y. Endoscopy-assisted percutaneous repair of acute Achilles tendon tears. Foot Ankle Int. 2013;34(8):1168-1176.
- Karabinas PK, Benetos IS, Lampropoulou-Adamidou K, Romoudis P, Mavrogenis AF, Vlamis J. Percutaneous versus open repair of acute Achilles tendon ruptures. Eur J Orthop Surg Traumatol. 2014;24(4):607-613.
- Hsu AR, Jones CP, Cohen BE, Davis WH, Ellington JK, Anderson RB. Clinical outcomes and complications of percutaneous Achilles repair system versus open technique for acute Achilles tendon ruptures. Foot Ankle Int. 2015;36(11):1279-1286.











